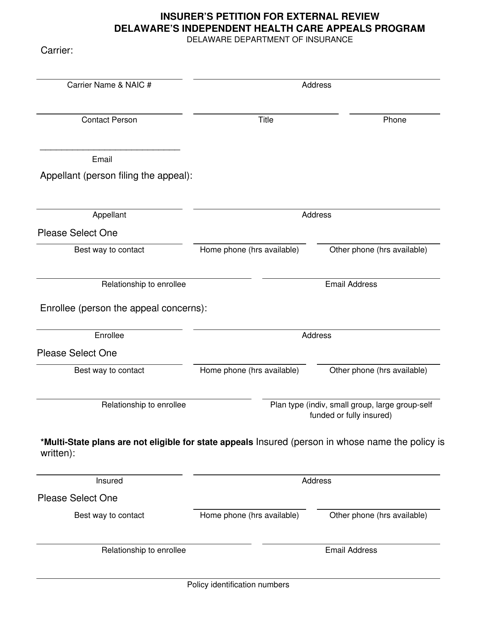
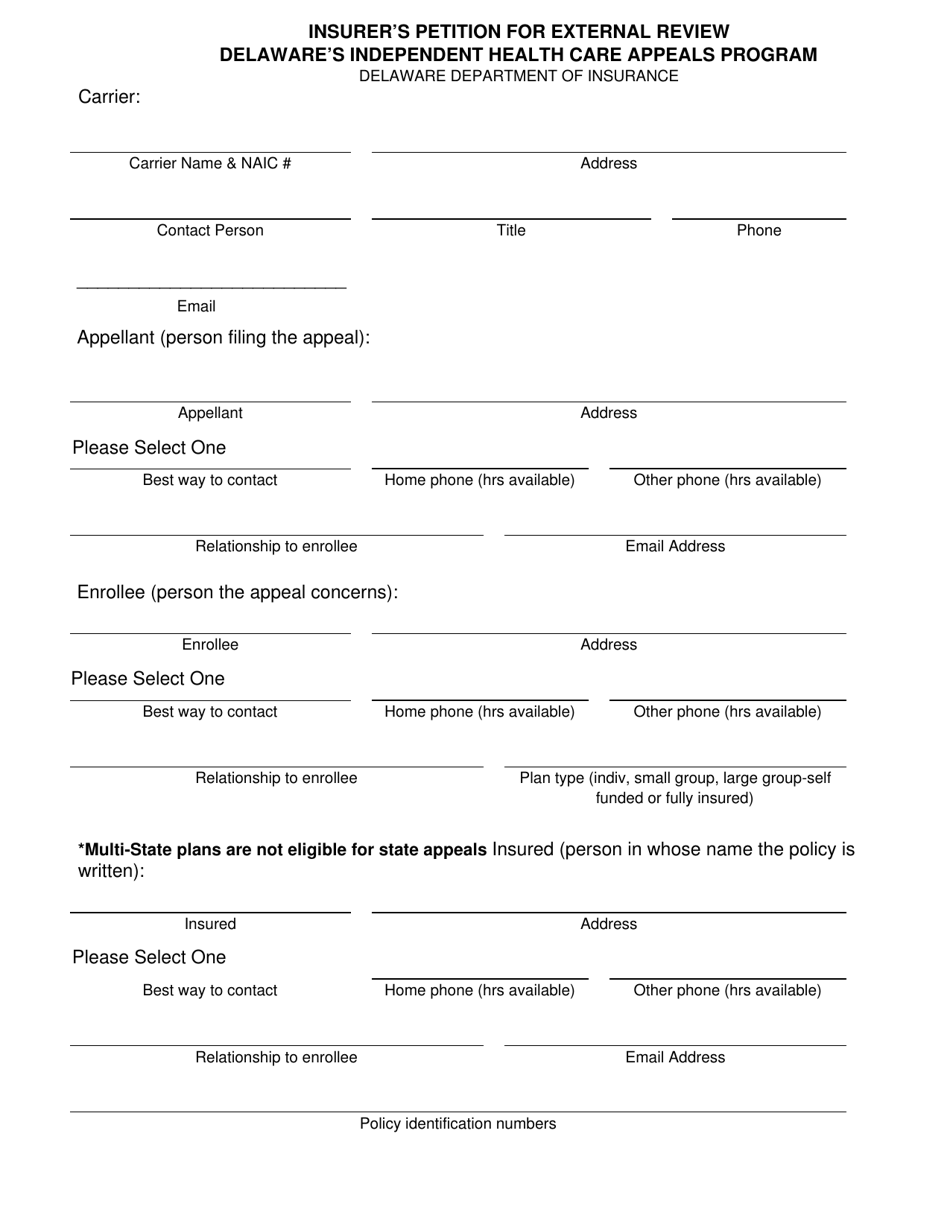
Insurer's Petition for External Review - Delaware's Independent Health Care Appeals Program - Delaware
Insurer's Petition for External Review - Delaware's Independent Health Care Appeals Program is a legal document that was released by the Delaware Department of Insurance - a government authority operating within Delaware.
FAQ
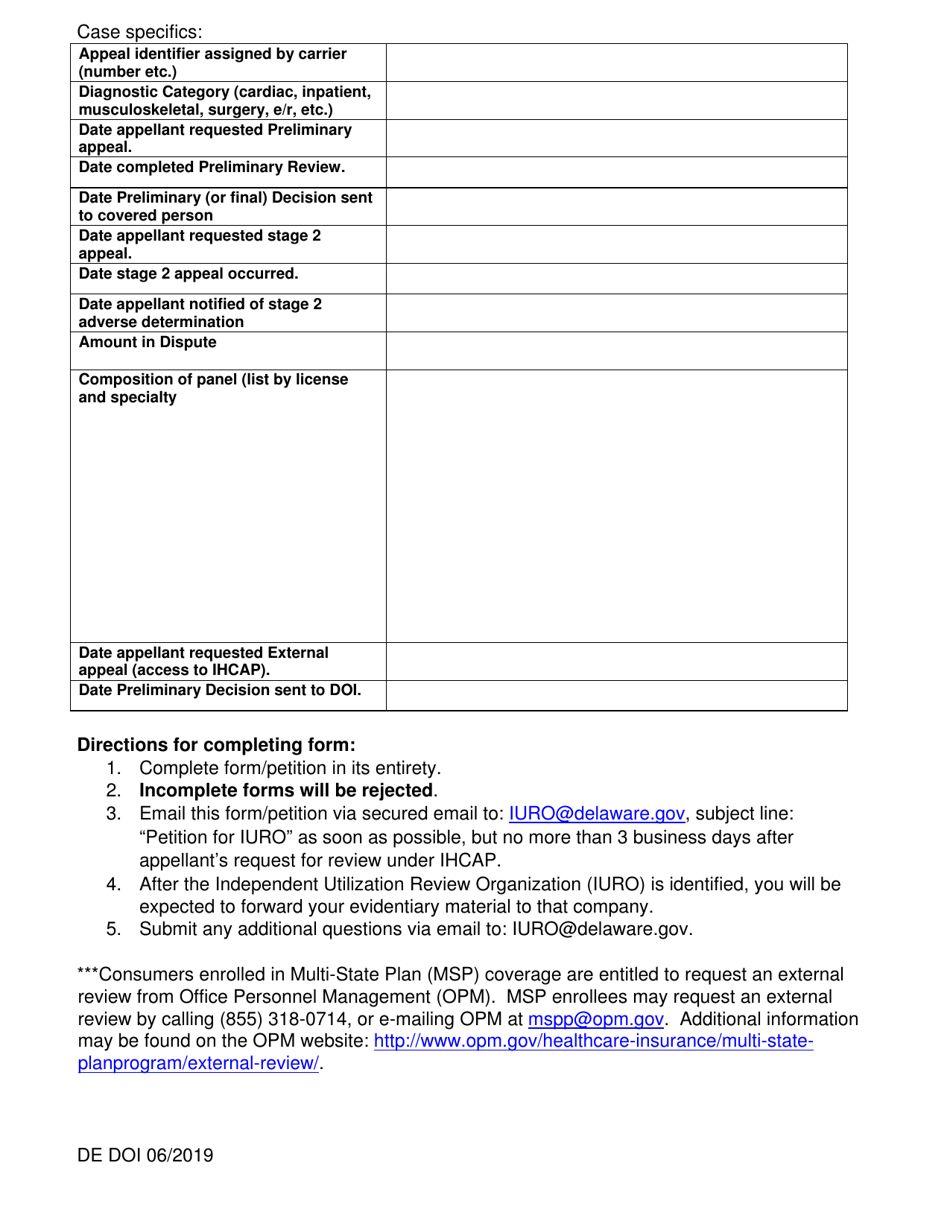
Q: What is an Insurer's Petition for External Review?
A: An Insurer's Petition for External Review is a request made by an insurance company to have an independent review of a denied health care claim.
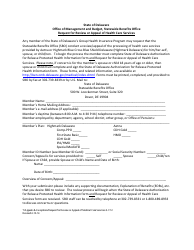
Q: What is Delaware's Independent Health Care Appeals Program?
A: Delaware's Independent Health Care Appeals Program is a program that allows consumers to appeal decisions made by their health insurance company regarding denied claims or coverage disputes.
Q: Who can file an Insurer's Petition for External Review?
A: An insurance company can file an Insurer's Petition for External Review.
Q: Why would an insurance company file an Insurer's Petition for External Review?
A: An insurance company may file an Insurer's Petition for External Review to request an independent evaluation of a denied health care claim and to provide an opportunity for a fair and impartial review.
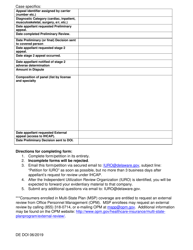
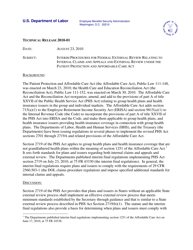
Q: How does Delaware's Independent Health Care Appeals Program work?
A: Delaware's Independent Health Care Appeals Program provides a formal process for consumers to appeal decisions made by their health insurance company. It involves the review of the denied claim by an independent third party, who will make a decision based on the available evidence.
Q: What happens after an Insurer's Petition for External Review is filed?
A: After an Insurer's Petition for External Review is filed, the independent reviewer will evaluate the denied claim and make a decision. The insurance company must comply with the reviewer's decision, which is binding.
Q: How long does the external review process take?
A: The length of the external review process can vary, but typically it should be completed within 45 days from the receipt of all necessary information.
Q: Can consumers file their own appeals under Delaware's Independent Health Care Appeals Program?
A: Yes, consumers can file their own appeals under Delaware's Independent Health Care Appeals Program. They can request an External Review Application form from the Delaware Department of Insurance or their health insurance company.
Q: Is there a cost associated with filing an Insurer's Petition for External Review?
A: No, there is no cost to the insurance company for filing an Insurer's Petition for External Review.
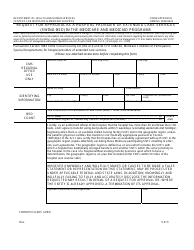
Form Details:
- Released on June 1, 2019;
- The latest edition currently provided by the Delaware Department of Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Delaware Department of Insurance.