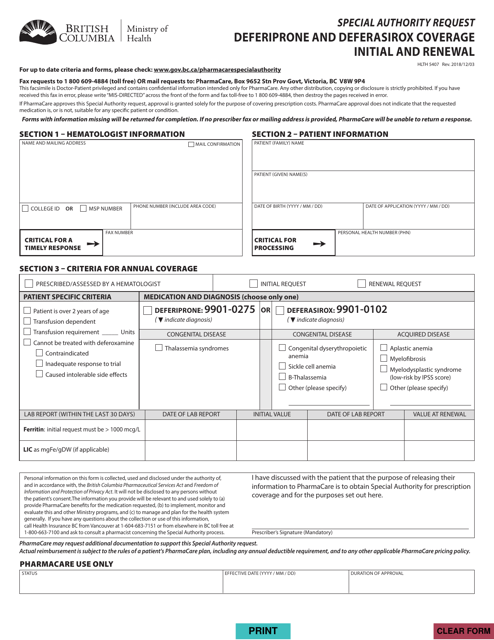
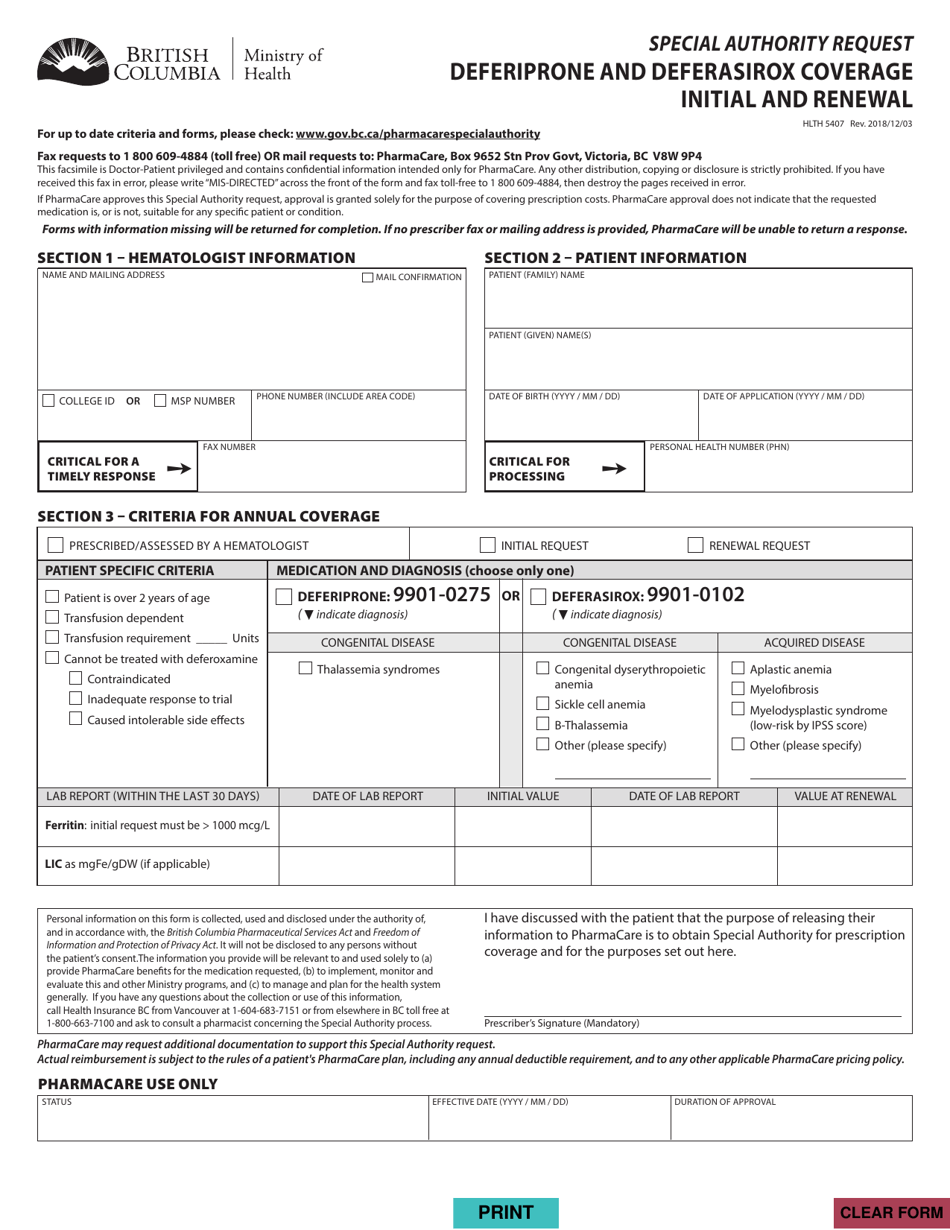
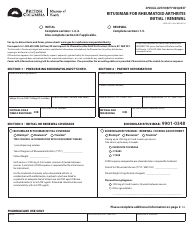
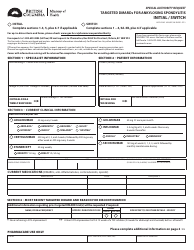
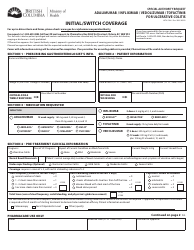
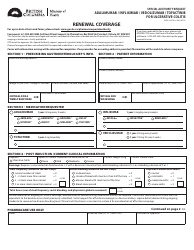
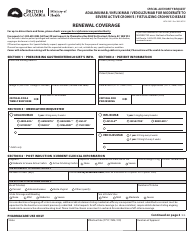
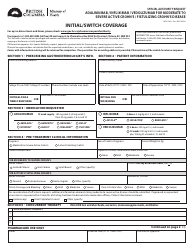
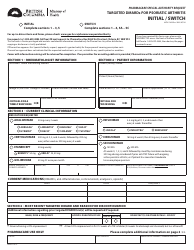
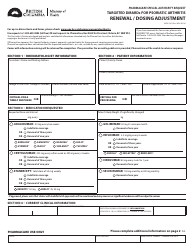
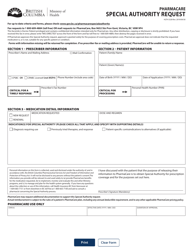
Form HLTH5407 Special Authority Request - Deferiprone and Deferasirox Coverage Initial and Renewal - British Columbia, Canada
Form HLTH5407 Special Authority Request - Deferiprone and Deferasirox Coverage Initial and Renewal is used in British Columbia, Canada to request coverage for the medications Deferiprone and Deferasirox. These medications are used in the treatment of certain conditions, such as iron overload, and require special authorization from the provincial health authorities for coverage.
The form HLTH5407 Special Authority Request - Deferiprone and Deferasirox Coverage Initial and Renewal in British Columbia, Canada is filed by the healthcare provider or the prescribing physician.
FAQ
Q: What is a special authority request?
A: A special authority request is a formal submission to the government to request coverage for a medication that is not automatically covered under the public drug plan.
Q: What is Deferiprone and Deferasirox?
A: Deferiprone and Deferasirox are medications used for the treatment of iron overload in certain medical conditions, such as thalassemia.
Q: Who is eligible for coverage under this special authority request?
A: Patients in British Columbia, Canada who have been diagnosed with iron overload and meet specific criteria may be eligible for coverage.
Q: How do I apply for a special authority request?
A: To apply for a special authority request, your healthcare provider needs to submit an application on your behalf. They will need to provide supporting documentation and complete the necessary forms.
Q: What criteria need to be met for a special authority request to be approved?
A: The specific criteria for approval may vary, but generally, patients need to have a confirmed diagnosis of iron overload, have tried and failed other treatments, and meet certain laboratory result criteria.
Q: Can I apply for a special authority request on my own?
A: No, you will need to work with your healthcare provider to apply for a special authority request.
Q: How long does it take to process a special authority request?
A: The processing time for a special authority request can vary, but it typically takes several weeks to receive a decision.
Q: If my special authority request is approved, what coverage will I receive?
A: If your special authority request is approved, you may receive coverage for the specific medication (Deferiprone or Deferasirox) as determined by the government.
Q: What happens if my special authority request is denied?
A: If your special authority request is denied, you may have options for appeals or alternative coverage pathways. You can discuss these options with your healthcare provider.
Q: Are there any costs associated with the special authority request process?
A: There may be costs associated with the special authority request process, such as fees for medical appointments or laboratory tests. It is best to check with your healthcare provider or the government for specific information.