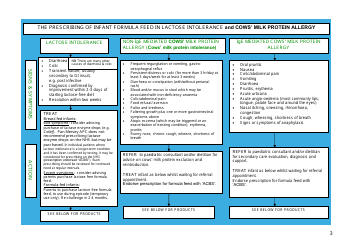
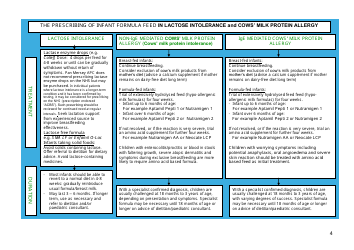
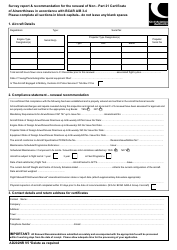
Pan-Mersey Prescribing Guidelines for Specialist Infant Formula Feeds in Lactose Intolerance and Cows' Milk Protein Allergy - United Kingdom
Fill PDF Online
Fill out online for free
without registration or credit card
This "Pan-Mersey Prescribing Guidelines for Specialist Infant Formula Feeds in Lactose Intolerance and Cows' Milk Protein Allergy" is a part of the paperwork released by the United Kingdom National Health Service specifically for United Kingdom residents.
The latest fillable version of the document was released on November 1, 2016 and can be downloaded through the link below or found through the department's forms library.