Memorandum (Compendium of Animal Rabies Prevention and Control, 2011) - National Association of State Public Health Veterinarians, Inc.
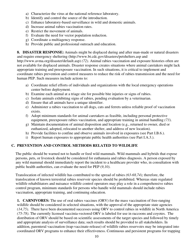
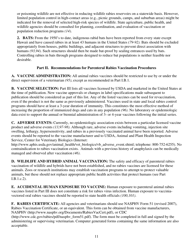
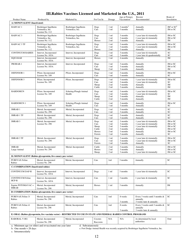
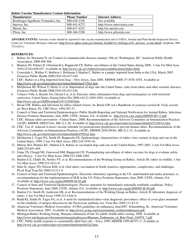
The Memorandum is a document created by the National Association of State Public Health Veterinarians, Inc. It serves as a compendium of guidelines and recommendations for the prevention and control of animal rabies. It provides guidance to public health officials, veterinarians, and other professionals involved in rabies control efforts.
FAQ
Q: What is the purpose of the memorandum?
A: The purpose of the memorandum is to provide guidelines for animal rabies prevention and control.
Q: Who published the memorandum?
A: The memorandum was published by the National Association of State Public Health Veterinarians, Inc.
Q: When was the memorandum published?
A: The memorandum was published in 2011.
Q: What does the memorandum cover?
A: The memorandum covers various aspects of animal rabies prevention and control.
Q: Why is animal rabies prevention important?
A: Animal rabies prevention is important to protect both human and animal health.
Q: Who is the target audience for the memorandum?
A: The target audience for the memorandum is public health veterinarians and related professionals.
Q: Is the memorandum still applicable today?
A: While the memorandum was published in 2011, it may still contain relevant information, but it is recommended to consult updated guidelines.