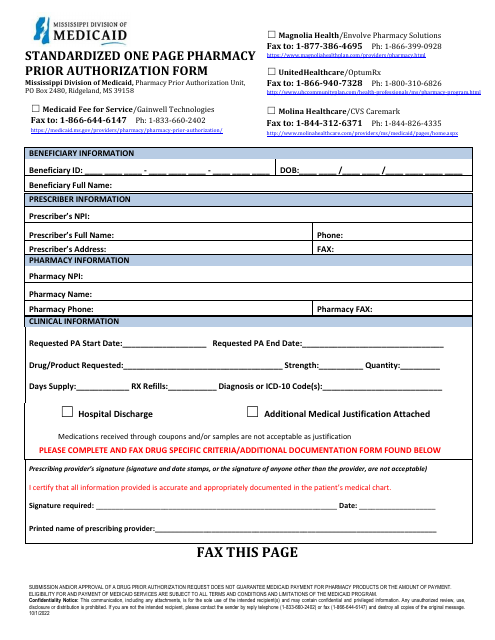
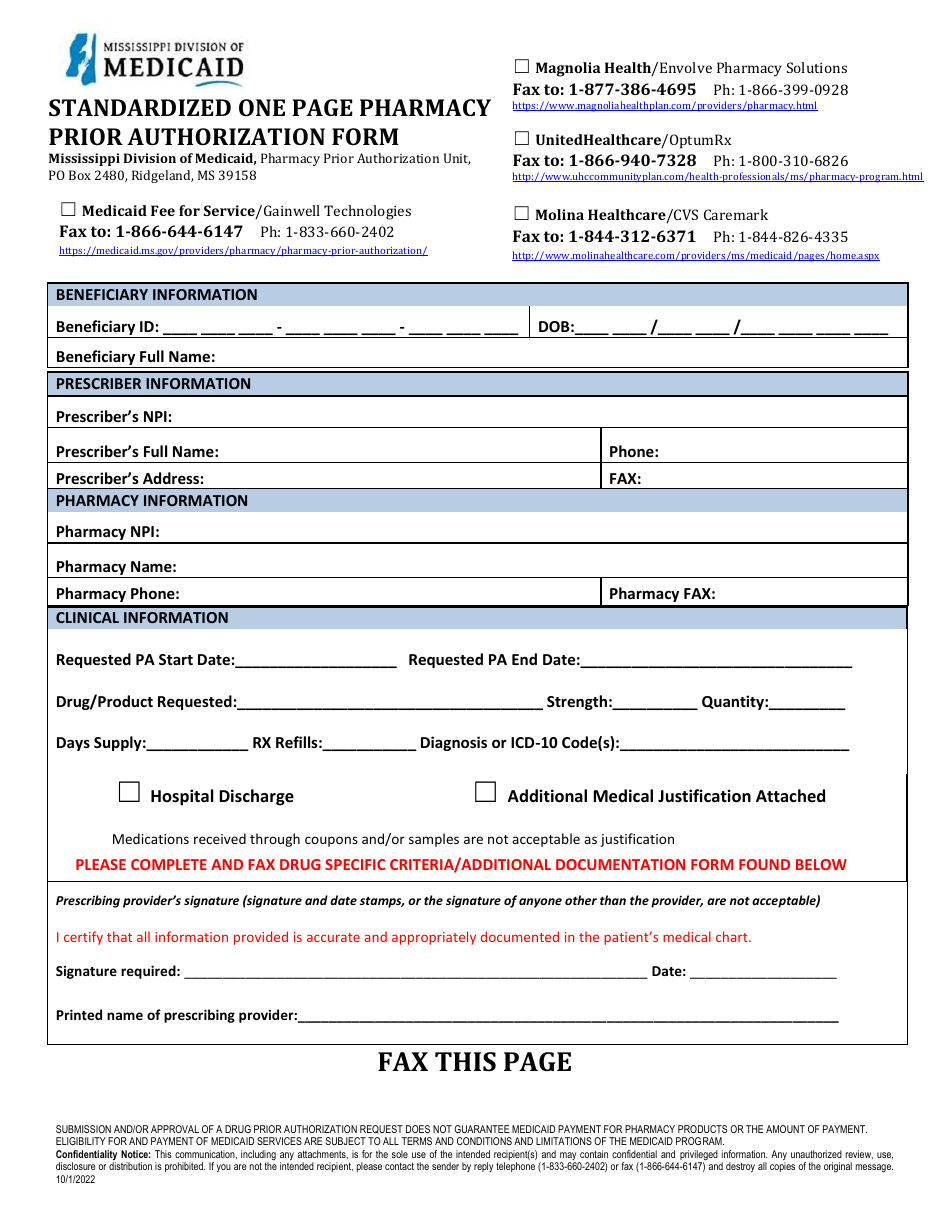
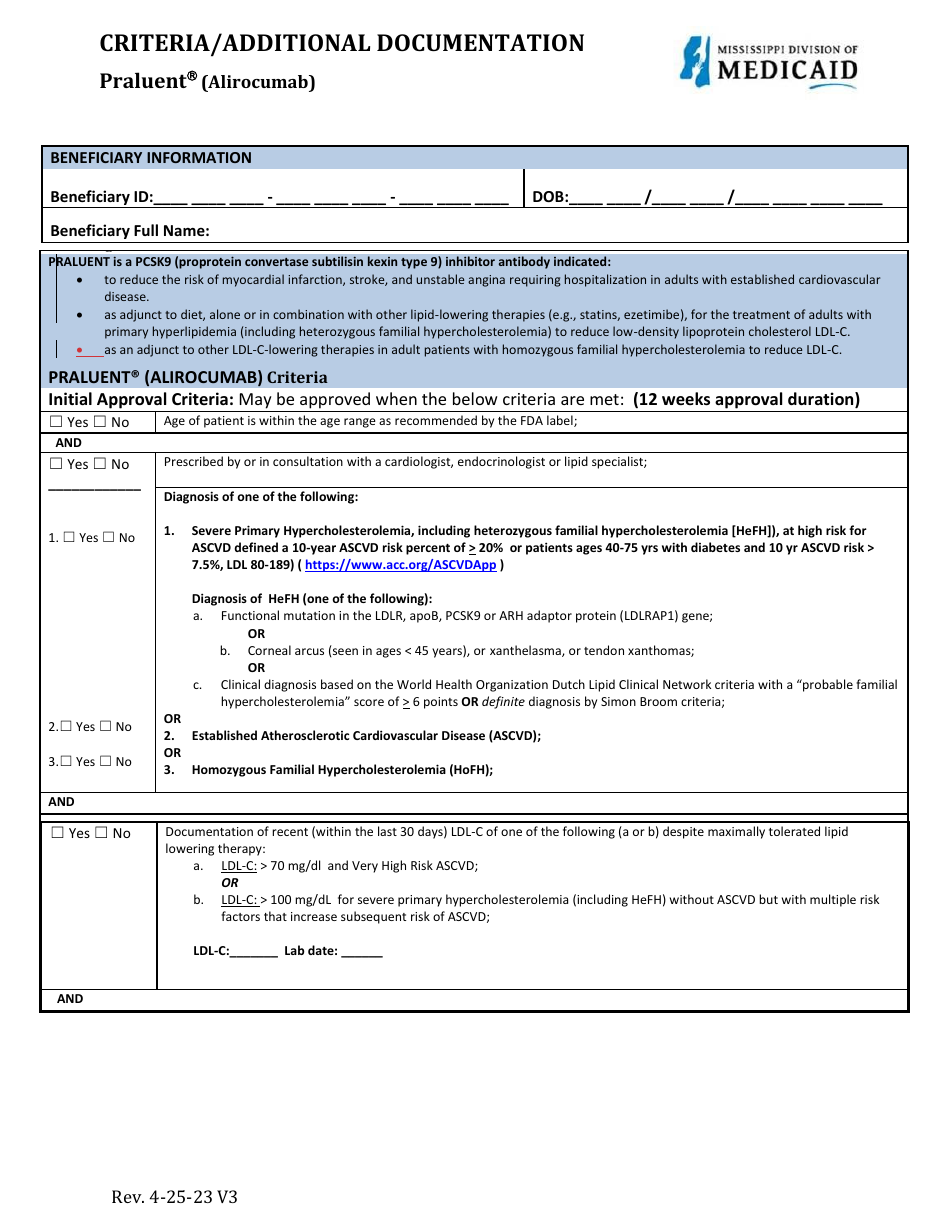
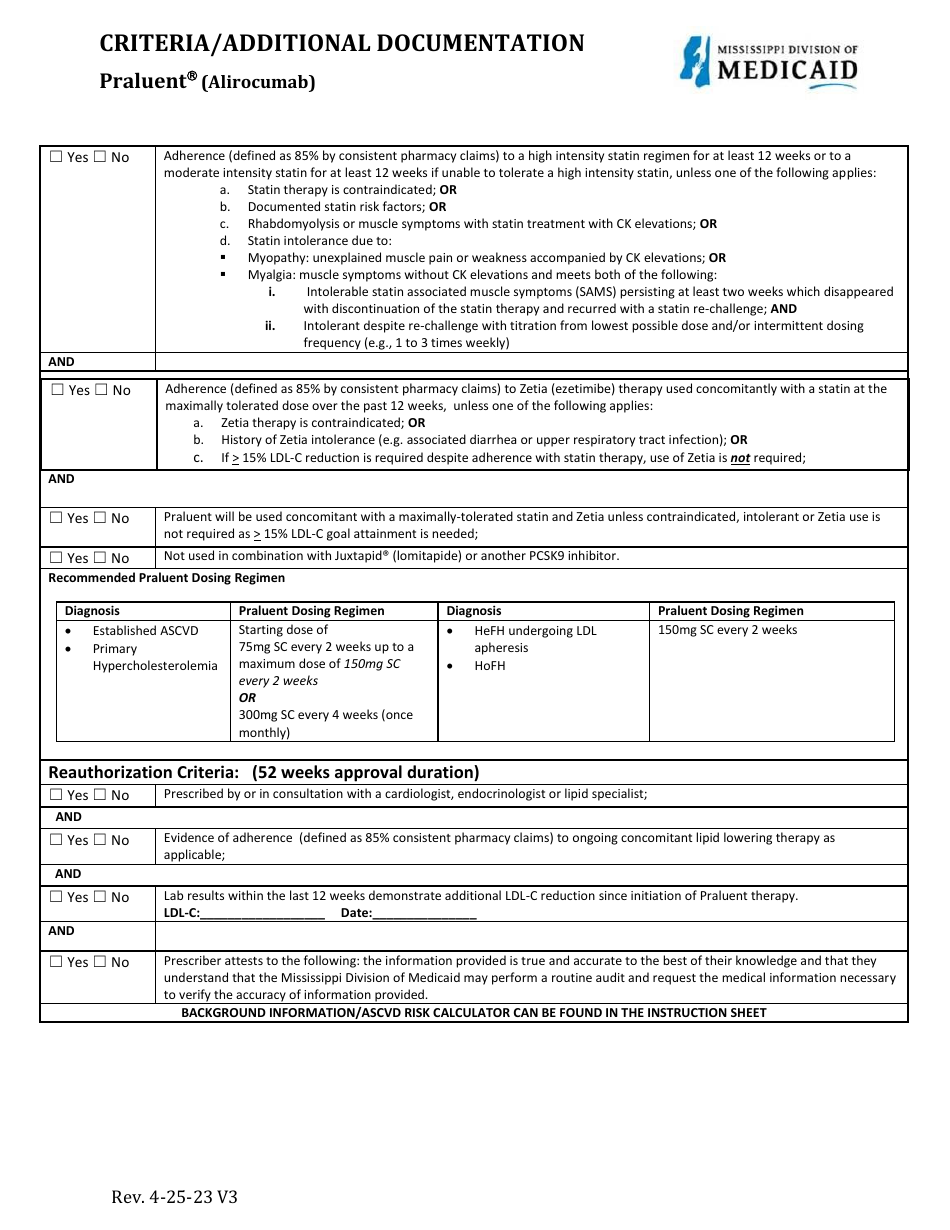
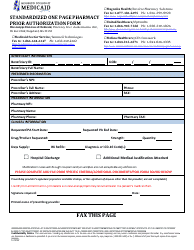
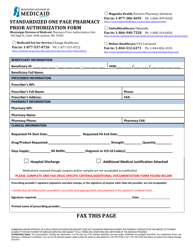
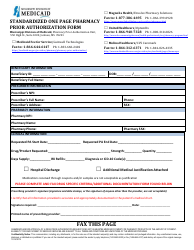
Standardized One Page Pharmacy Prior Authorization Form - Praluent (Alirocumab) - Mississippi
Standardized One Page Pharmacy Prior Authorization Form - Praluent (Alirocumab) is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is a pharmacy prior authorization form?
A: A pharmacy prior authorization form is a document that must be filled out by a healthcare provider to request coverage for a specific medication from an insurance company or pharmacy benefits manager.
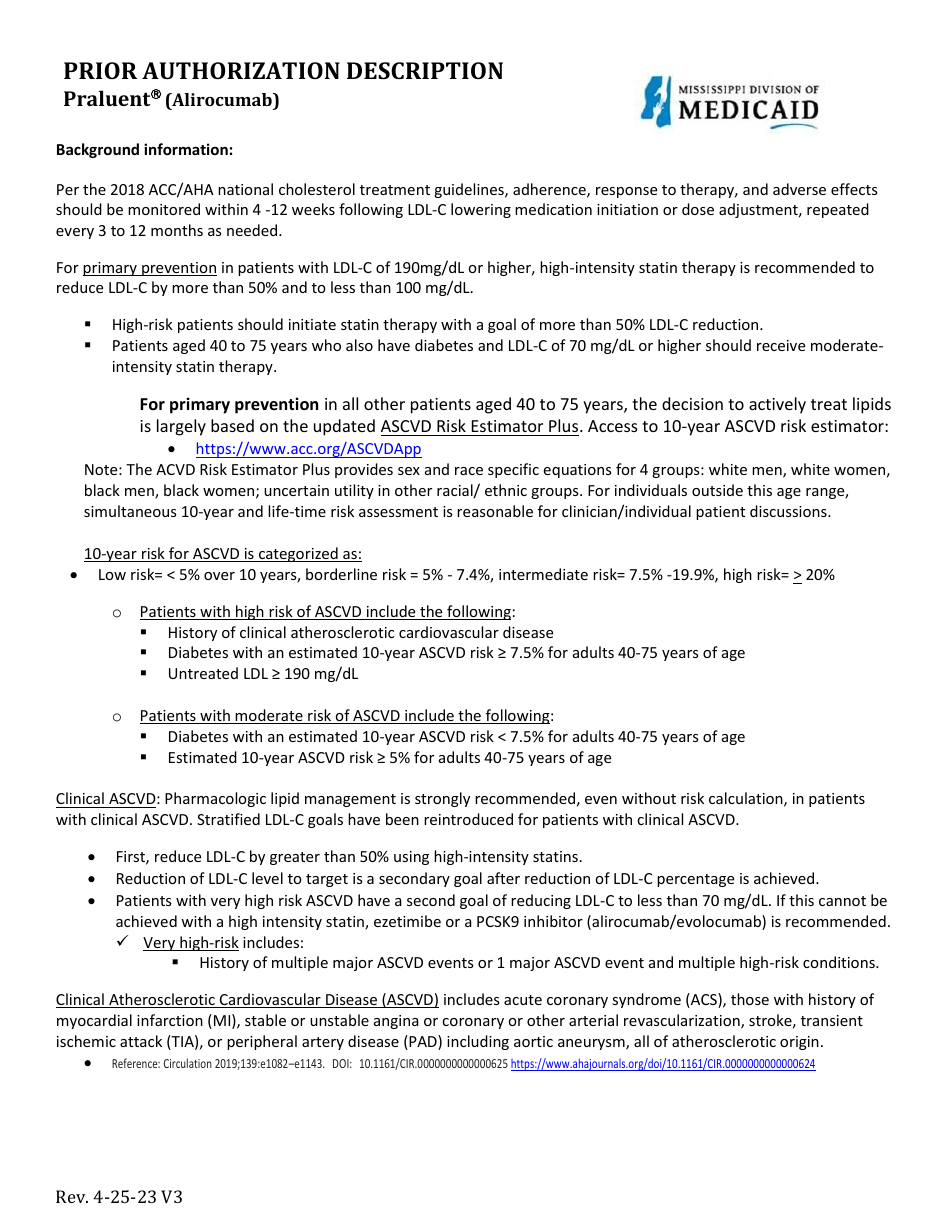
Q: What is Praluent (Alirocumab)?
A: Praluent (Alirocumab) is a medication used to lower cholesterol levels in individuals with familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease.
Q: Why is a prior authorization needed for Praluent?
A: A prior authorization is needed for Praluent to ensure that the medication is prescribed appropriately and that coverage will be provided by the insurance company.
Q: How can a healthcare provider obtain a pharmacy prior authorization form for Praluent?
A: Healthcare providers can obtain a pharmacy prior authorization form for Praluent from the insurance company or pharmacy benefits manager.
Q: What information is typically required on a pharmacy prior authorization form?
A: A pharmacy prior authorization form typically requires information such as the patient's personal information, diagnosis, prescribed medication, and supporting clinical documentation.
Form Details:
- Released on April 25, 2023;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.