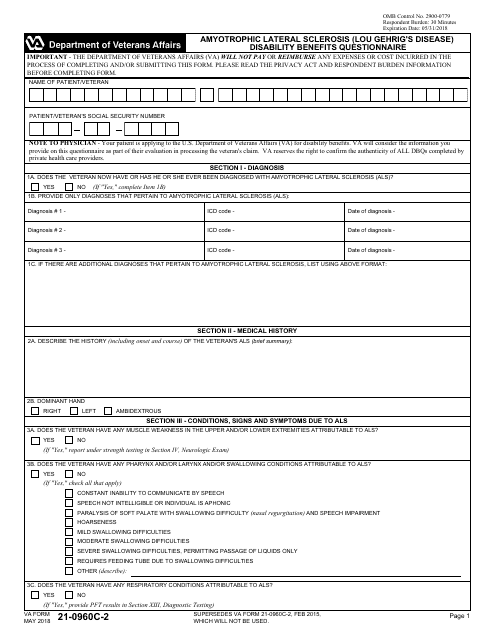
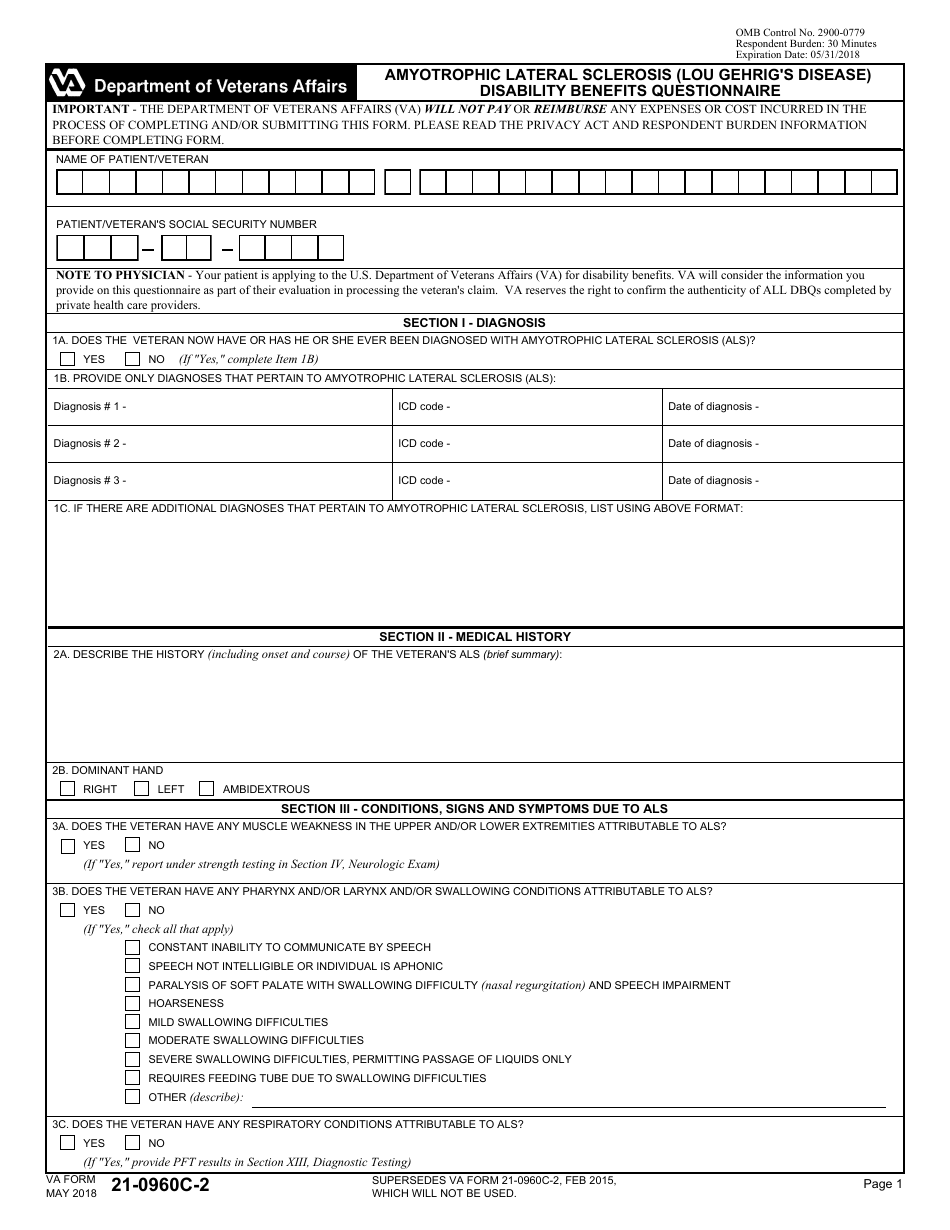
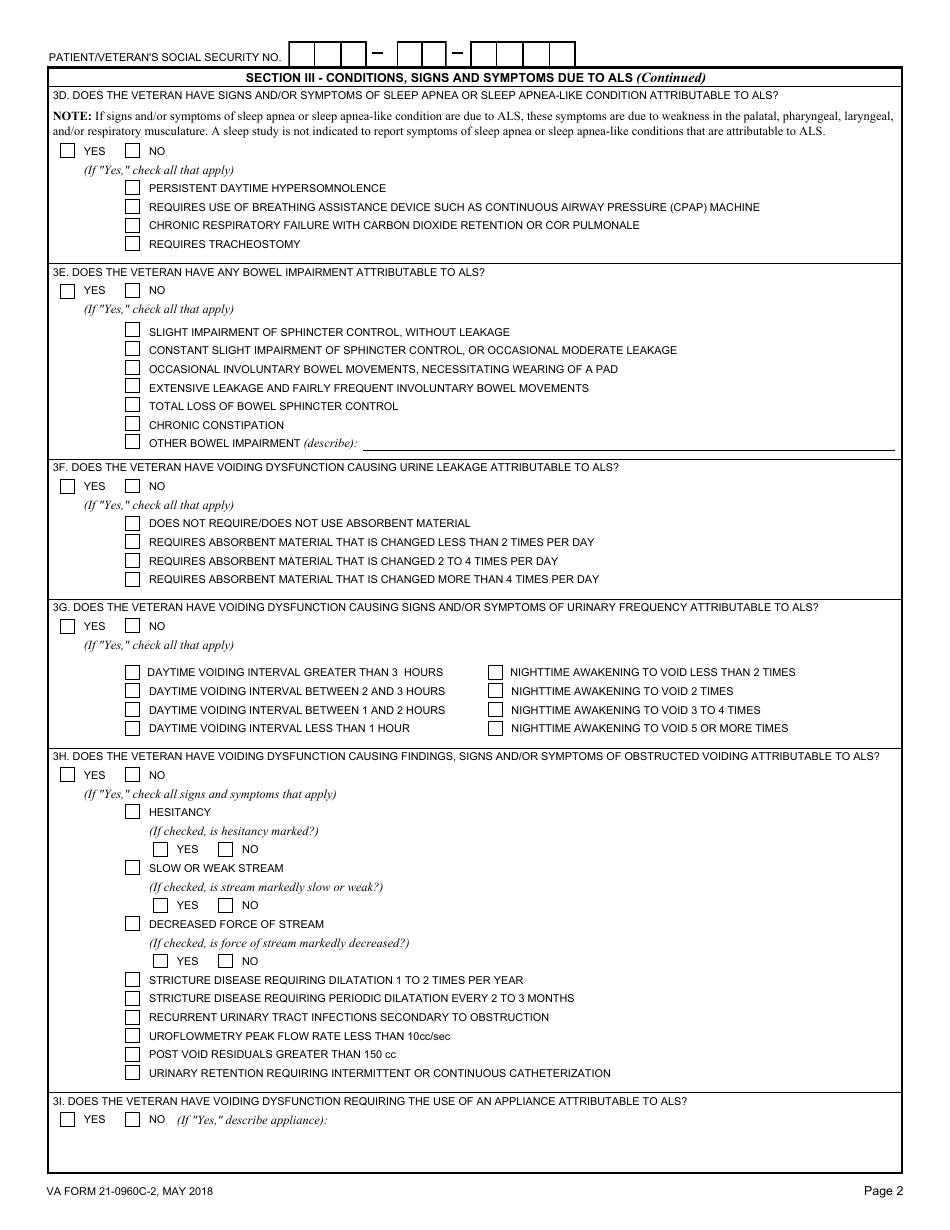
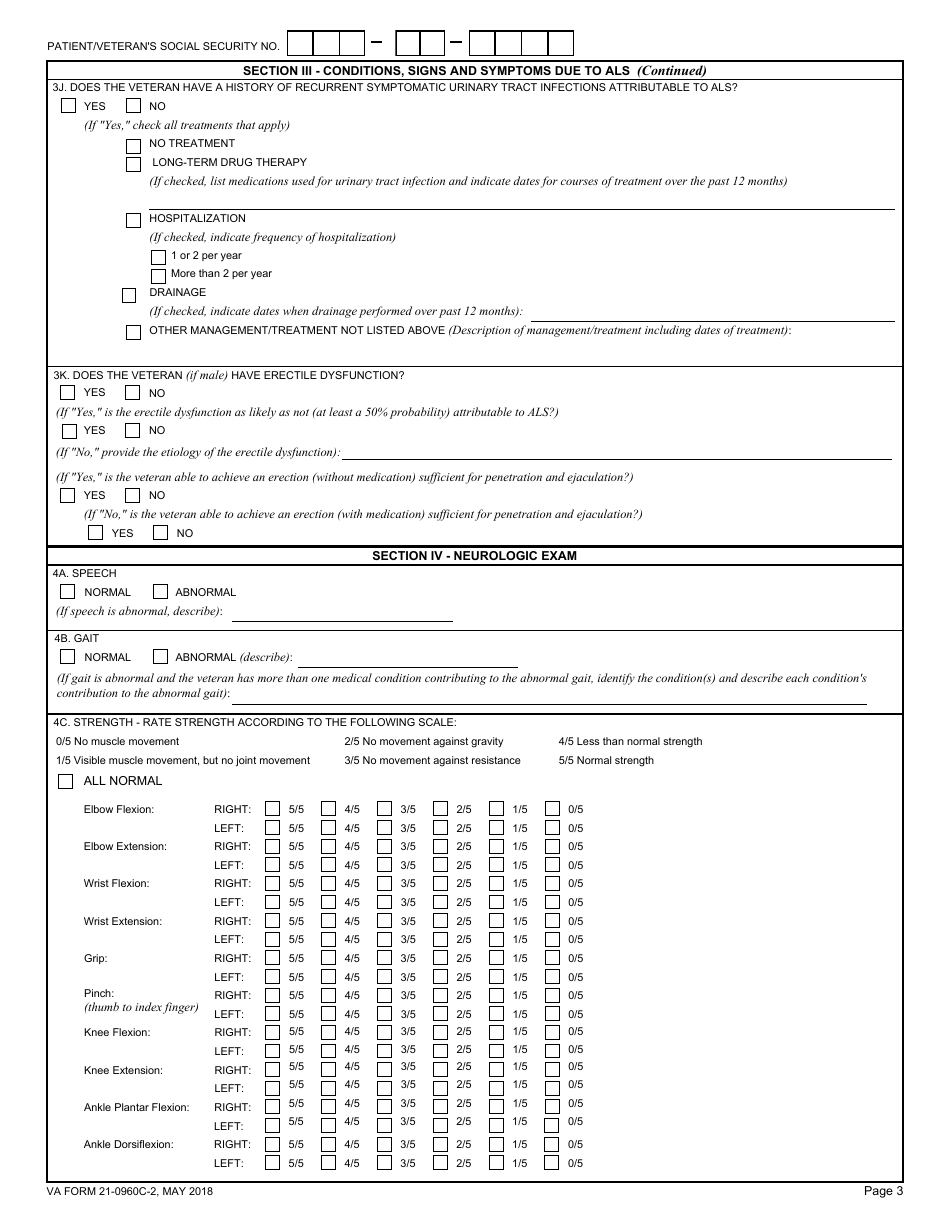
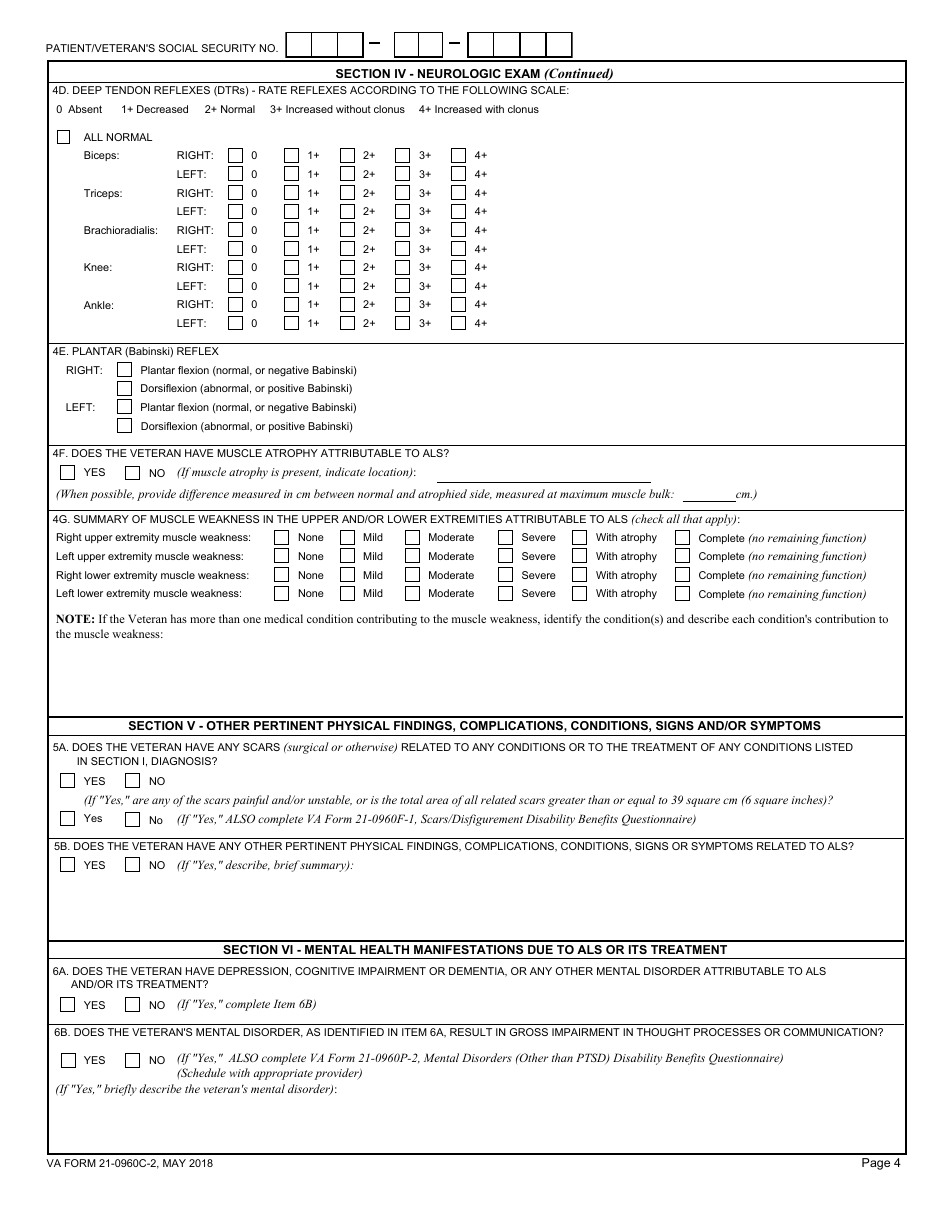
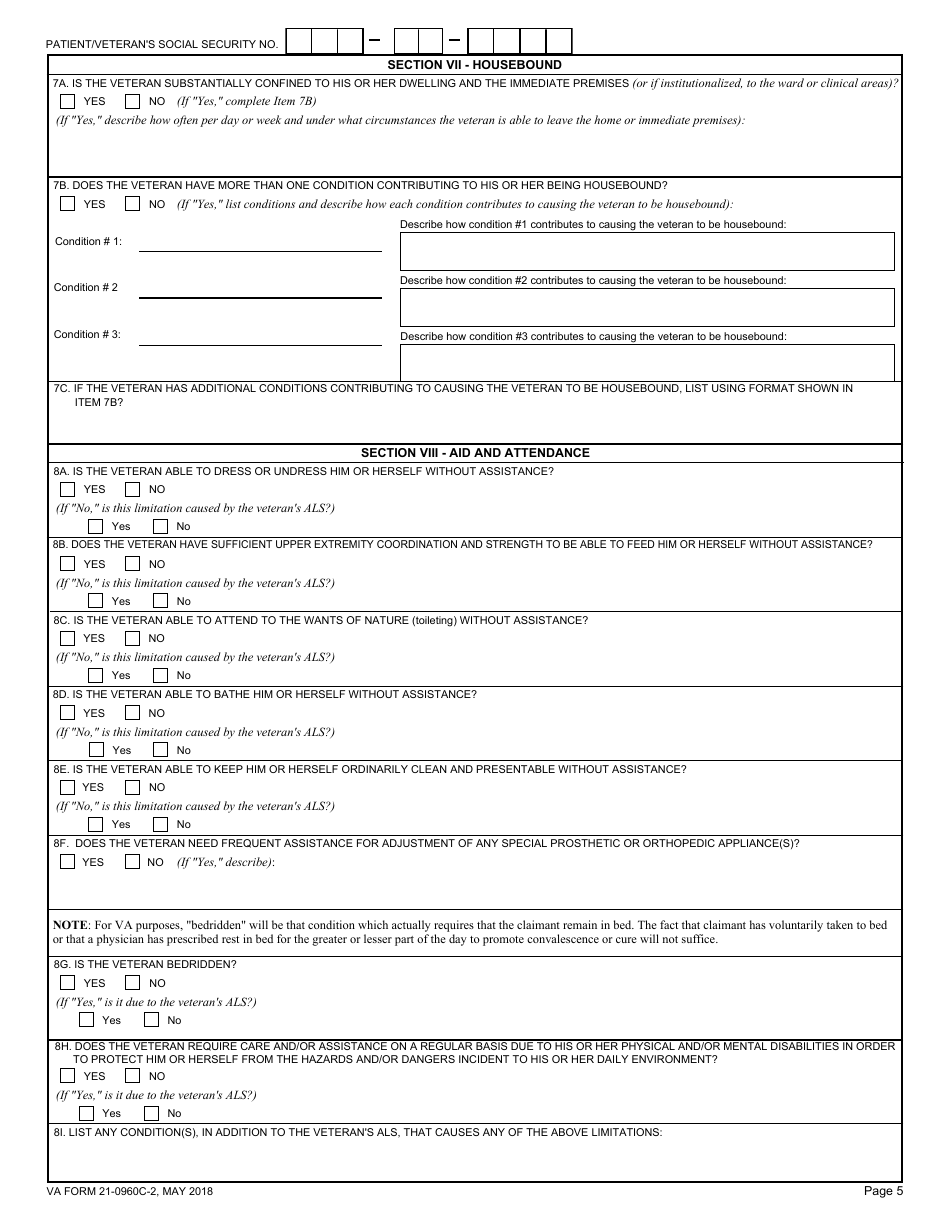
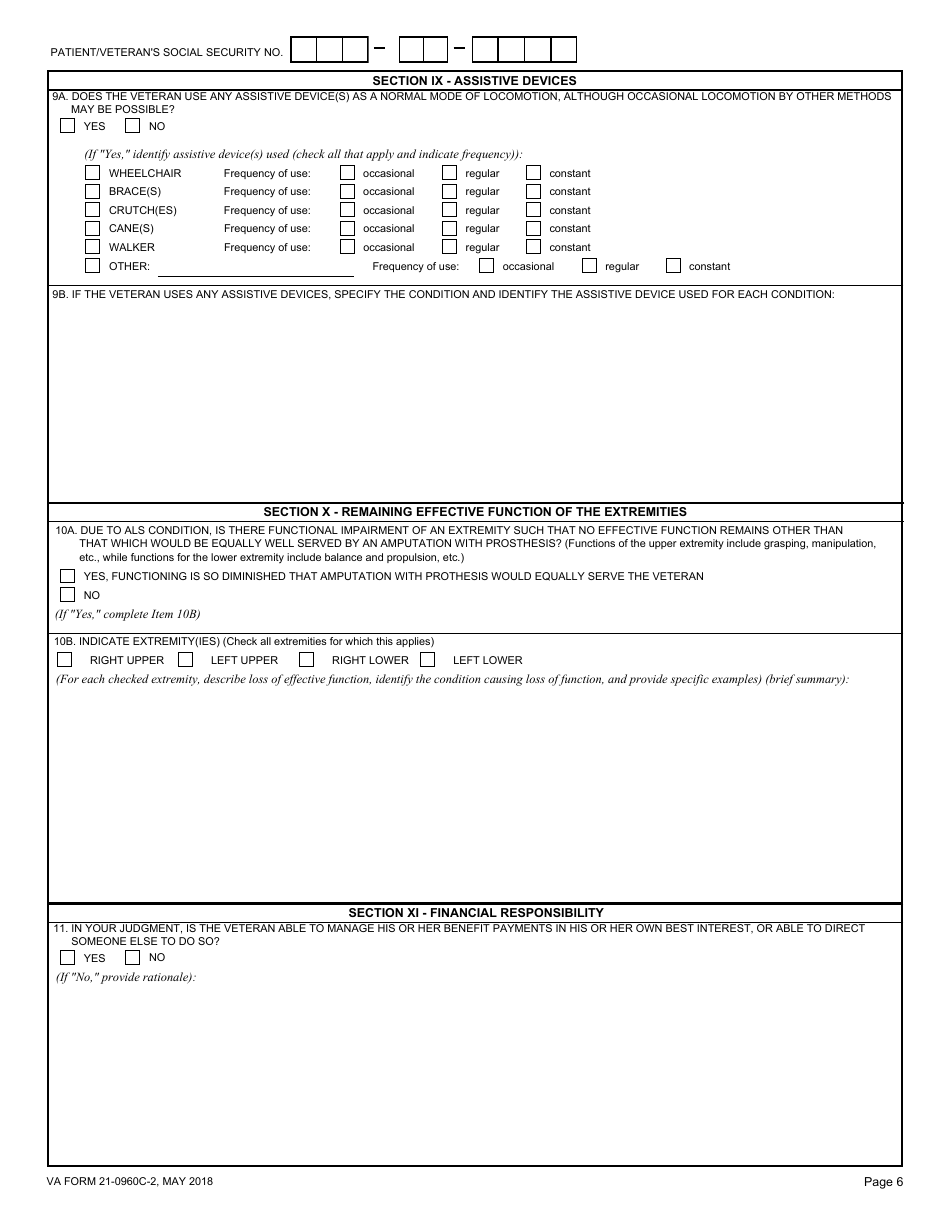
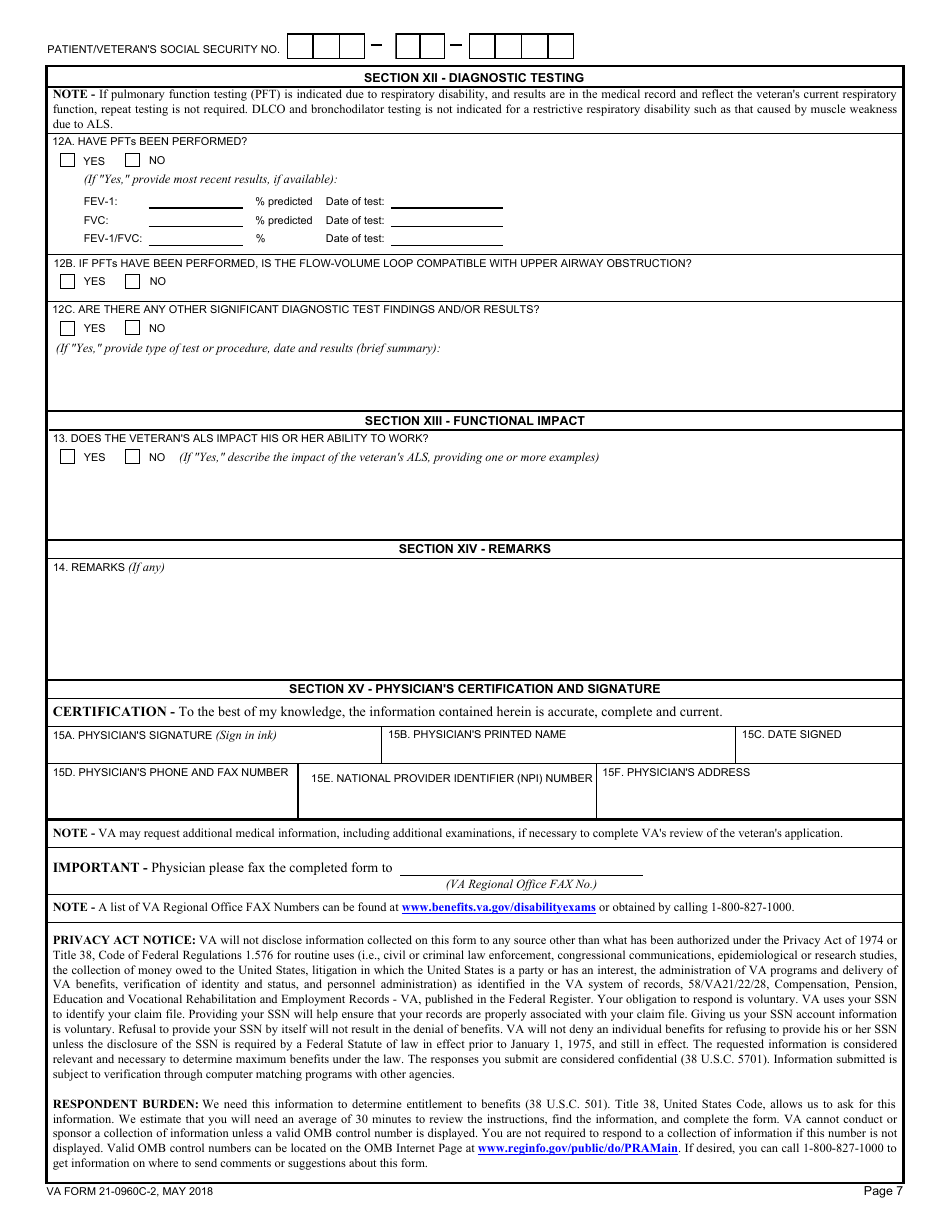
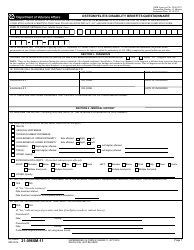
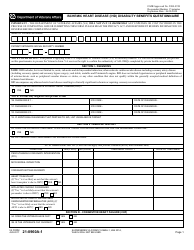
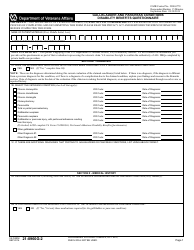
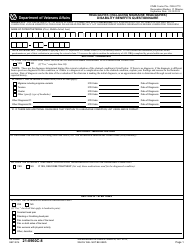
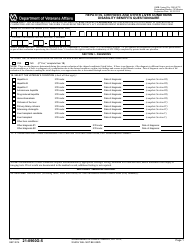
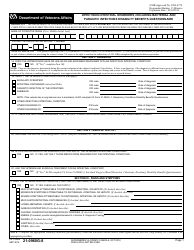
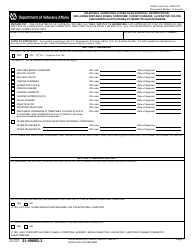
VA Form 21-0960C-2 Amyotrophic Lateral Sclerosis (Lou Gehrig's Disease) Disability Benefits Questionnaire
What Is VA Form 21-0960C-2?
This is a legal form that was released by the U.S. Department of Veterans Affairs on May 1, 2018 and used country-wide. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is VA Form 21-0960C-2?
A: VA Form 21-0960C-2 is a form used to evaluate disability benefits for Amyotrophic Lateral Sclerosis (ALS) or Lou Gehrig's Disease.
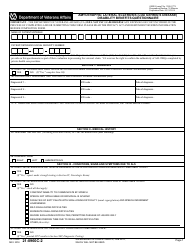
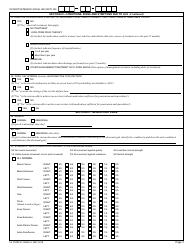
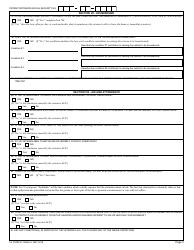
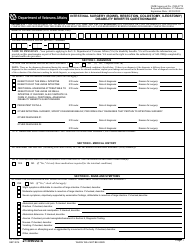
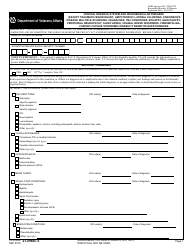
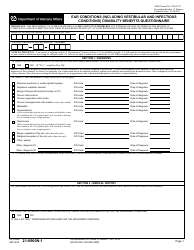
Q: What does the form evaluate?
A: The form evaluates the impact of ALS on an individual's ability to function.
Q: Who can use this form?
A: Veterans with a diagnosis of ALS who are applying for disability benefits.
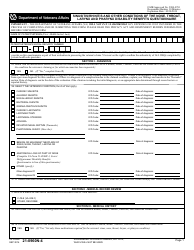
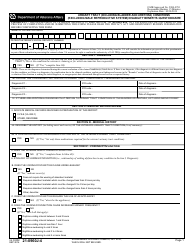
Q: What information is required on the form?
A: The form requires information about medical history, symptoms, treatment, and functional limitations.
Q: How long does it take to complete the form?
A: The time required to complete the form varies depending on individual circumstances.
Q: Are there any supporting documents required?
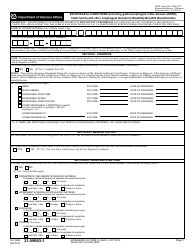
A: Yes, supporting medical evidence such as doctor's notes and test results should be submitted along with the form.
Q: What should I do after completing the form?
A: After completing the form, you should submit it to the VA along with the supporting documents.
Q: How long does it take to receive a decision on disability benefits?
A: The processing time for disability benefits applications can vary, but it typically takes several months.
Q: Can I appeal if my application is denied?
A: Yes, if your application is denied, you have the right to appeal the decision.
Form Details:
- Released on May 1, 2018;
- The latest available edition released by the U.S. Department of Veterans Affairs;
- Easy to use and ready to print;
- Yours to fill out and keep for your records;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of VA Form 21-0960C-2 by clicking the link below or browse more documents and templates provided by the U.S. Department of Veterans Affairs.