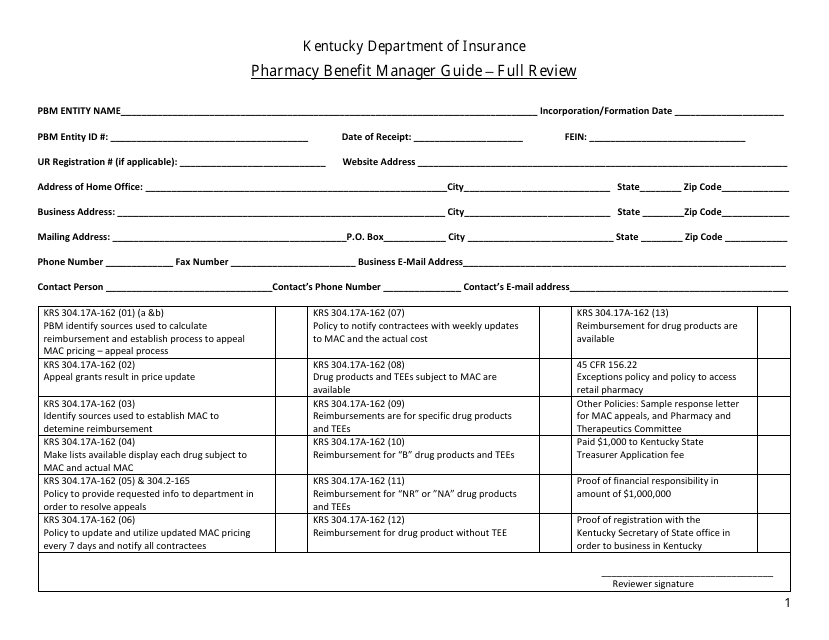
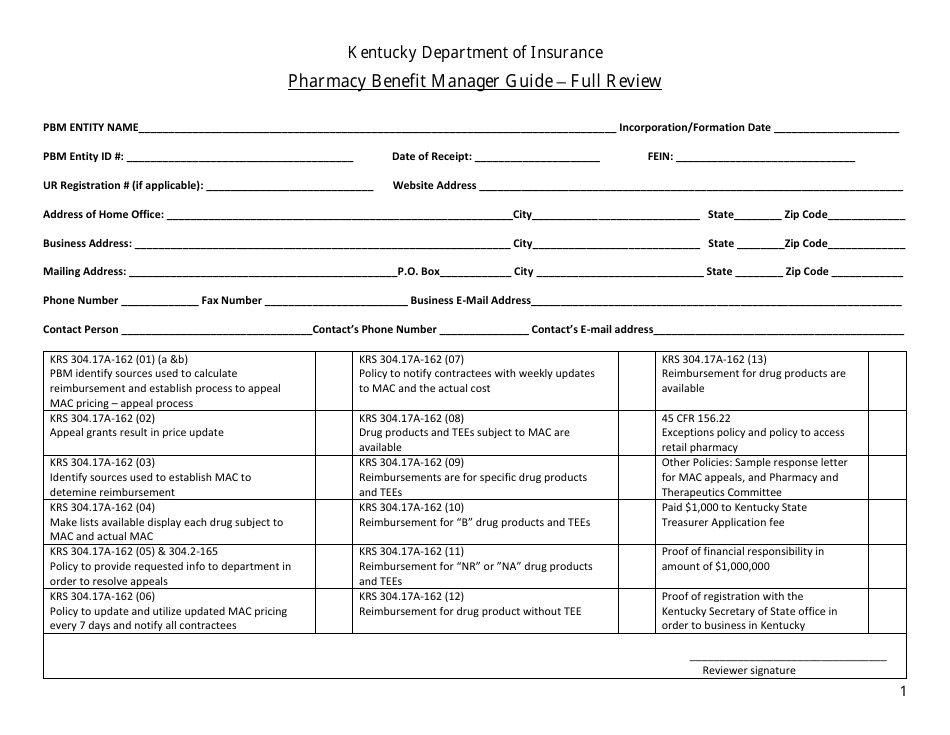
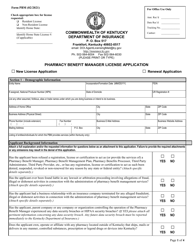
Pharmacy Benefit Manager Guide - Full Review - Kentucky
Pharmacy Benefit Manager Guide - Full Review is a legal document that was released by the Kentucky Department of Insurance - a government authority operating within Kentucky.
FAQ
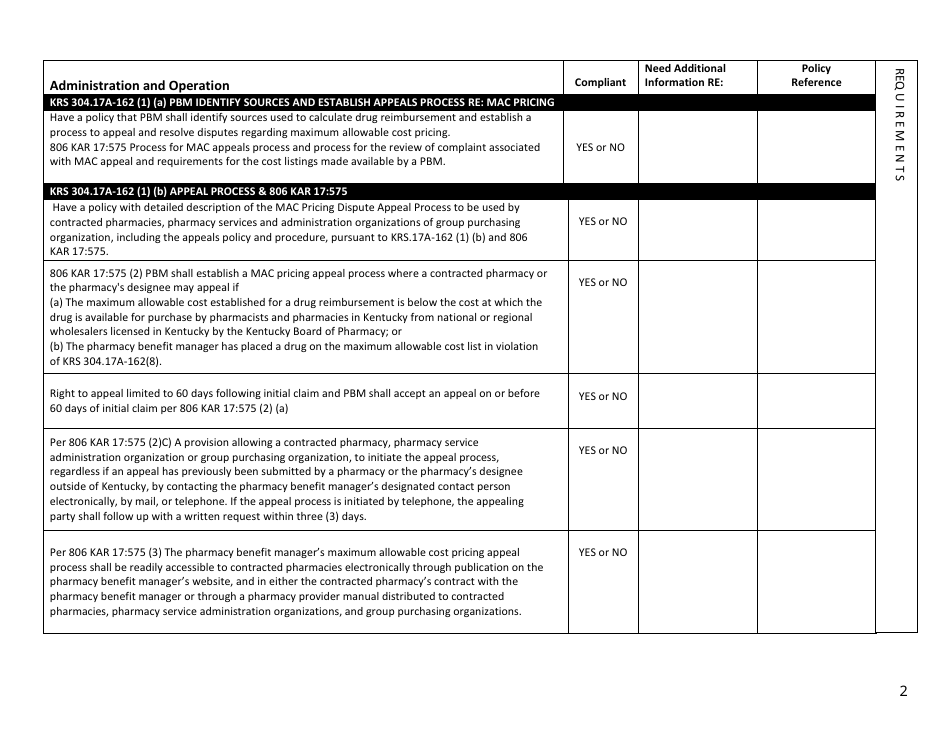
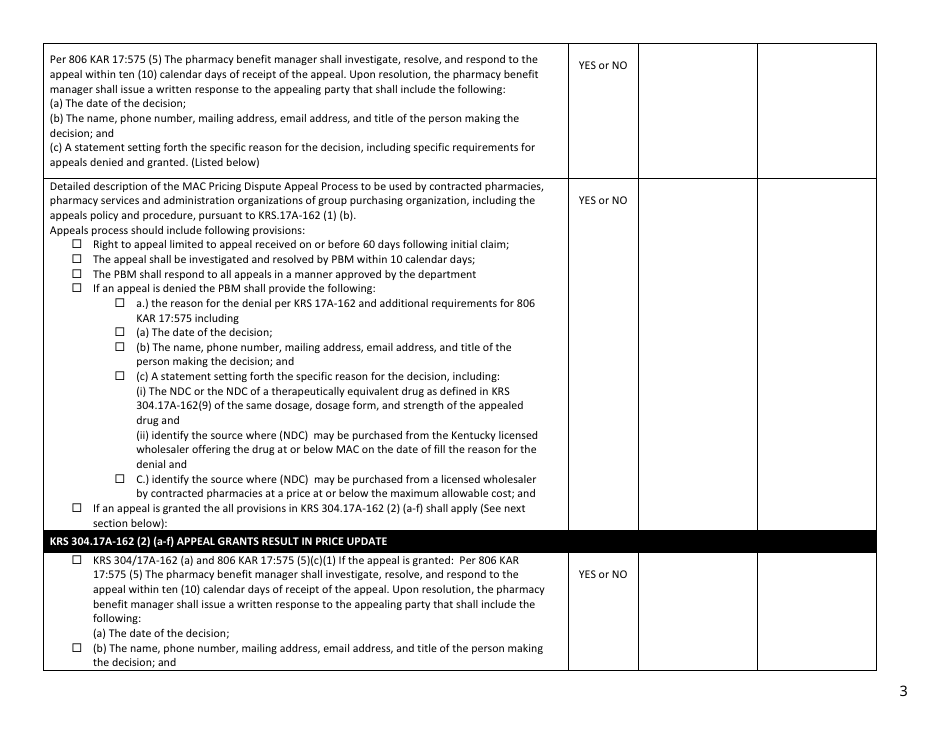
Q: What is a pharmacy benefit manager (PBM)?
A: A pharmacy benefit manager (PBM) is a third-party administrator that handles prescription drug benefits for health plans.
Q: What services do pharmacy benefit managers (PBMs) provide?
A: PBMs provide various services such as negotiating drug prices with manufacturers, processing and paying prescription claims, managing pharmacy networks, and implementing drug utilization management strategies.
Q: How do pharmacy benefit managers (PBMs) negotiate drug prices?
A: PBMs negotiate drug prices with manufacturers by leveraging their purchasing power and implementing formularies to promote the use of lower-cost drugs.
Q: What is a formulary?
A: A formulary is a list of prescription drugs that an insurer or PBM covers and encourages plan members to use. It categorizes drugs into tiers, with lower-tier drugs being less expensive.
Q: How do pharmacy benefit managers (PBMs) impact drug costs?
A: PBMs play a role in managing and lowering drug costs by negotiating discounts and rebates with manufacturers, promoting the use of generic drugs, and implementing cost-control measures on high-cost medications.
Q: Do pharmacy benefit managers (PBMs) affect drug choices for patients?
A: Yes, PBMs influence drug choices by implementing formularies and restricting coverage to certain medications. However, they also work to ensure there are options for affordable and effective treatments.
Q: Can individuals use pharmacy benefit managers (PBMs) to access prescription drugs?
A: No, individuals cannot directly access PBMs. PBMs work with health plans and pharmacy networks to process and manage prescription drug benefits.
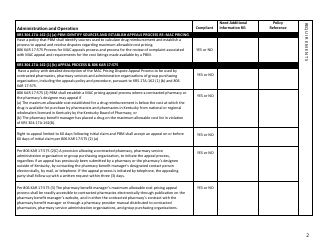
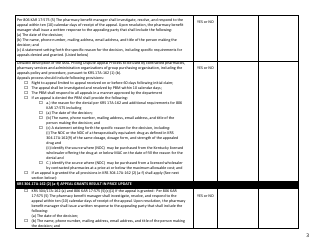
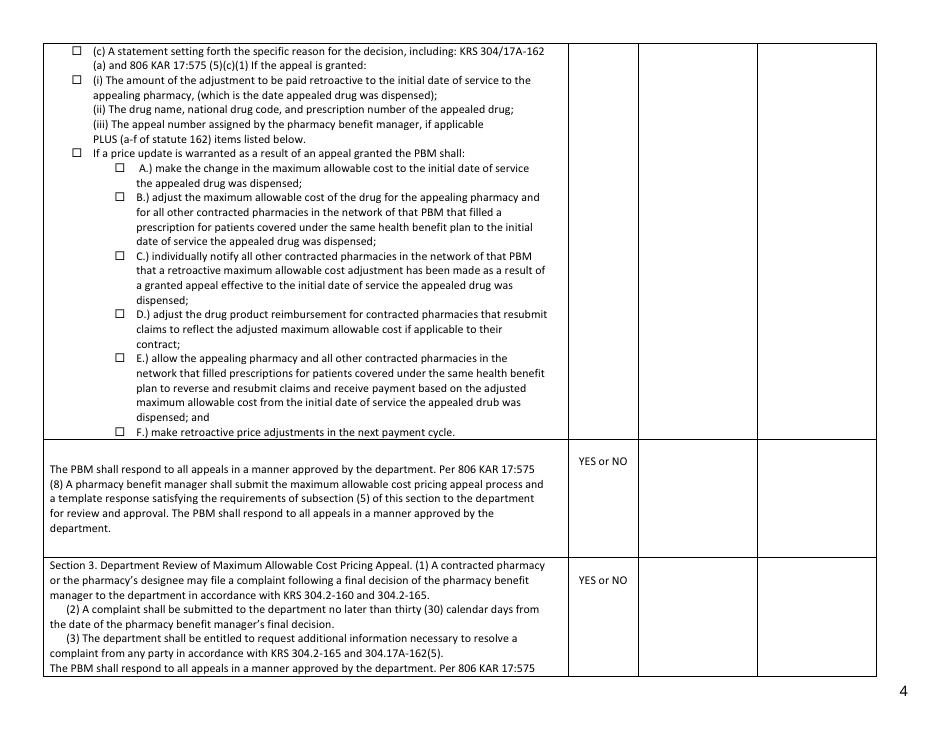
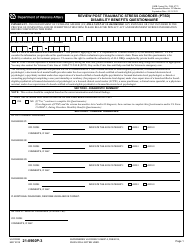
Q: Are pharmacy benefit managers (PBMs) regulated?
A: Yes, PBMs are regulated by state and federal laws. They must comply with transparency requirements and report certain information, but regulation varies by state.
Q: What should I do if I have concerns or questions about my prescription drug benefits?
A: If you have concerns or questions about your prescription drug benefits, contact your health plan or insurance provider. They can provide information and assist you.
Q: What are some common terms and abbreviations related to pharmacy benefit managers (PBMs)?
A: Common terms and abbreviations include formulary, generic drugs, brand-name drugs, specialty medications, drug tiers, prior authorization, and step therapy.
Form Details:
- The latest edition currently provided by the Kentucky Department of Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Kentucky Department of Insurance.