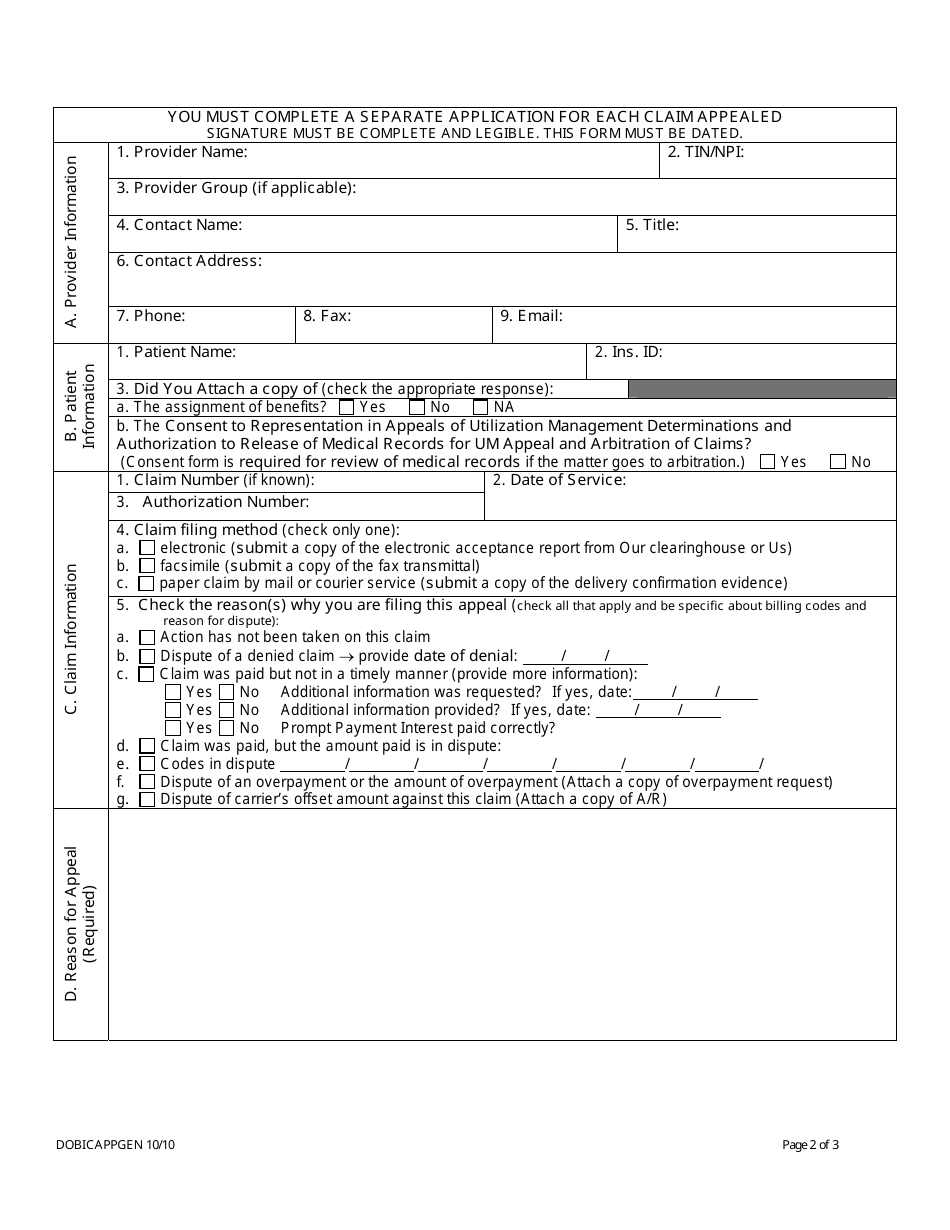
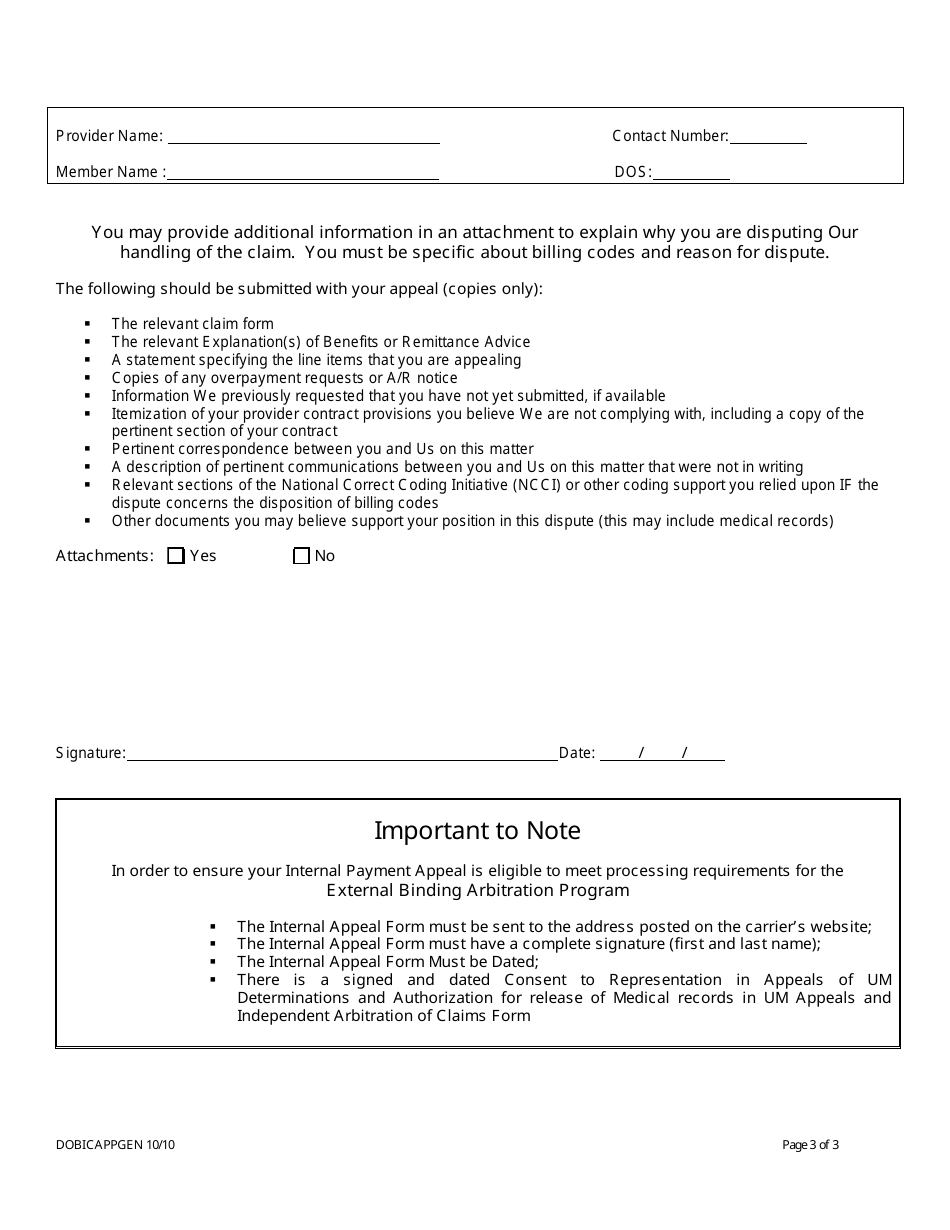
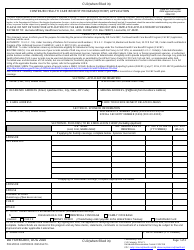
Health Care Provider Application to Appeal a Claims Determination - New Jersey
Health Care Provider Application to Appeal a Claims Determination is a legal document that was released by the New Jersey Department of Banking and Insurance - a government authority operating within New Jersey.
FAQ
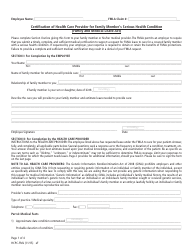
Q: What is a claims determination?
A: A claims determination is a decision made by a health care provider's insurance company regarding coverage for a specific medical service or treatment.
Q: Why would a health care provider appeal a claims determination?
A: A health care provider may appeal a claims determination if they believe it was made in error or if they disagree with the decision.
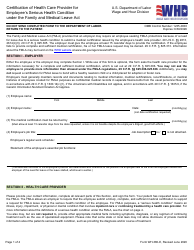
Q: What is the process for appealing a claims determination in New Jersey?
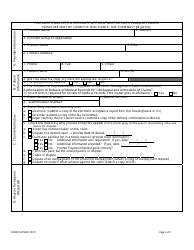
A: The process for appealing a claims determination in New Jersey varies depending on the insurance company. However, generally, it involves submitting a formal appeal in writing along with supporting documentation.
Q: Can a health care provider request an expedited review of their appeal?
A: Yes, a health care provider can request an expedited review of their appeal if they believe it is necessary due to the patient's health condition.
Q: What should a health care provider do if their appeal is denied?
A: If a health care provider's appeal is denied, they may have the option to pursue additional steps such as mediation or litigation to further challenge the claims determination.
Q: Is there a time limit for filing an appeal?
A: Yes, there is typically a time limit for filing an appeal after receiving a claims determination. It is important for health care providers to review their insurance policy or contact their insurance company to determine the specific deadline.
Form Details:
- Released on October 1, 2010;
- The latest edition currently provided by the New Jersey Department of Banking and Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the New Jersey Department of Banking and Insurance.