Soap Note Templates
Soap Note Templates are used for documenting patient encounters in the healthcare field, specifically by healthcare providers such as doctors, nurses, therapists, and other medical professionals. The term "SOAP" stands for Subjective, Objective, Assessment, and Plan, which are the four main components of the note. These templates provide a structured format for healthcare professionals to record important information about the patient's symptoms, physical examination findings, assessments, and treatment plans. The Soap Note Templates help ensure consistency and accuracy in documenting patient care, facilitating communication between healthcare providers, improving continuity of care, and serving as a legal record of the patient's healthcare journey.
Documents:
5
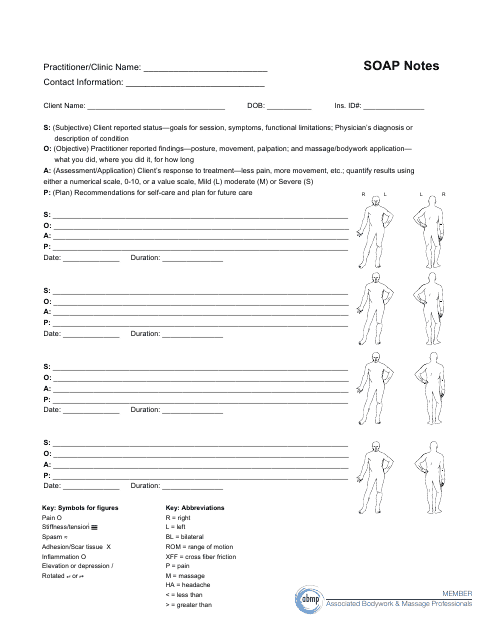
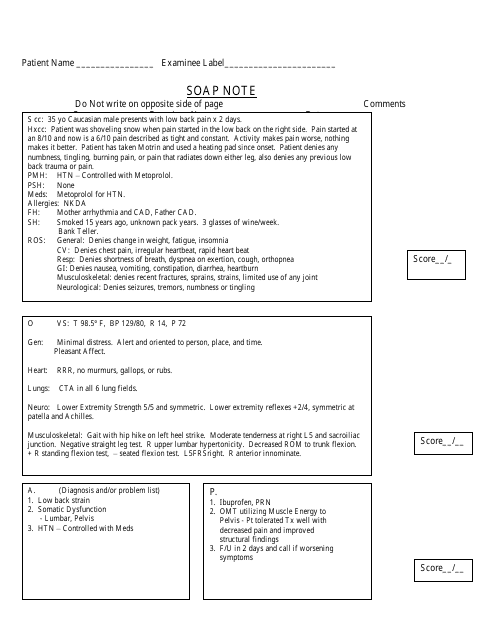
This document is a template for recording SOAP notes, which are a standard format used by massage therapists and other healthcare professionals to document client sessions. SOAP stands for Subjective, Objective, Assessment, and Plan, and these notes help track a client's progress and guide future treatment.
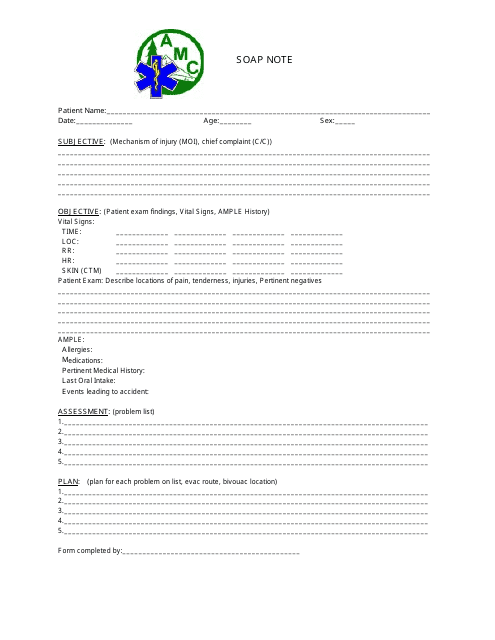
This document is a Soap Note Template used by healthcare professionals at the AMC. A Soap Note is a method of documenting patient encounters in a structured format, including subjective, objective, assessment, and plan. This template helps healthcare providers organize and record important patient information.
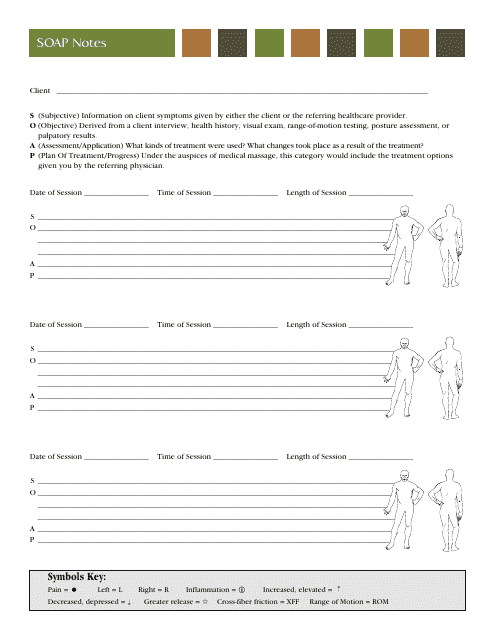
This document is a Soap Notes Template used by healthcare providers to record patient information, including subjective, objective, assessment, and plan for treatment.
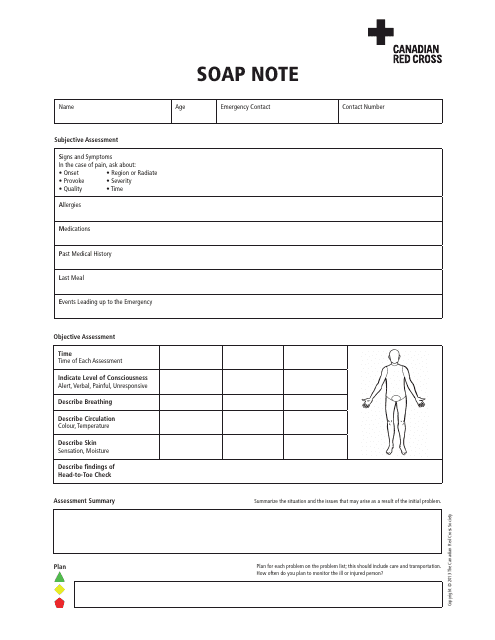
This document is a Soap Note Template provided by the Canadian Red Cross. It is used for organizing and recording patient information in a structured format.
This type of document is a Soap Note, which is a method used by healthcare professionals to document patient information, including subjective and objective observations, assessment, and plan for treatment. It is used to keep a record of a patient's medical history and progress throughout their treatment.