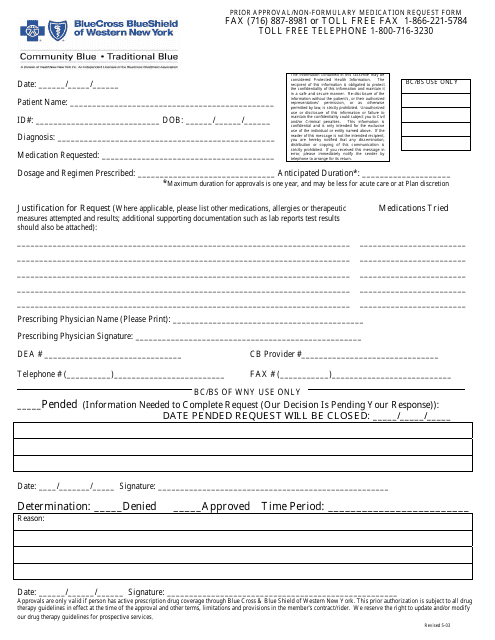
Blue Cross Blue Shield Prior Authorization Form Templates
Blue Cross Blue Shield Prior Authorization Forms are used to request approval for medications that are not part of the insurer's formulary (list of covered medications) or require prior authorization. The form allows healthcare providers to provide detailed information about why a specific medication is necessary in order to receive approval from the insurance company. This helps ensure that the medication is appropriate, medically necessary, and will be covered by the insurance plan.
Documents:
1
This document is used for requesting approval for medications that are not included in the preferred formulary of Blue Cross Blue Shield of Western New York.