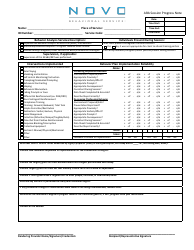
Mental Health Progress Note Template
Mental Health Progress Note Template: What Is It?
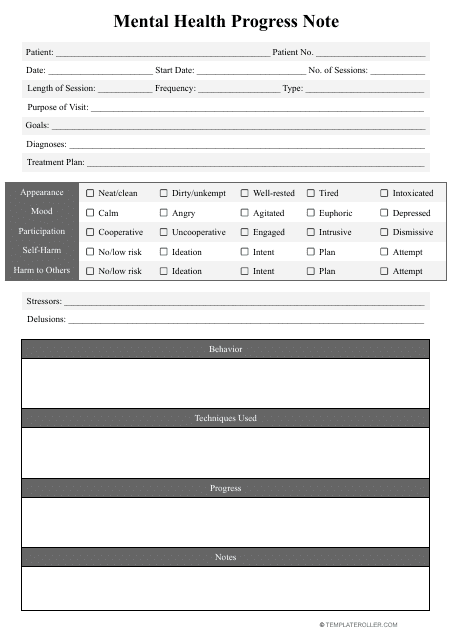
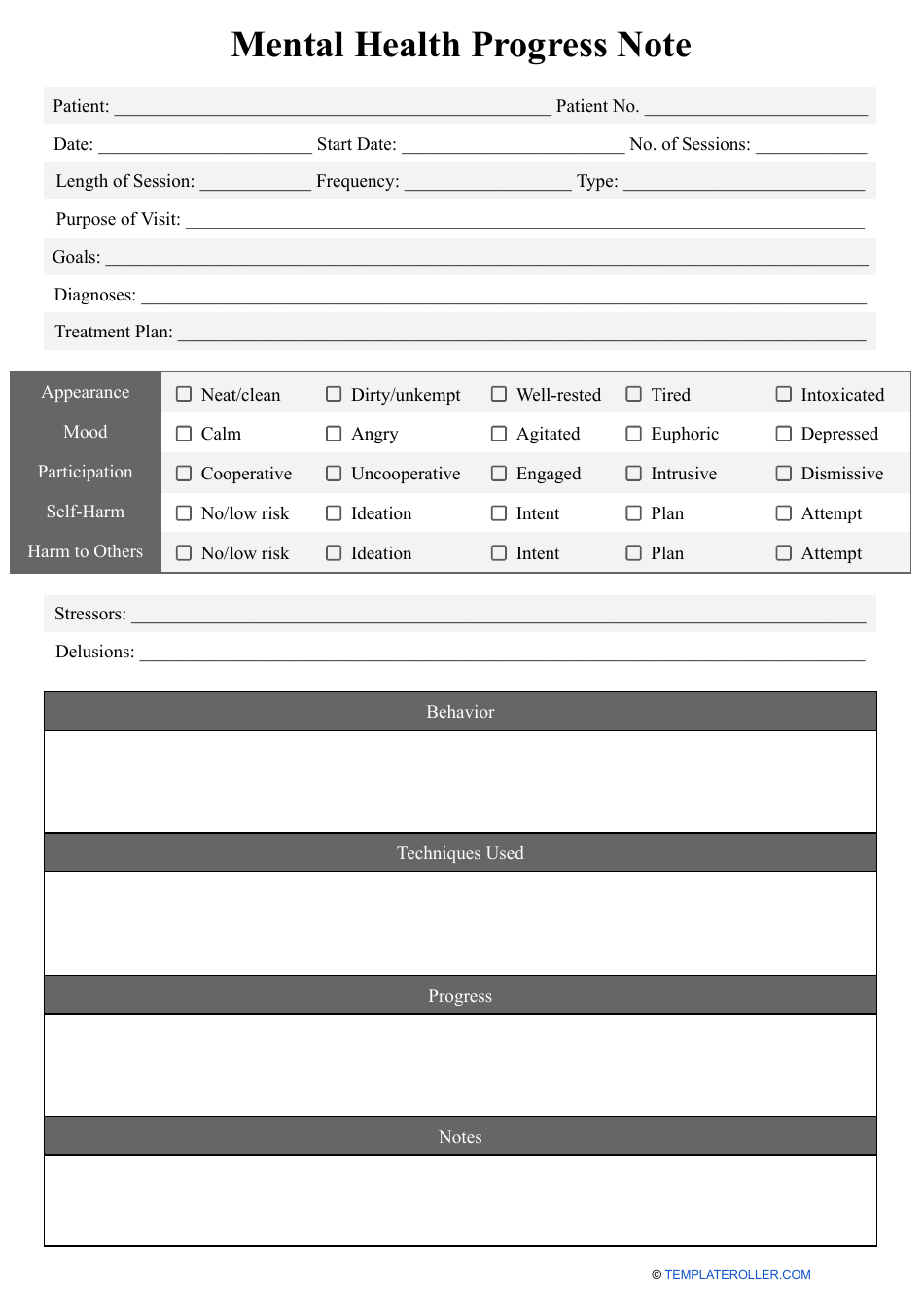
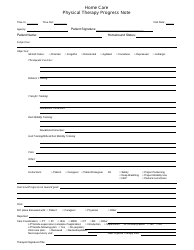
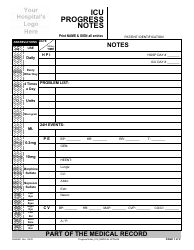
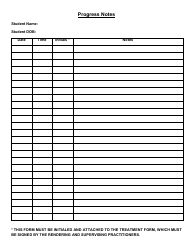
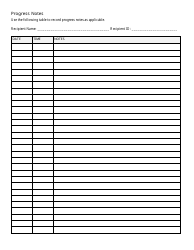
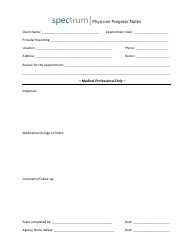
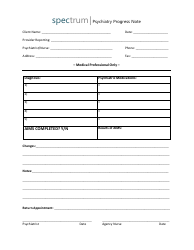
A Mental Health Progress Note Template is a standardized document required for documenting the progress of a patient receiving mental health treatment. The template typically contains segments for identifying information, assessing the obtained information, forming a diagnosis, creating a treatment plan, and keeping progress notes.
The identifying information section may request the individual's name, age, gender, and contact information. The assessment section may include the patient's current symptoms, mental status exam, and any relevant medical history. The diagnosis section will include a formal diagnosis. The treatment plan section may include goals, interventions and medication.
A Mental Health Progress Note template can be downloaded by clicking the link below.
Progress notes for mental health are where the clinician documents the patient's progress over time. This section may include information about:
- The individual’s response to treatment;
- Details about any changes in symptoms;
- Records of adverse effects from medication.
Any standard Mental Health Progress Note should be concise, objective, and centered on the individual’s goals.
It is worth noting that the content and format of a mental health progress note template may vary depending on the setting and the specific requirements of the individual. The template should be designed to facilitate accurate and effective recording of the individual’s development, while also protecting the patient's privacy and confidentiality.
How to Write Mental Health Progress Notes?
Mental Health Progress Notes are an essential part of documenting a patient's treatment and progress. They provide a comprehensive record of the patient's mental health history, diagnosis, treatment plan, and progress towards recovery. Here are some tips on how to write effective mental health progress notes:
-
Start with the basics : Record the date, time, and location of the session, as well as the patient's name, age, and gender;
-
Objective observations : Record objective observations of the patient's behavior, mood, speech, and appearance during the session. This includes any changes in symptoms, behaviors, or emotions since the last session;
-
Treatment plan : Document any changes to the patient's treatment plan, including medication adjustments, therapy goals, and any new interventions;
-
Progress towards goals : Note the patient's progress towards their therapy goals and any challenges they may be facing. This could include improvements in mood, behavior, or relationships, as well as setbacks or difficulties;
-
Risk assessment : Assess the patient's risk of harm to themselves or others and document any safety concerns. This includes any suicidal or homicidal ideation, self-harm behaviors, or substance abuse;
-
Collaboration with other providers : If the patient is receiving treatment from other providers, document any collaboration or communication with those providers;
-
Plan for next session : End the note with a plan for the next session, including any homework or goals for the patient to work on.
It's important to remember that progress notes are legal documents and should be detailed, precise, and objective. Avoid using subjective language or making assumptions about the patient's thoughts or feelings. Stick to the facts and document any changes or concerns related to the patient's mental health treatment.
Haven't found the template you're looking for? Take a look at the related templates below:
- Nursing Progress Note Template;
- Psychotherapy Progress Note Template;
- Nursing Care Plan Template.