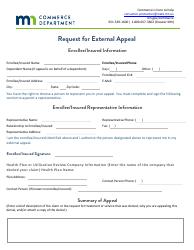
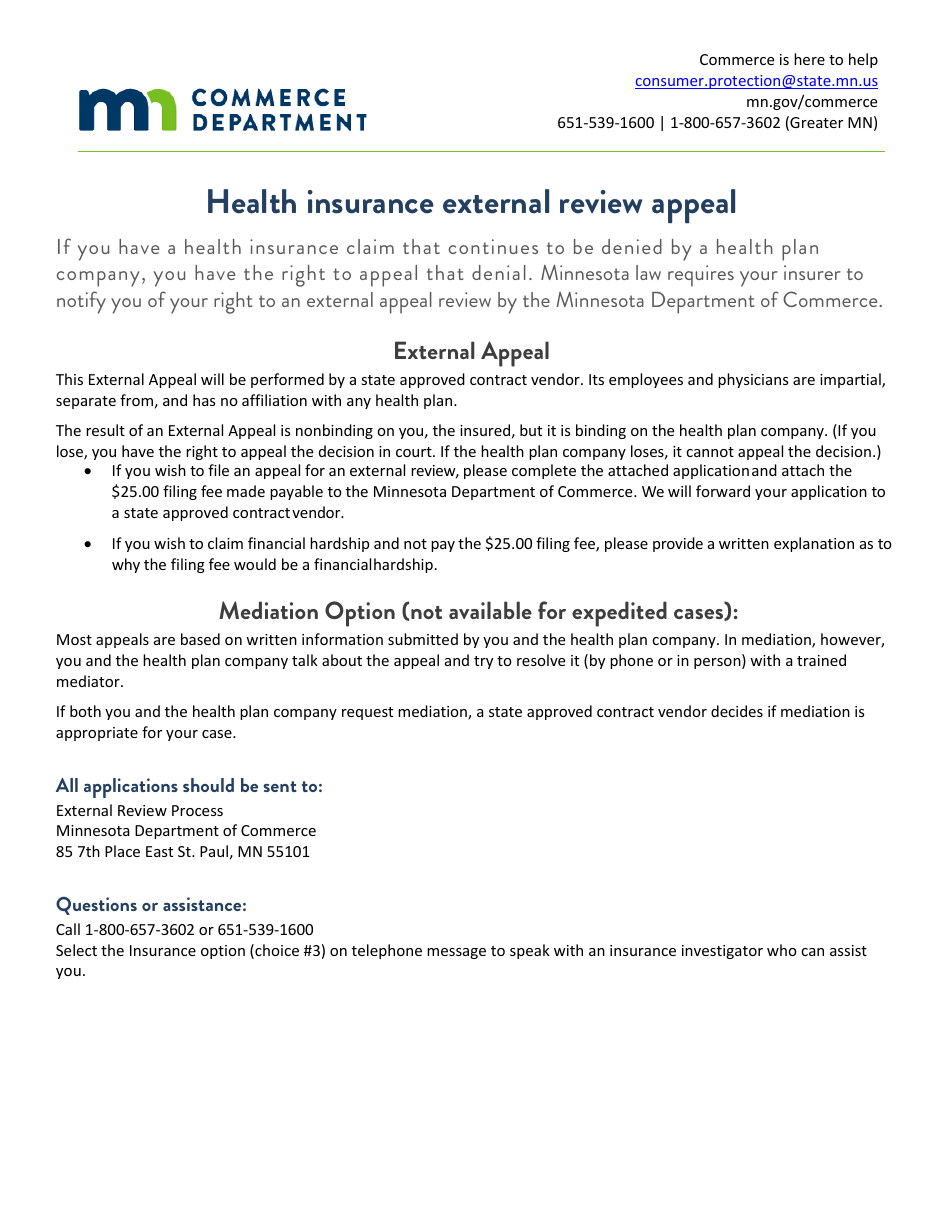
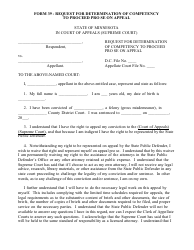
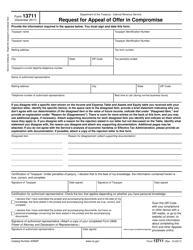
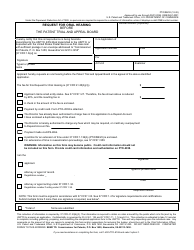
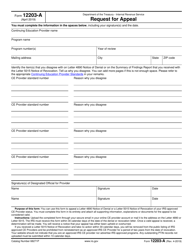
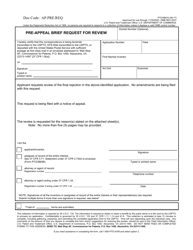
Request for External Appeal - Minnesota
Request for External Appeal is a legal document that was released by the Minnesota Commerce Department - a government authority operating within Minnesota.
FAQ
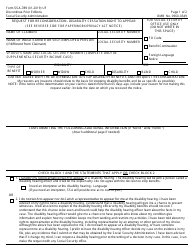
Q: What is an external appeal in Minnesota?
A: An external appeal in Minnesota is a process where an independent third party reviews a denial of health insurance coverage.
Q: Who can request an external appeal in Minnesota?
A: Any insured individual or their authorized representative can request an external appeal in Minnesota.
Q: When can I request an external appeal in Minnesota?
A: You can request an external appeal in Minnesota within 180 days of receiving a denial of coverage notice.
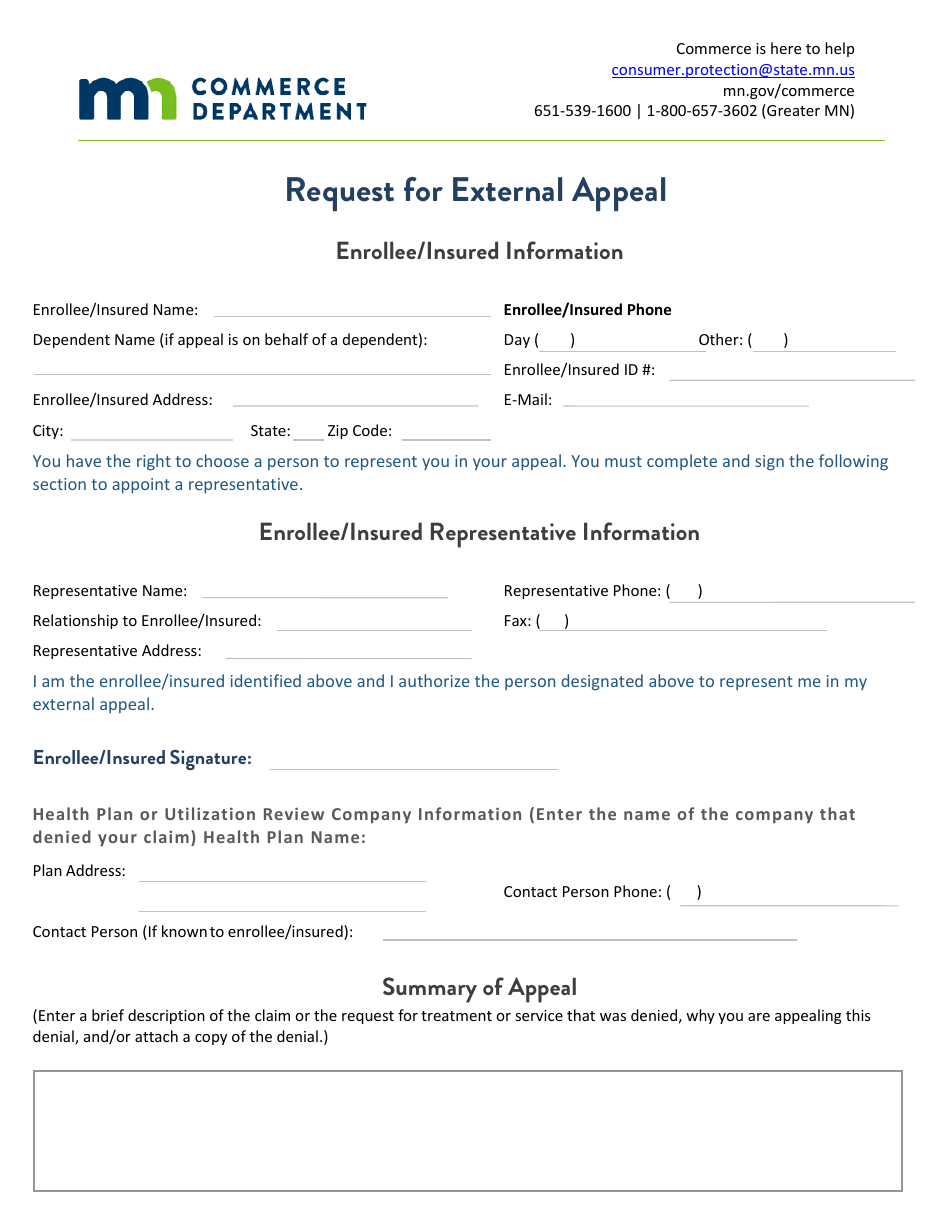
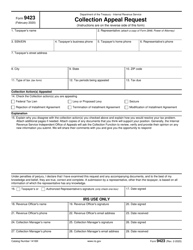
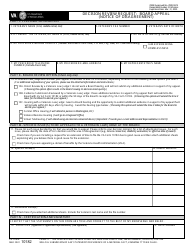
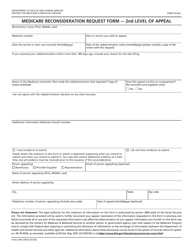
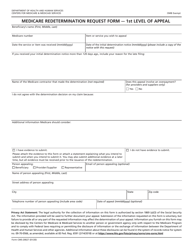
Q: How do I request an external appeal in Minnesota?
A: To request an external appeal in Minnesota, you need to complete and submit a request form provided by the Minnesota Department of Commerce.
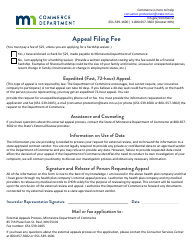
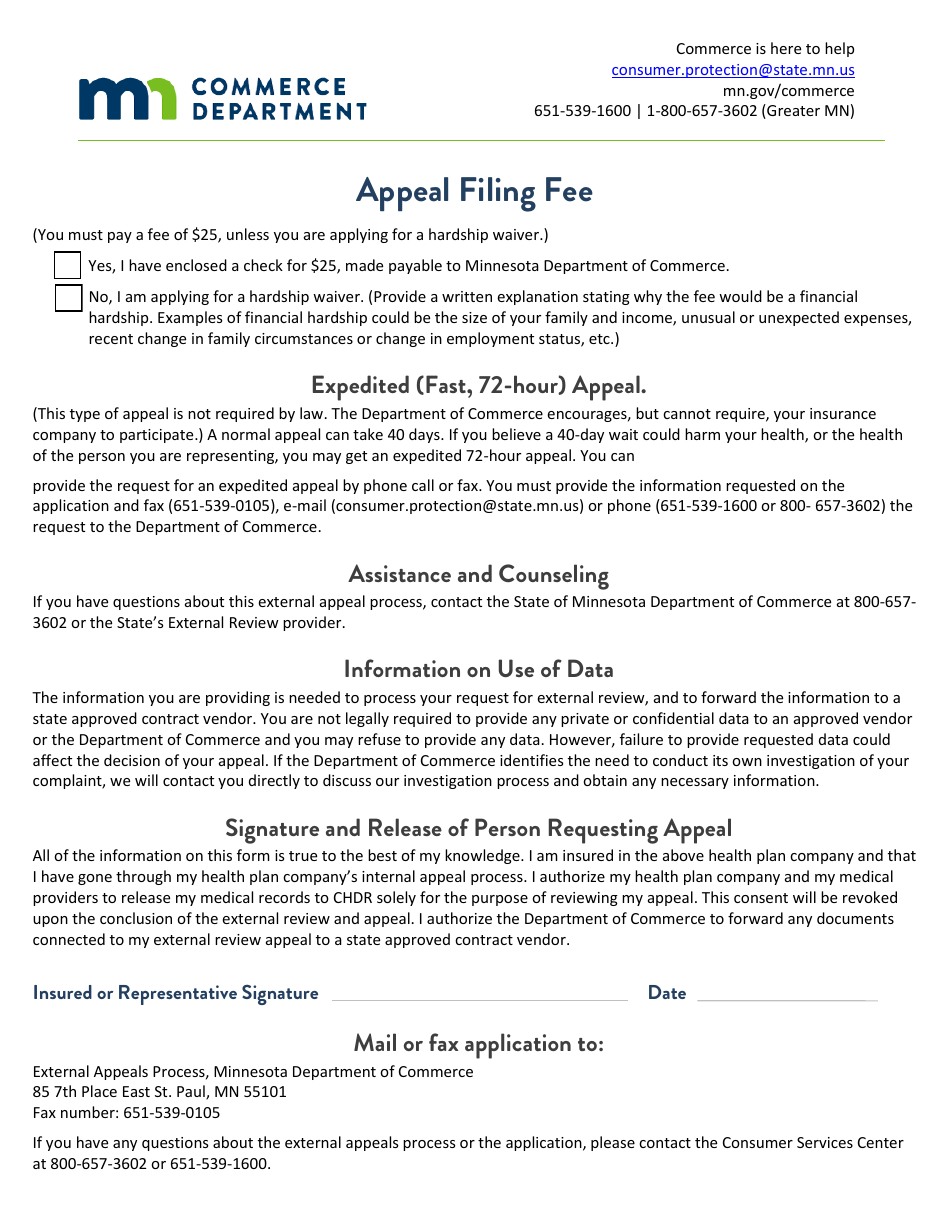
Q: Is there a fee to request an external appeal in Minnesota?
A: No, there is no fee to request an external appeal in Minnesota.
Q: What happens after I request an external appeal in Minnesota?
A: After you request an external appeal in Minnesota, an independent external review organization will be assigned to review your case.
Q: How long does the external appeal process take in Minnesota?
A: The external appeal process in Minnesota generally takes about 45 days.
Q: Can I continue receiving treatment during the external appeal process in Minnesota?
A: Yes, you can continue receiving treatment during the external appeal process in Minnesota.
Q: What decisions can the external appeal in Minnesota make?
A: The external appeal in Minnesota can uphold the denial, overturn the denial, or modify it in some way.
Form Details:
- The latest edition currently provided by the Minnesota Commerce Department;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Minnesota Commerce Department.