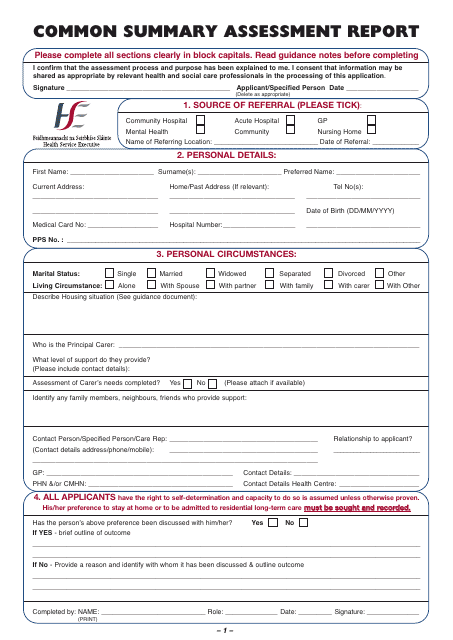
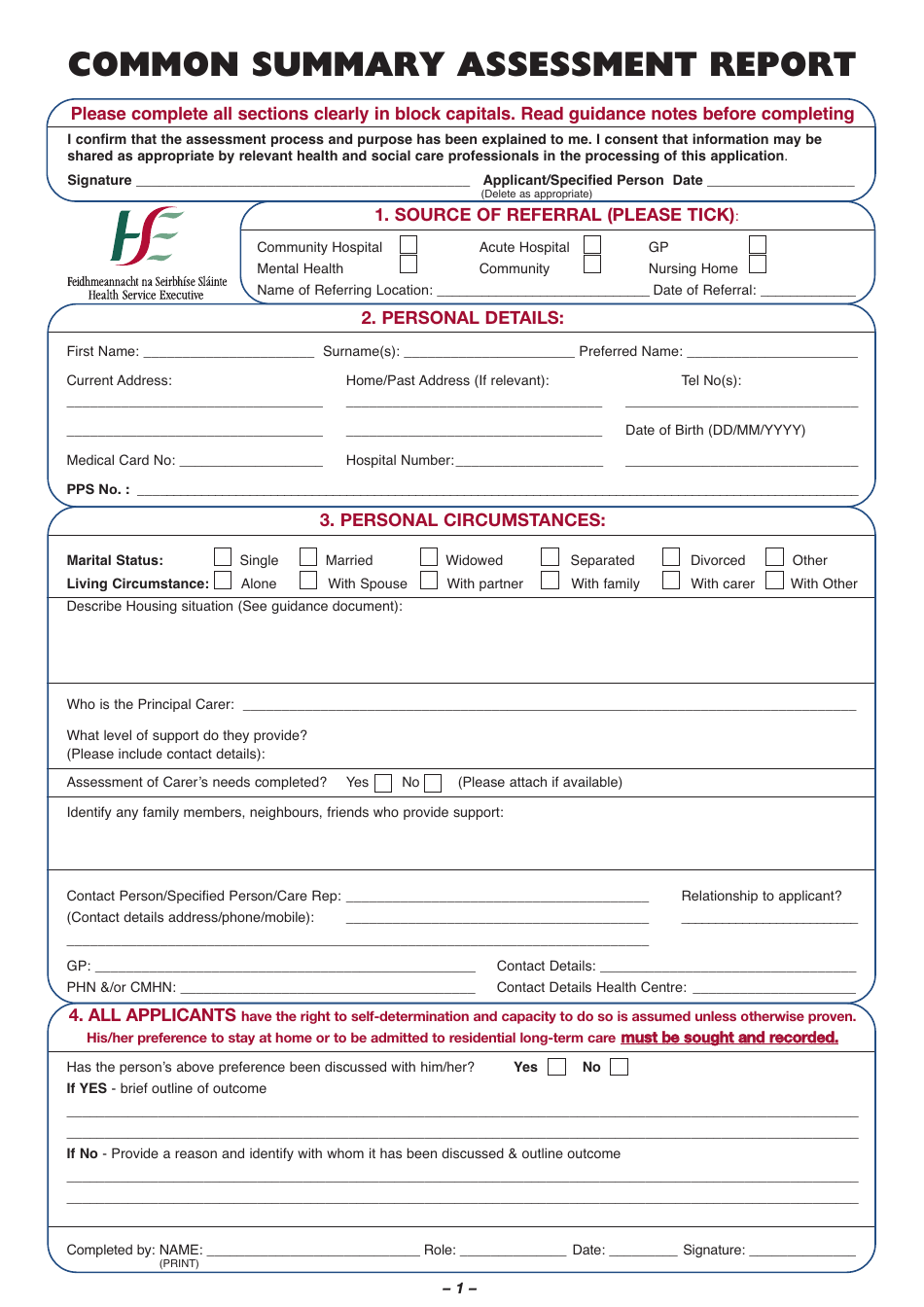
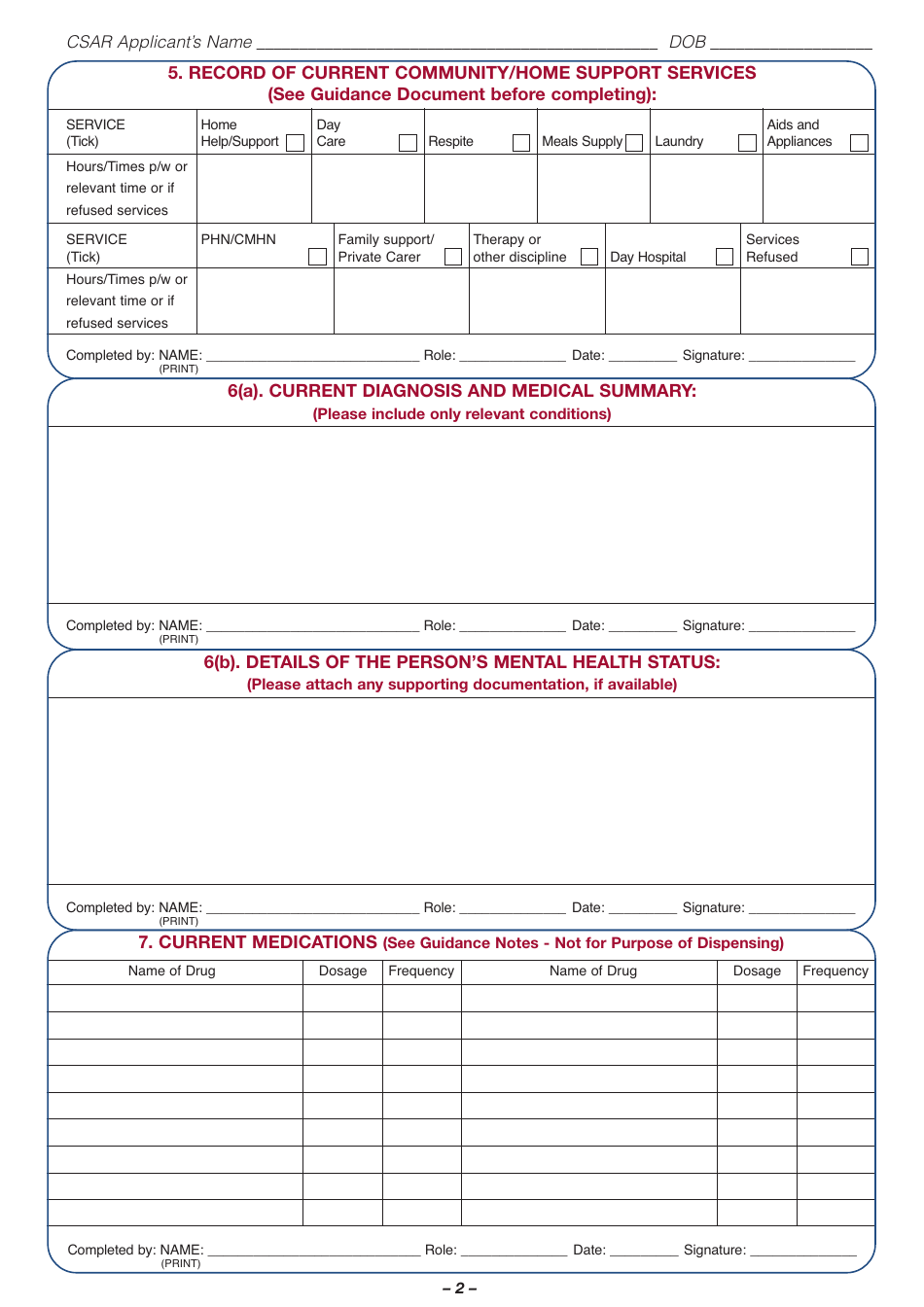
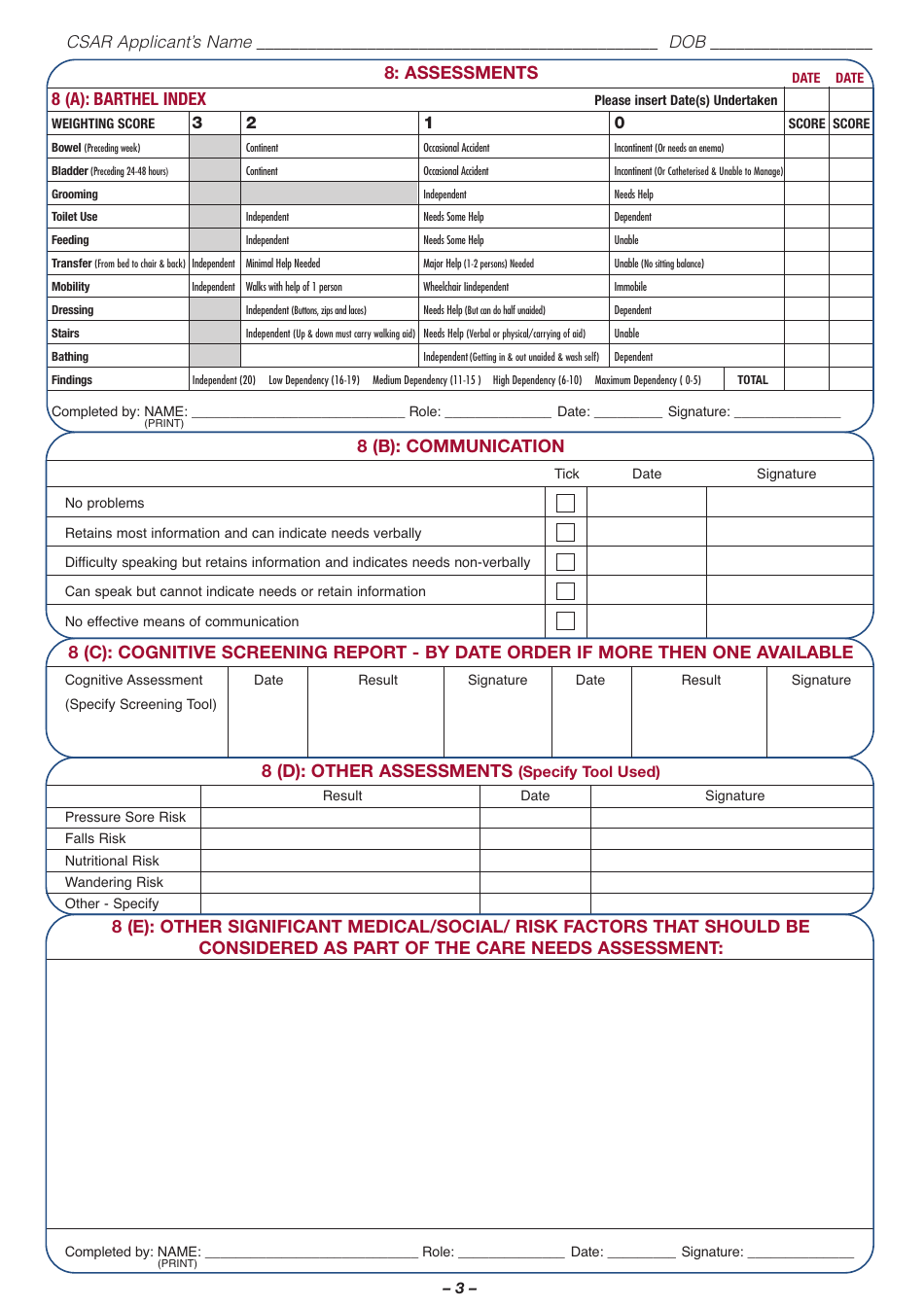
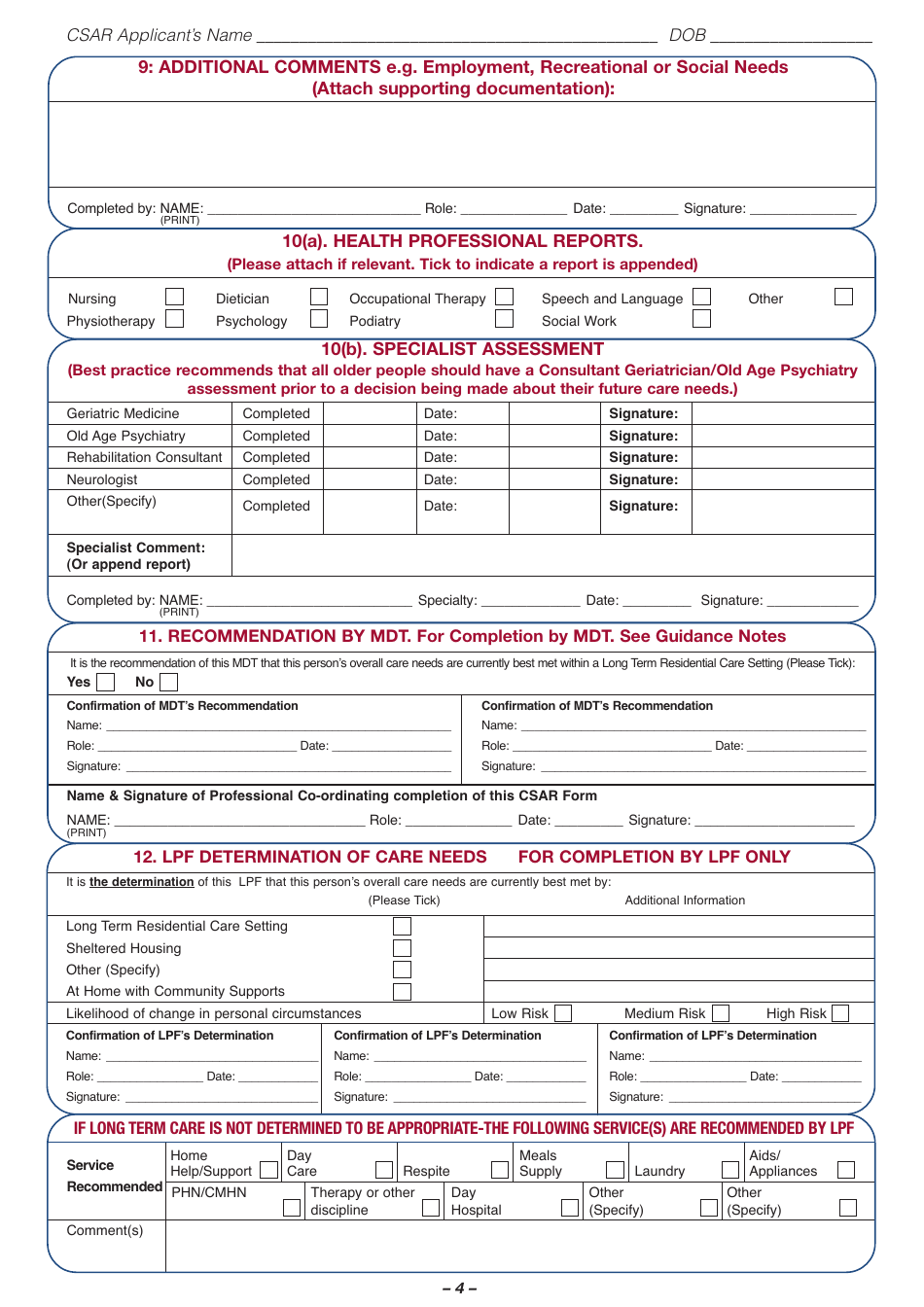
Common Summary Assessment Report Form - Ireland
Fill PDF Online
Fill out online for free
without registration or credit card
This Ireland-specific " Common Summary Assessment Report Form " is a document released by the Ireland's Health Services .
Download the fillable PDF by clicking the link below and use it according to the applicable legal guidelines.