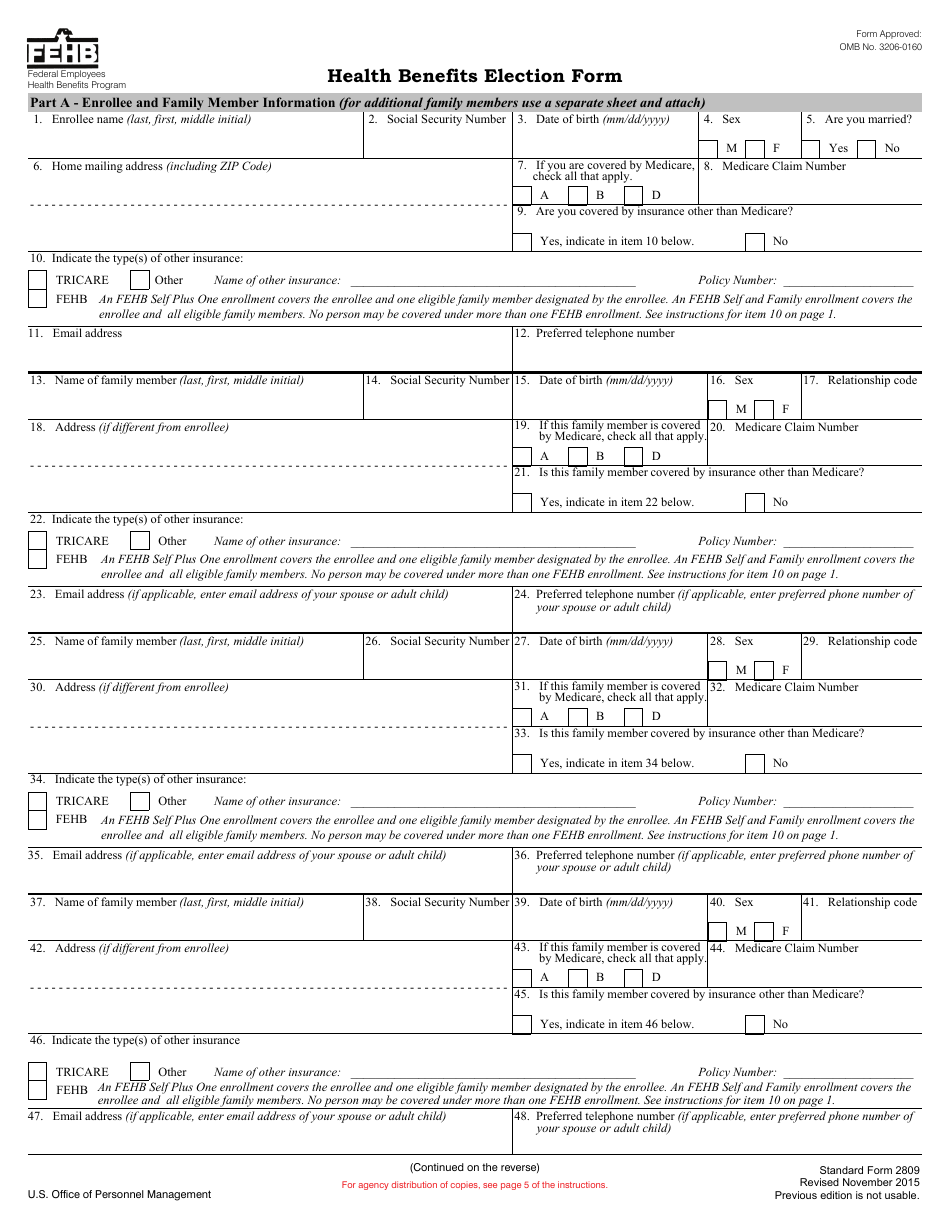
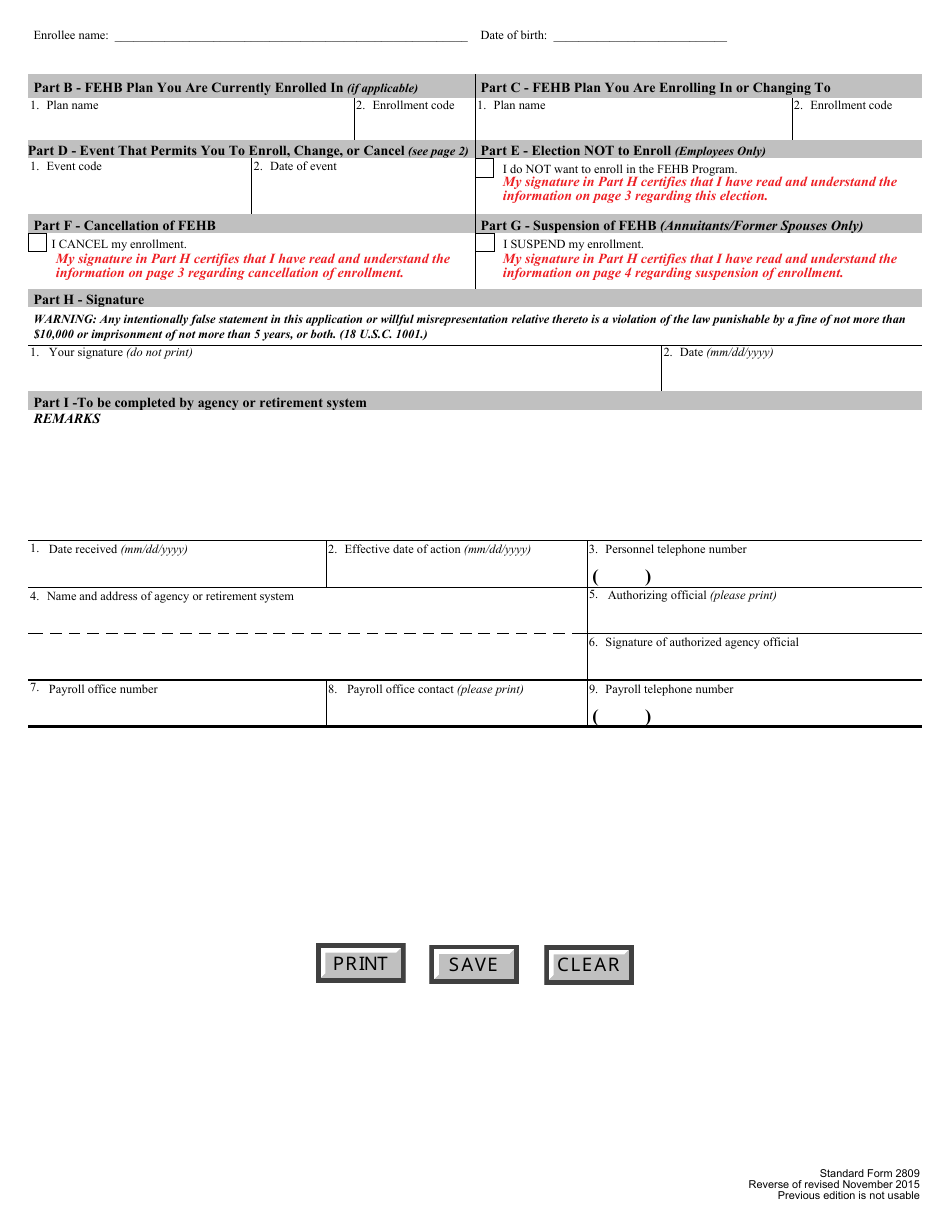
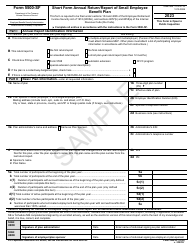
This version of the form is not currently in use and is provided for reference only. Download this version of
Form SF-2809
for the current year.
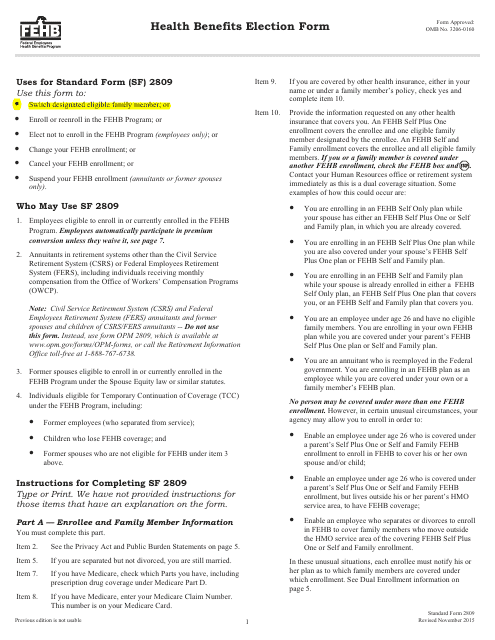
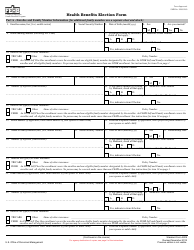
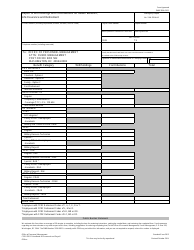
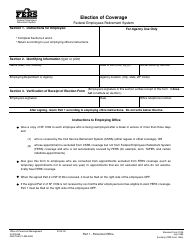
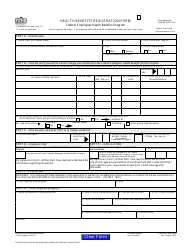
Form SF-2809 Employee Health Benefits Registration Form
What Is OPM Form SF-2809?
This is a legal form that was released by the U.S. Office of Personnel Management on November 1, 2015 and used country-wide. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
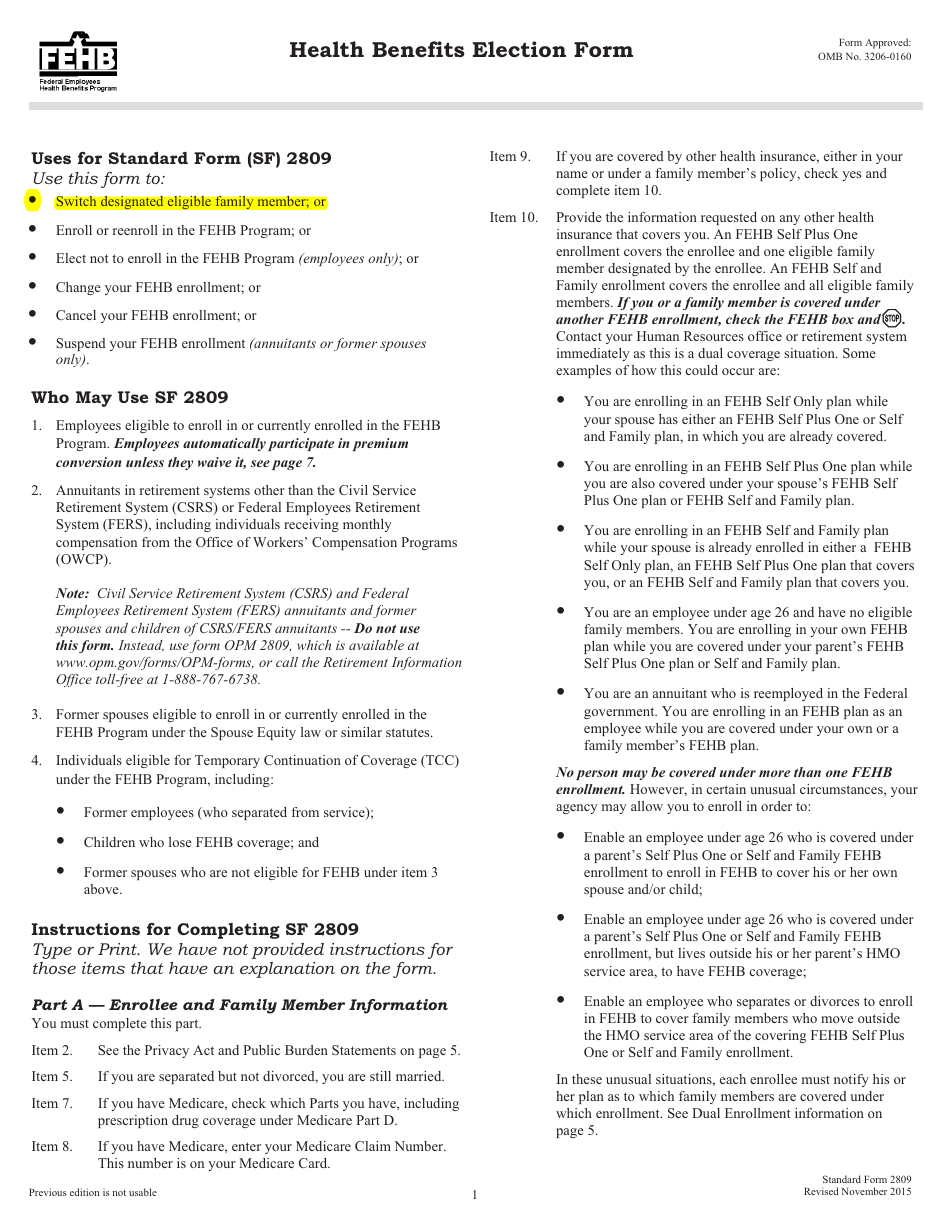
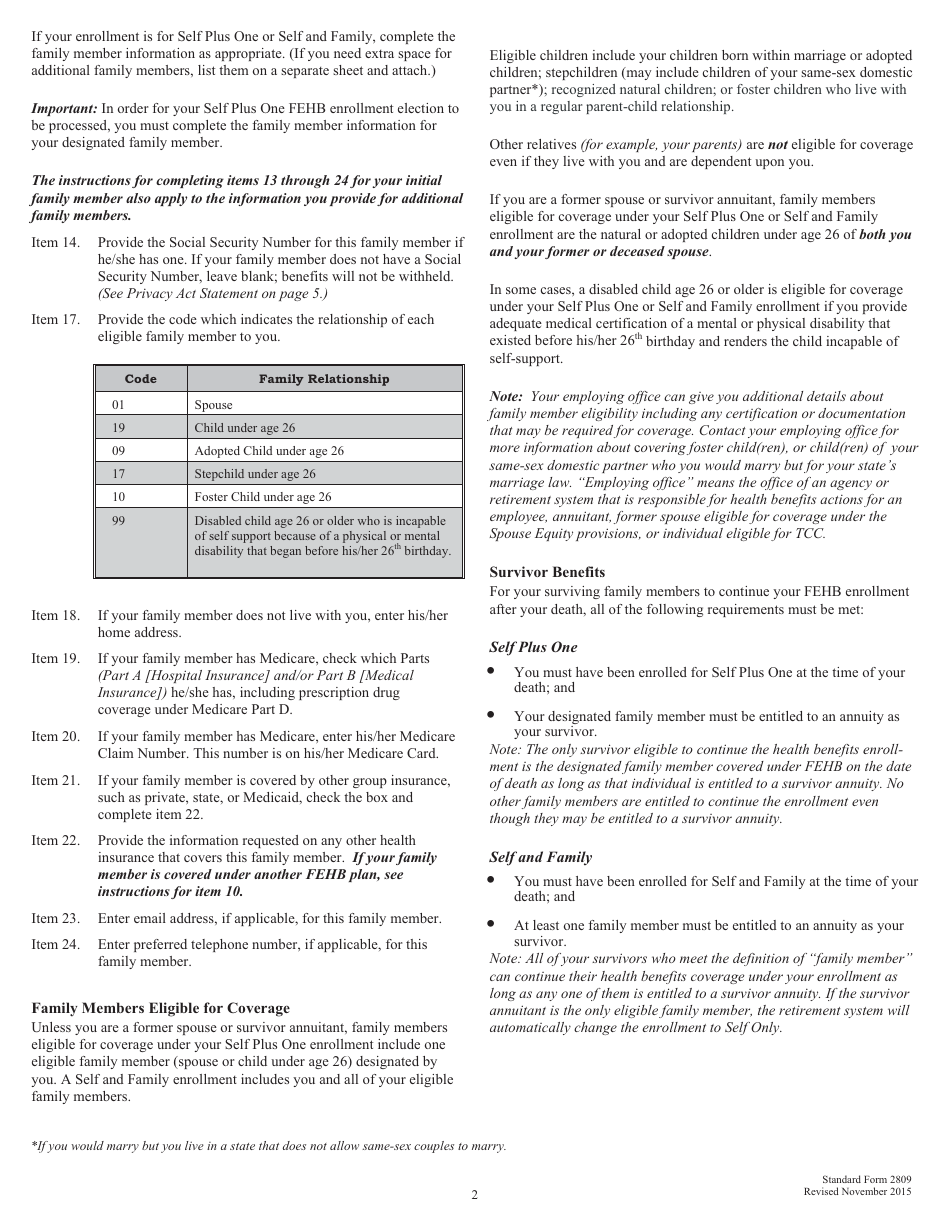
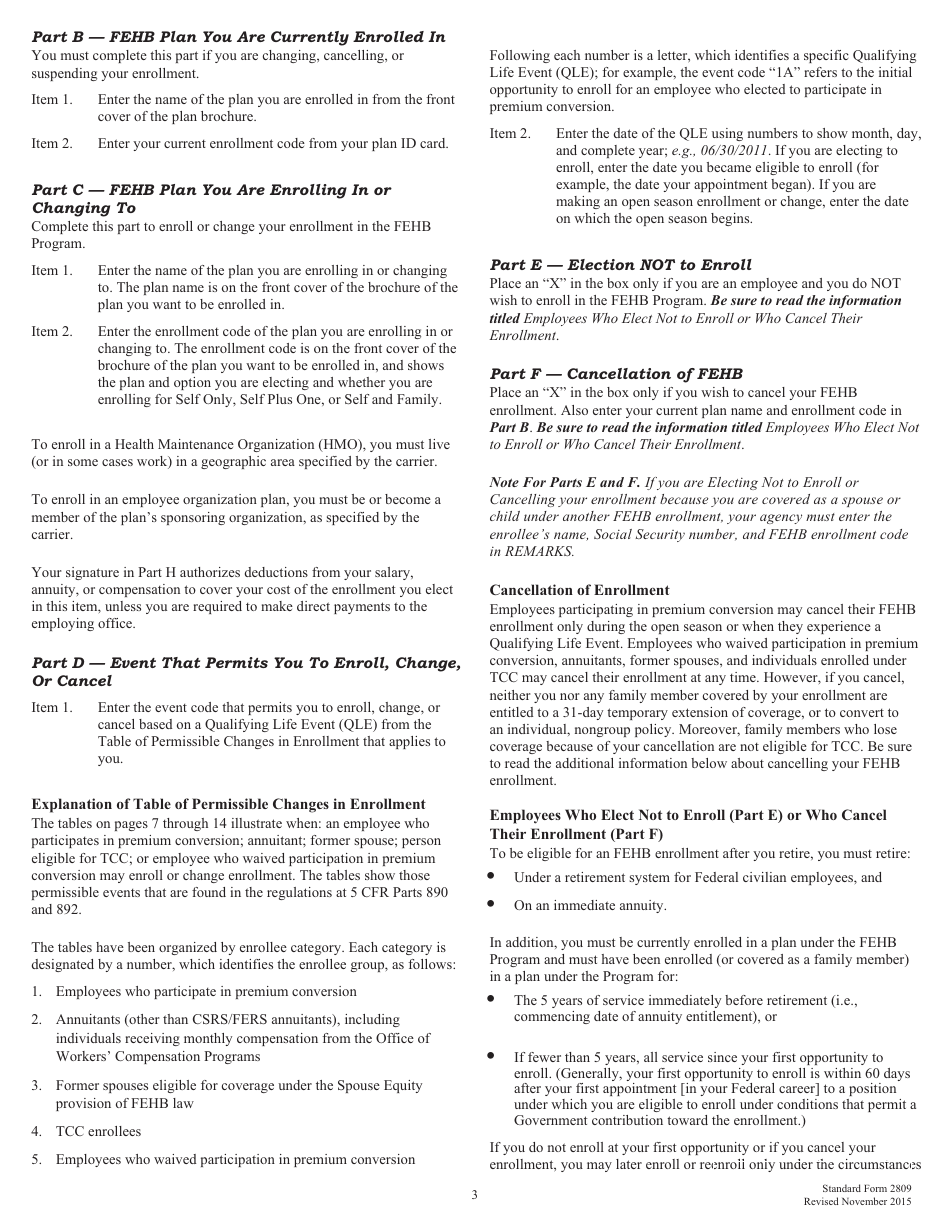
Q: What is OPM Form SF-2809?
A: OPM Form SF-2809 is the Employee Health Benefits Registration Form.
Q: What is the purpose of OPM Form SF-2809?
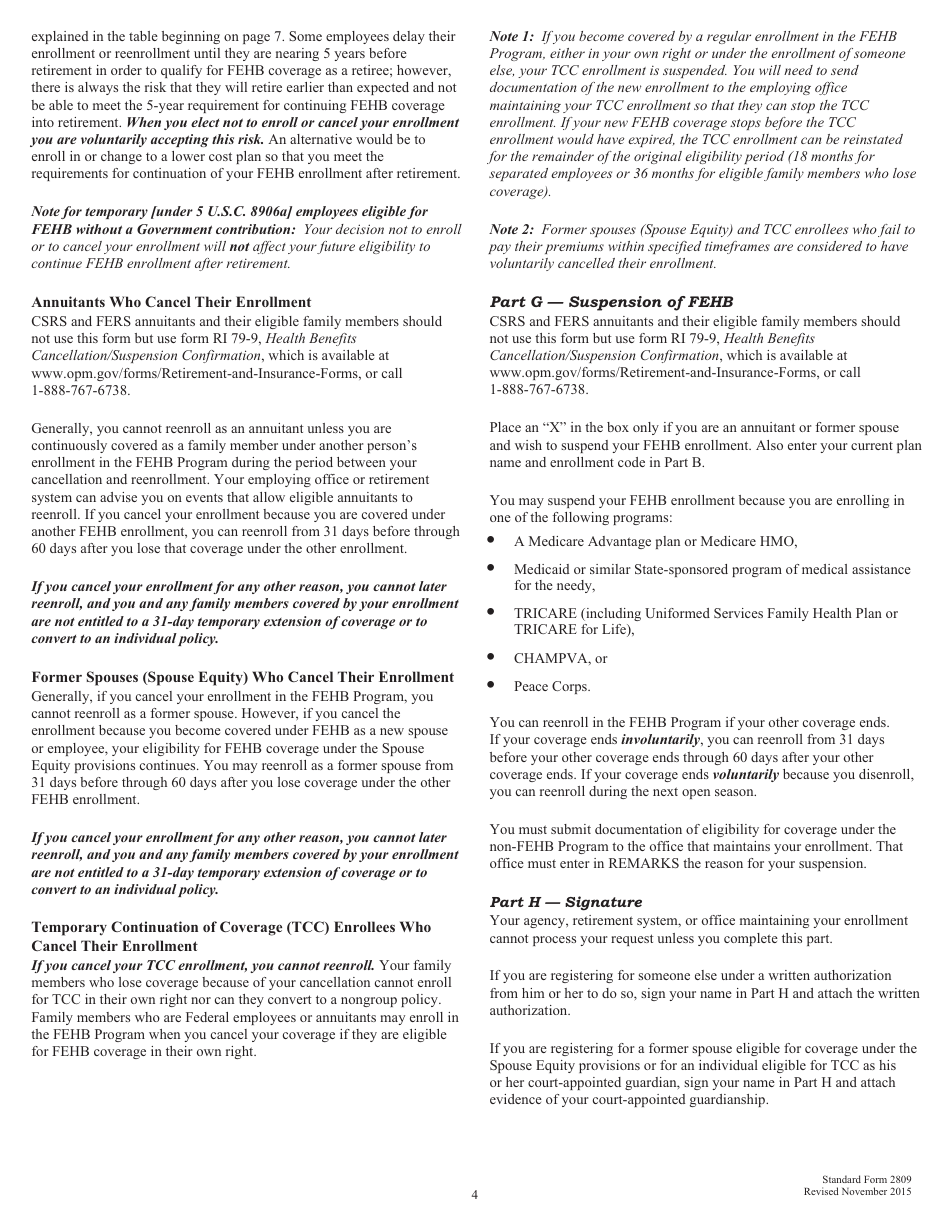
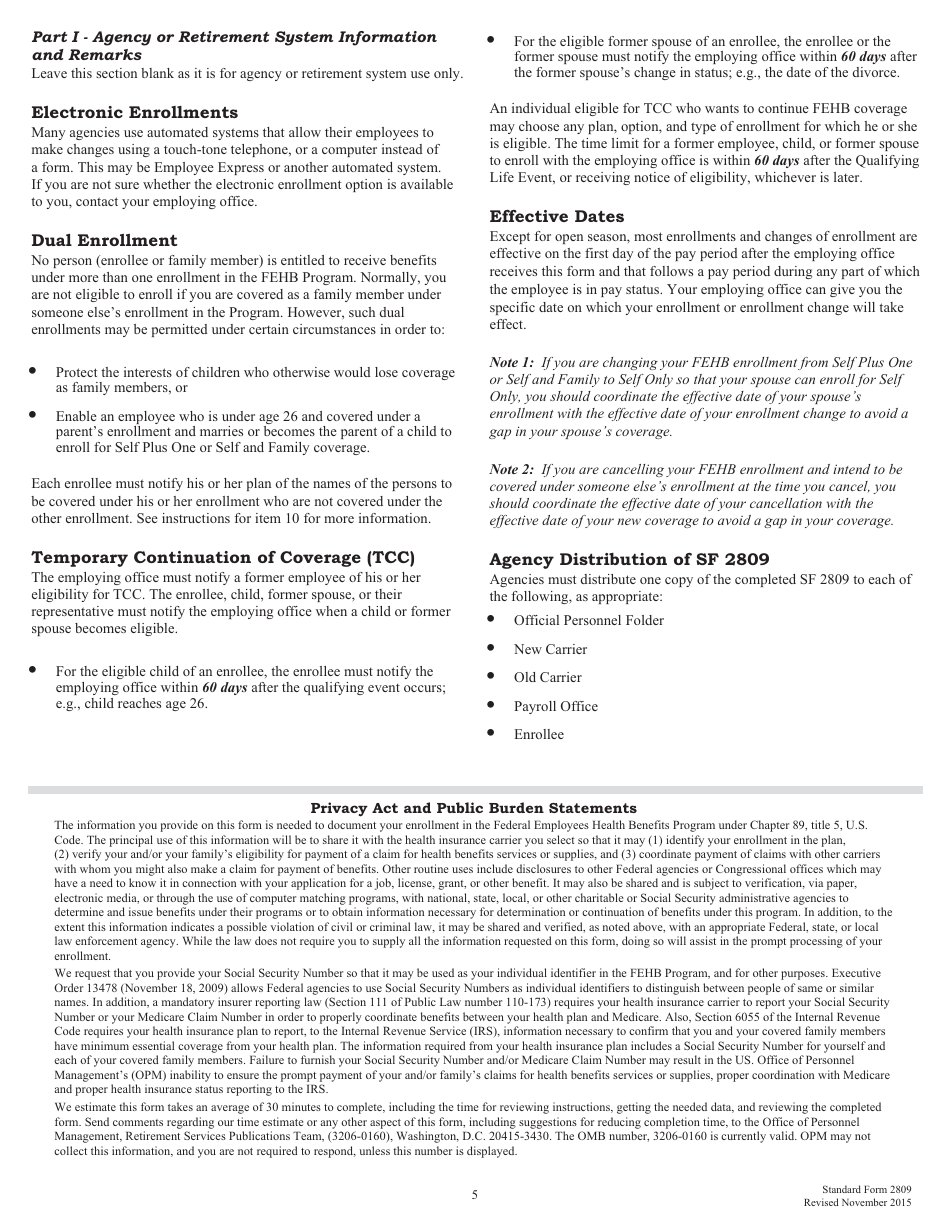
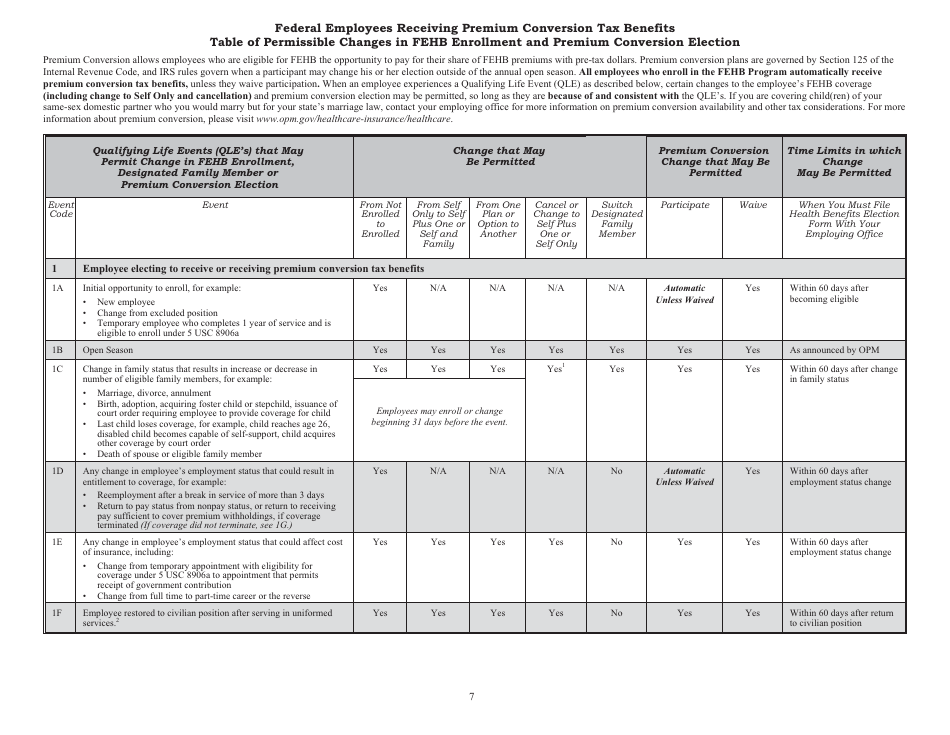
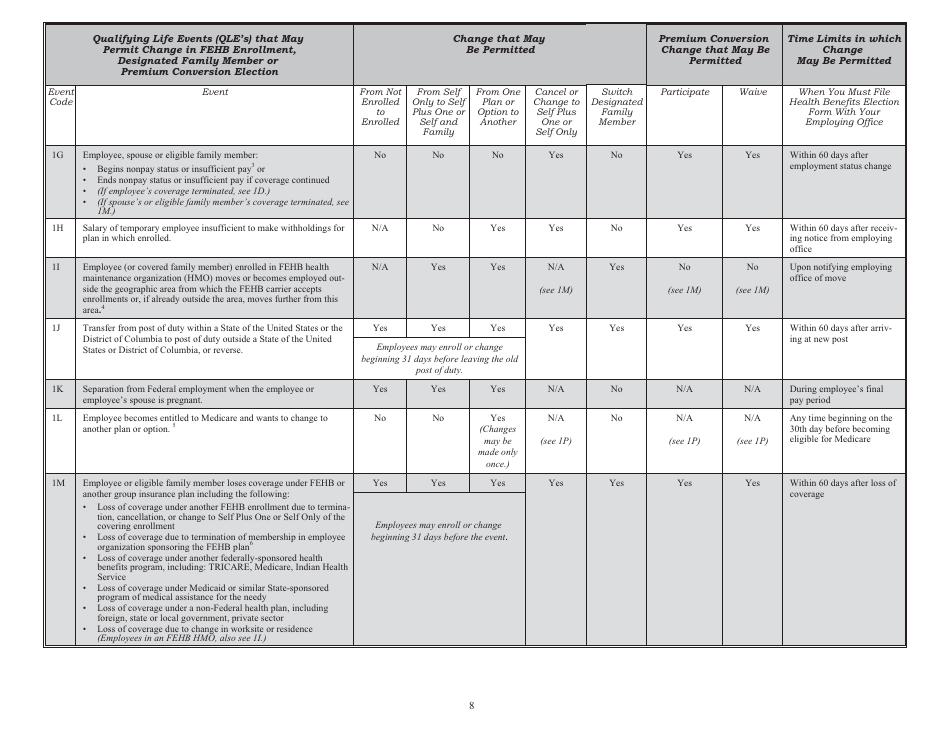
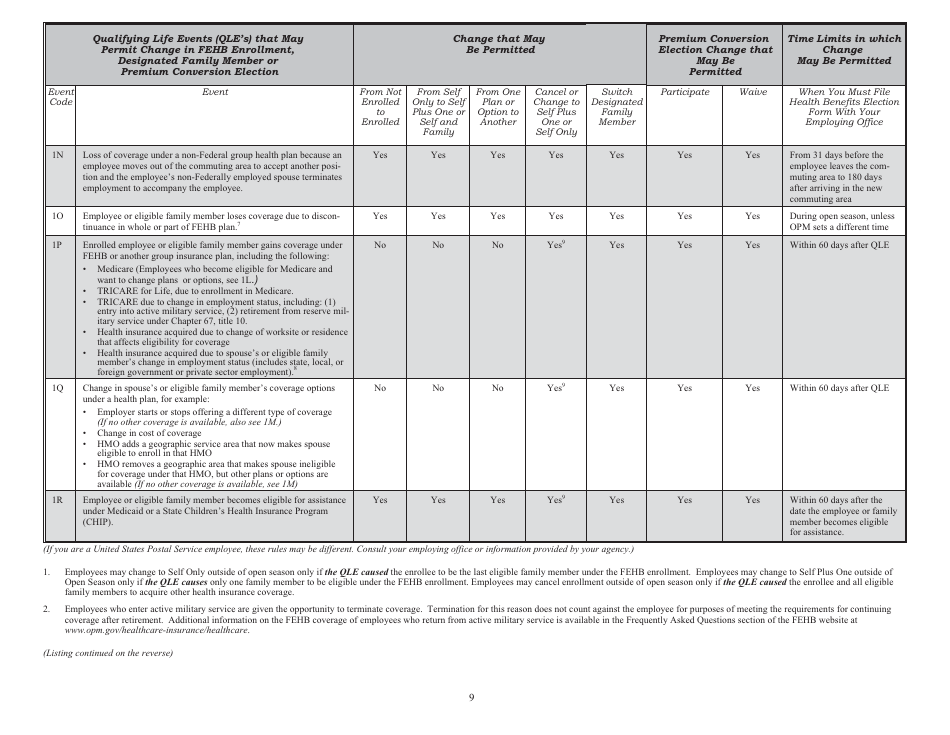
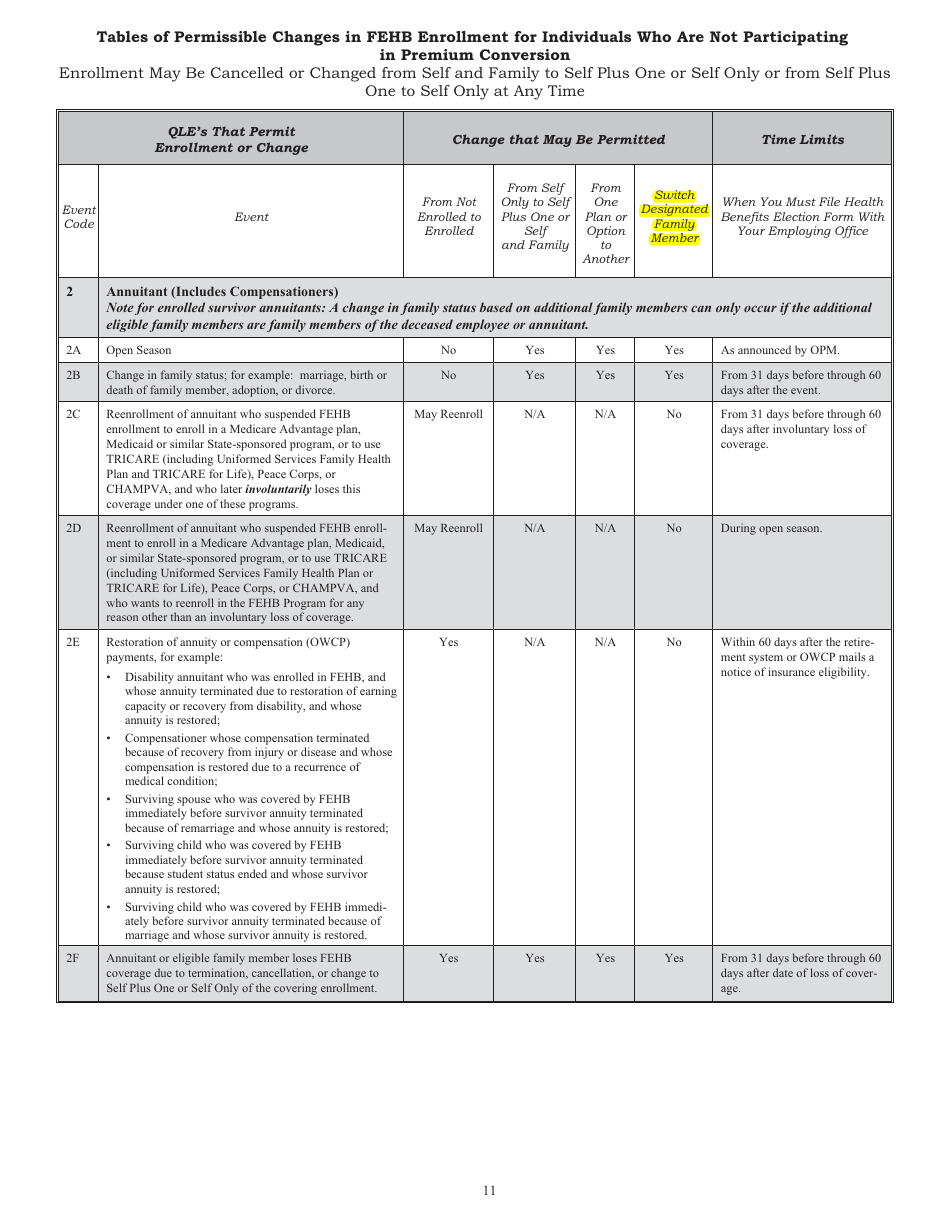
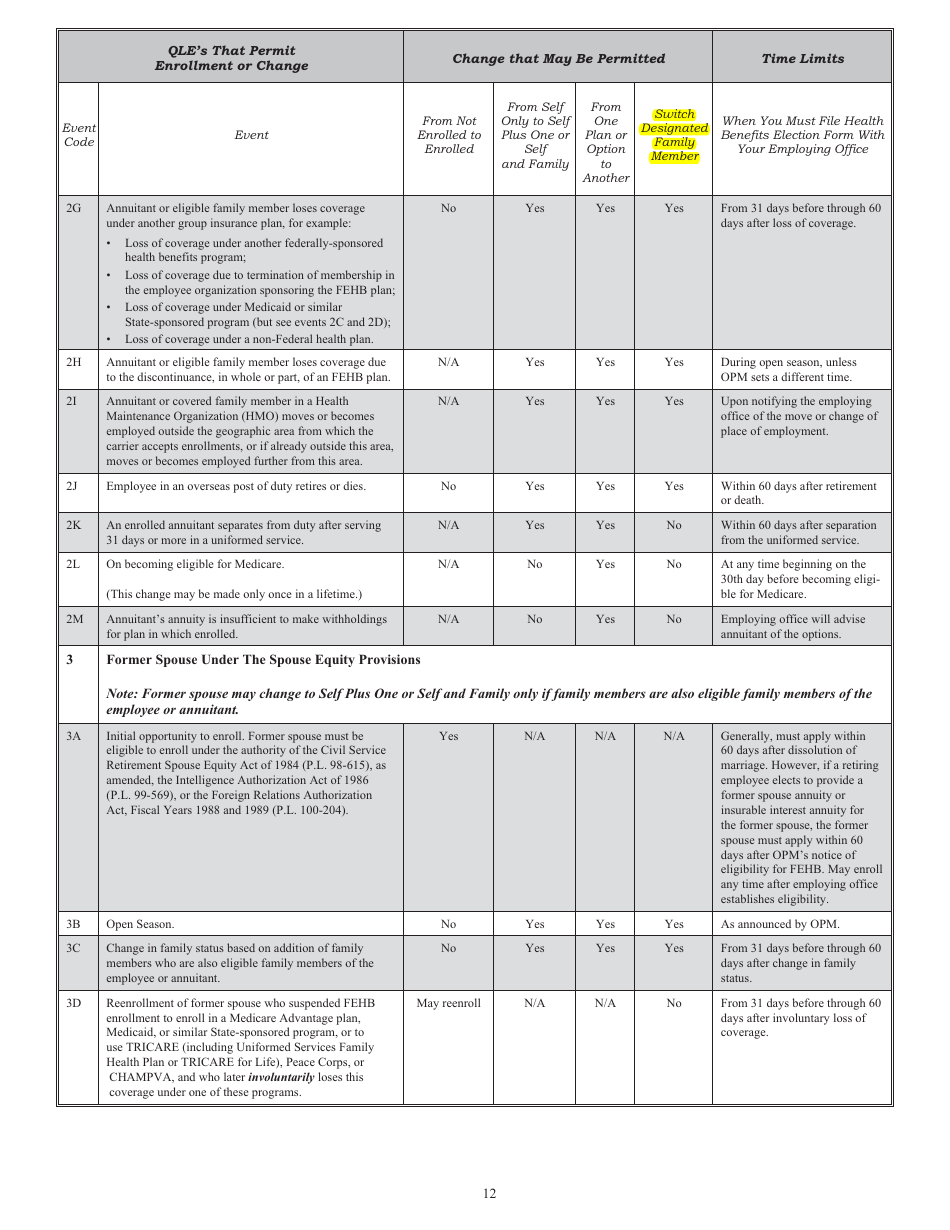
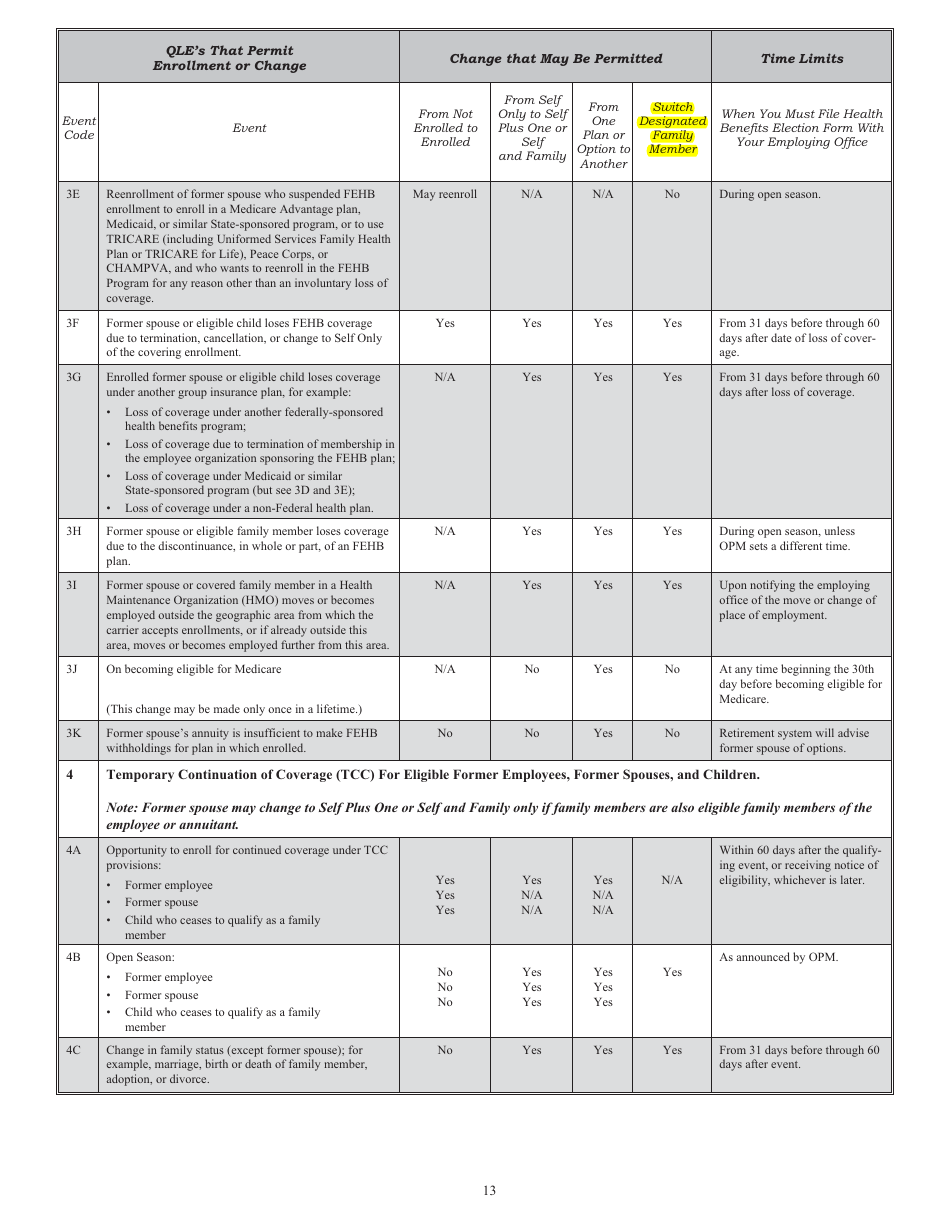
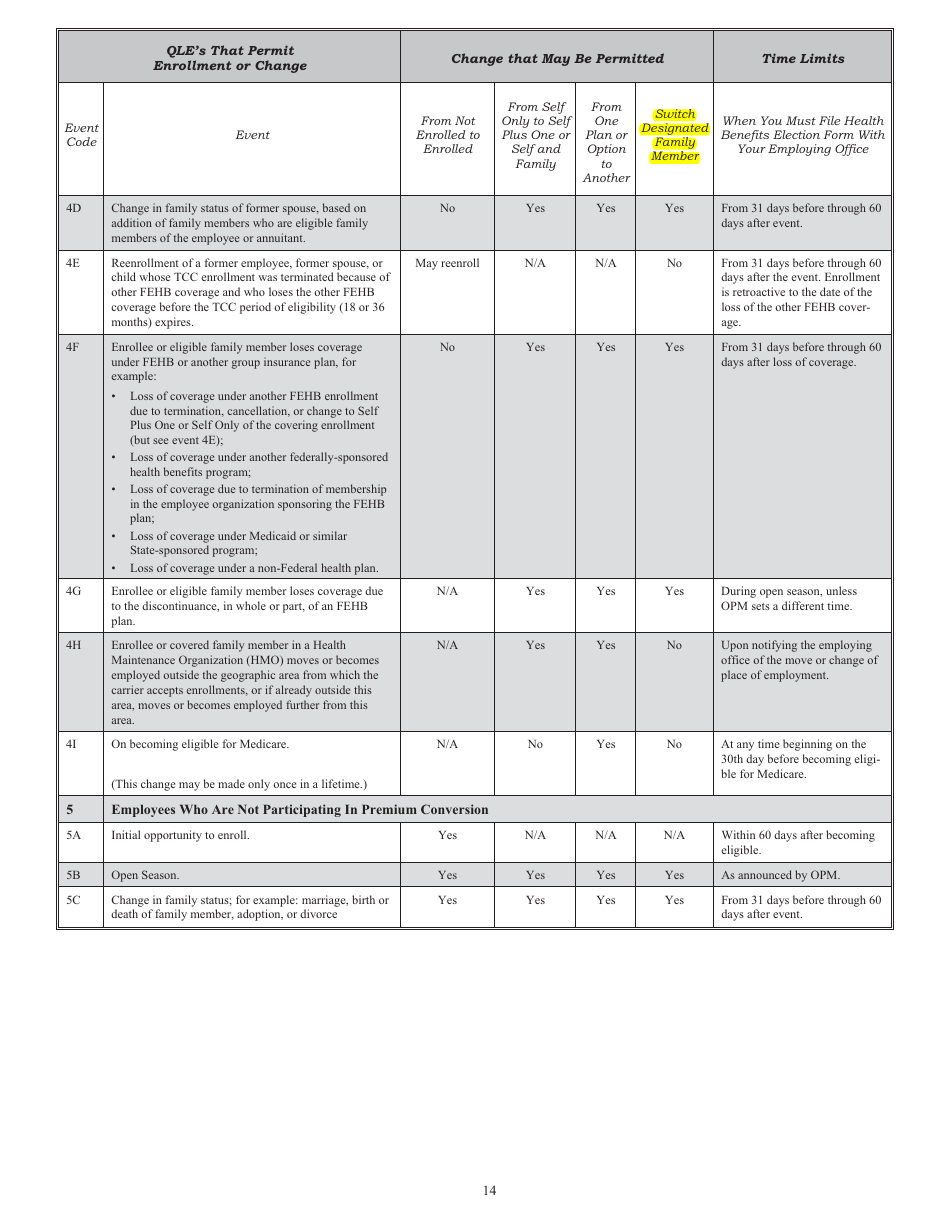
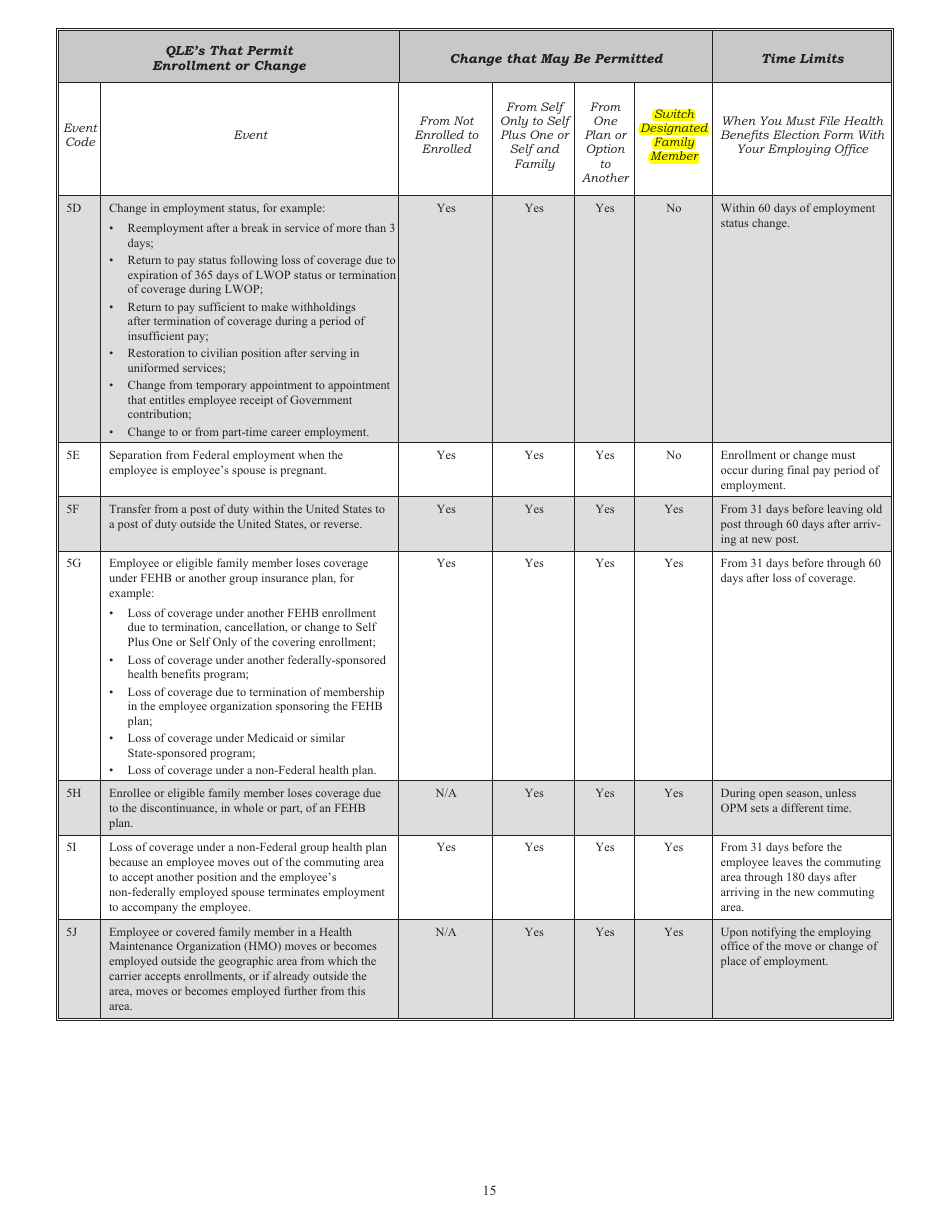
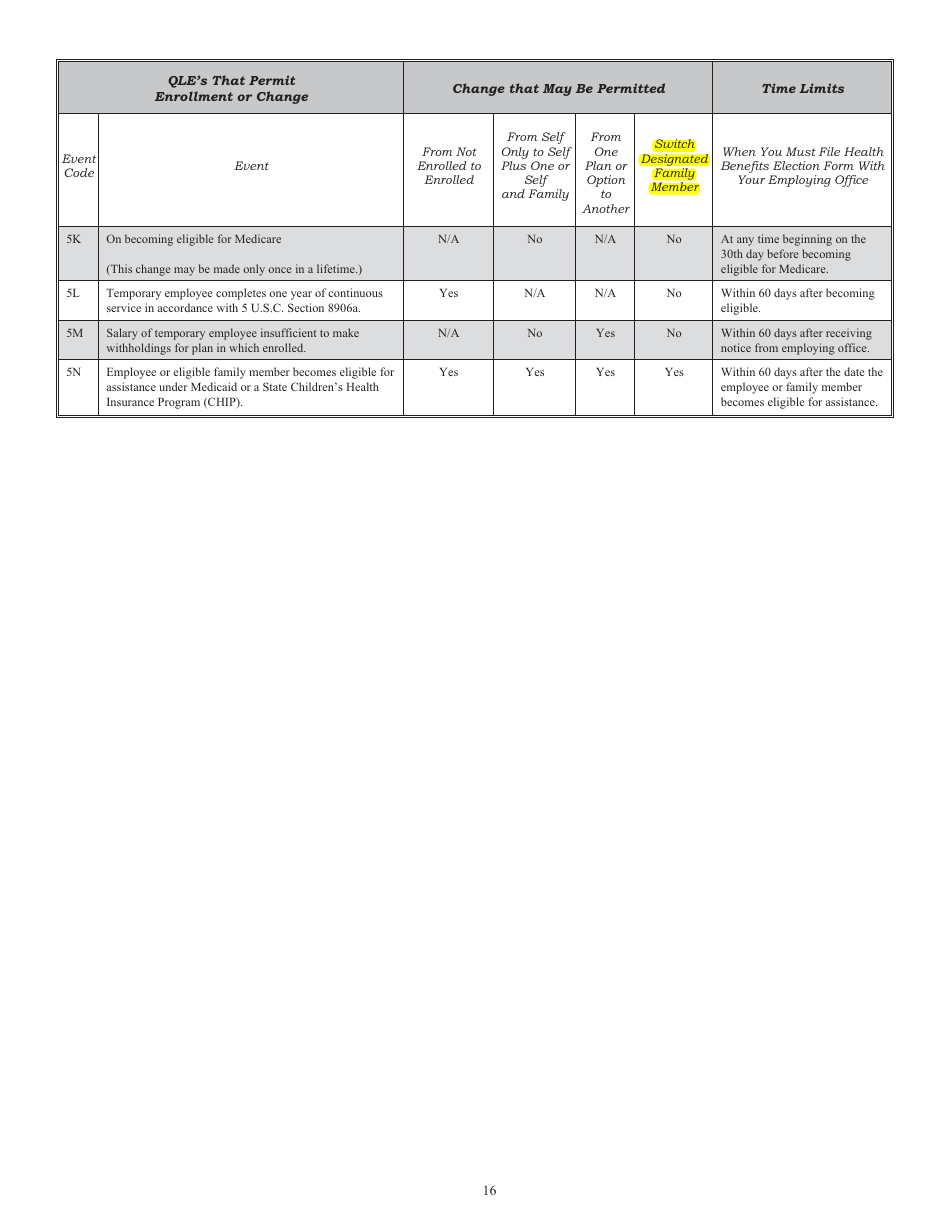
A: The purpose of OPM Form SF-2809 is to enroll or make changes to an employee's health benefits plan.
Q: Who needs to fill out OPM Form SF-2809?
A: Federal employees who are eligible for health benefits need to fill out OPM Form SF-2809.
Q: What information is required on OPM Form SF-2809?
A: OPM Form SF-2809 requires information such as the employee's personal details, chosen health benefits plan, and any eligible family members.
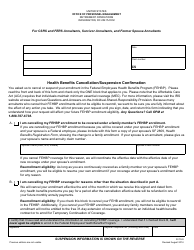
Q: Can I make changes to my health benefits plan using OPM Form SF-2809?
A: Yes, you can make changes to your health benefits plan using OPM Form SF-2809 during the annual Open Season or if you experience a Qualifying Life Event.
Form Details:
- Released on November 1, 2015;
- The latest available edition released by the U.S. Office of Personnel Management;
- Easy to use and ready to print;
- Yours to fill out and keep for your records;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of OPM Form SF-2809 by clicking the link below or browse more documents and templates provided by the U.S. Office of Personnel Management.