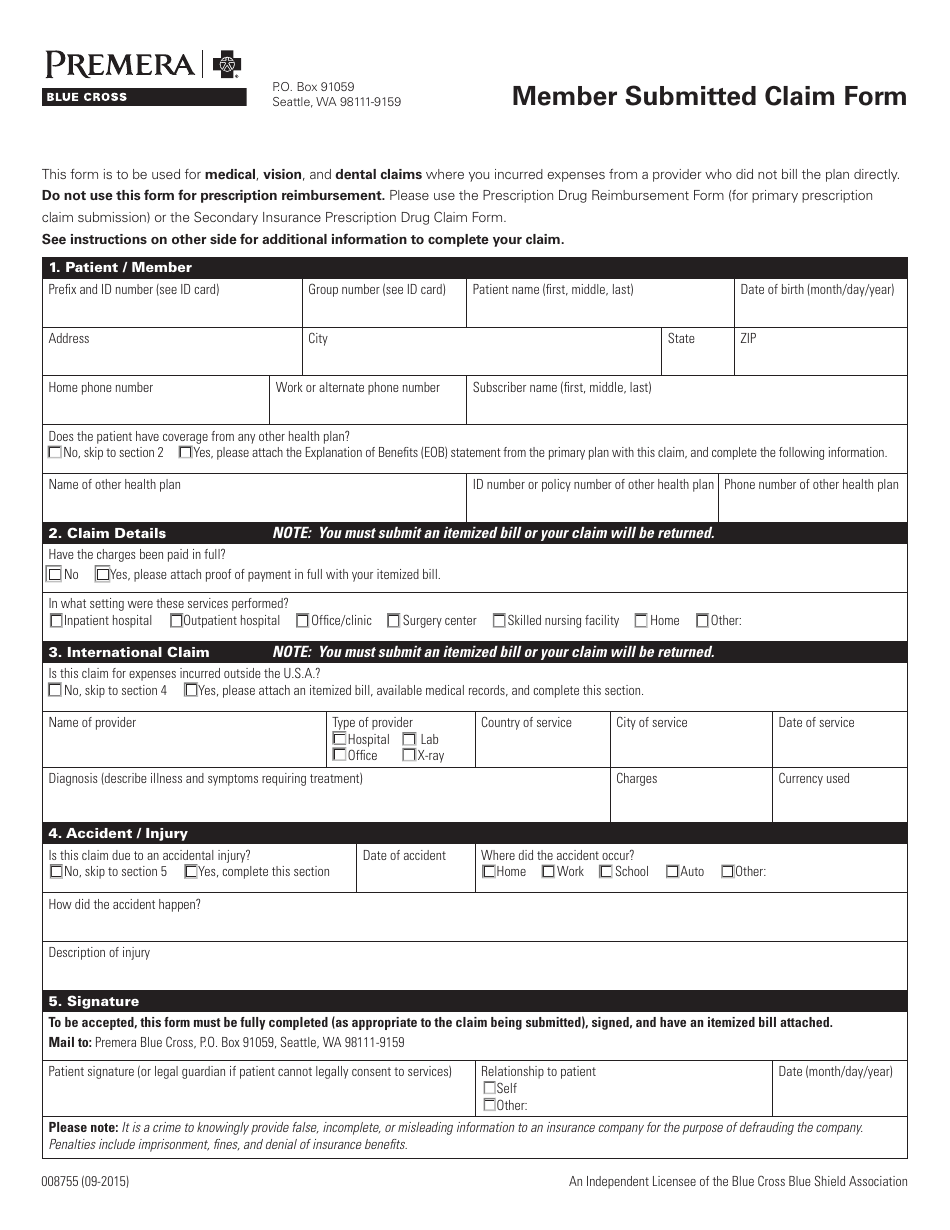
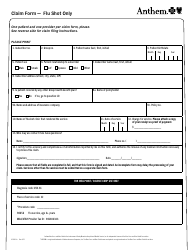
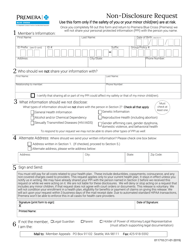
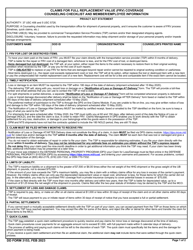
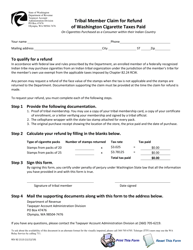
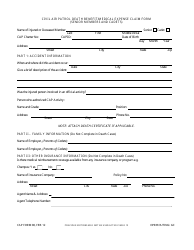
Form 008755 Member Submitted Claim Form - Premera Blue Cross - Washington
Form 008755 Member Submitted Claim Form - Premera Blue Cross - Washington is used for submitting healthcare claims to Premera Blue Cross in the state of Washington.
The individual member files the Form 008755 Member Submitted Claim Form with Premera Blue Cross in Washington.
FAQ
Q: What is Form 008755?
A: Form 008755 is a Member Submitted Claim Form.
Q: Who is it for?
A: It is for members of Premera Blue Cross in Washington.
Q: What is Premera Blue Cross?
A: Premera Blue Cross is a health insurance company.
Q: What is the purpose of the Member Submitted Claim Form?
A: The form is used to submit claims for reimbursement of medical expenses.
Q: How can I obtain Form 008755?
A: You can obtain the form from Premera Blue Cross.
Q: Does the form have any specific requirements?
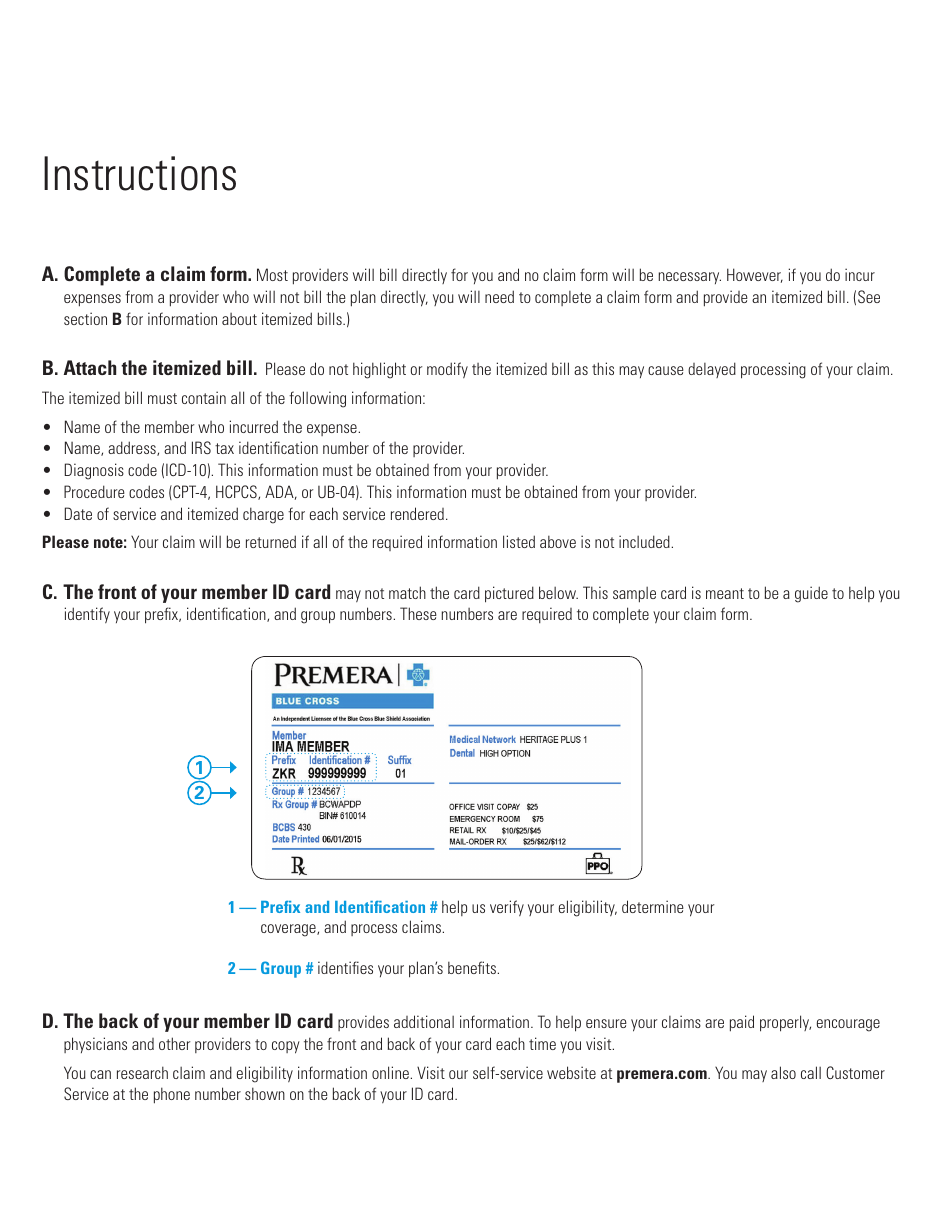
A: Yes, there are certain instructions and requirements mentioned on the form.
Q: Can I use this form for claims from providers outside of Washington?
A: No, this form is specifically for claims in Washington.
Q: What should I do after completing the form?
A: After completing the form, you need to submit it to Premera Blue Cross for processing.
Q: Is there a deadline for submitting the form?
A: It is recommended to submit the form as soon as possible after receiving services, but there may be a deadline specified by Premera Blue Cross.