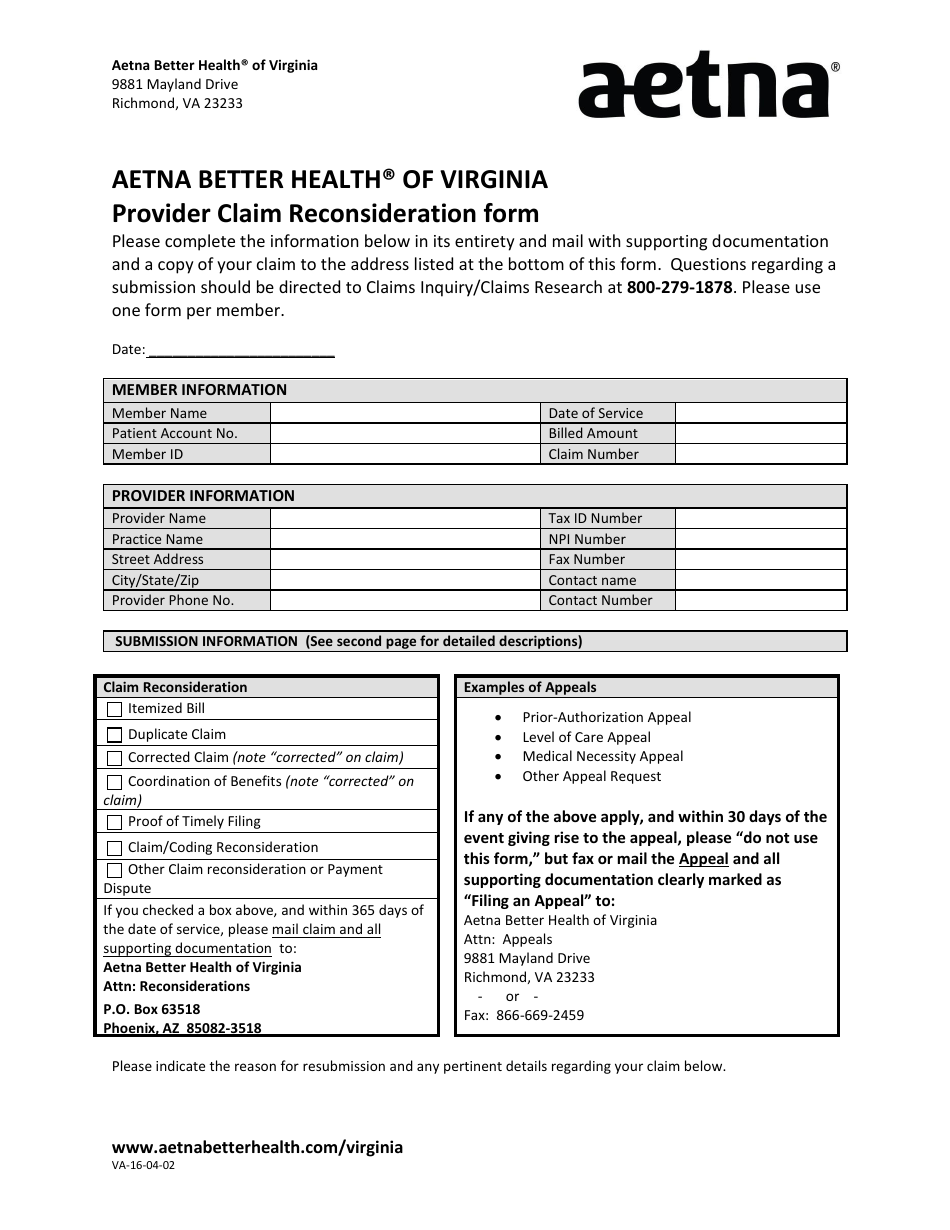
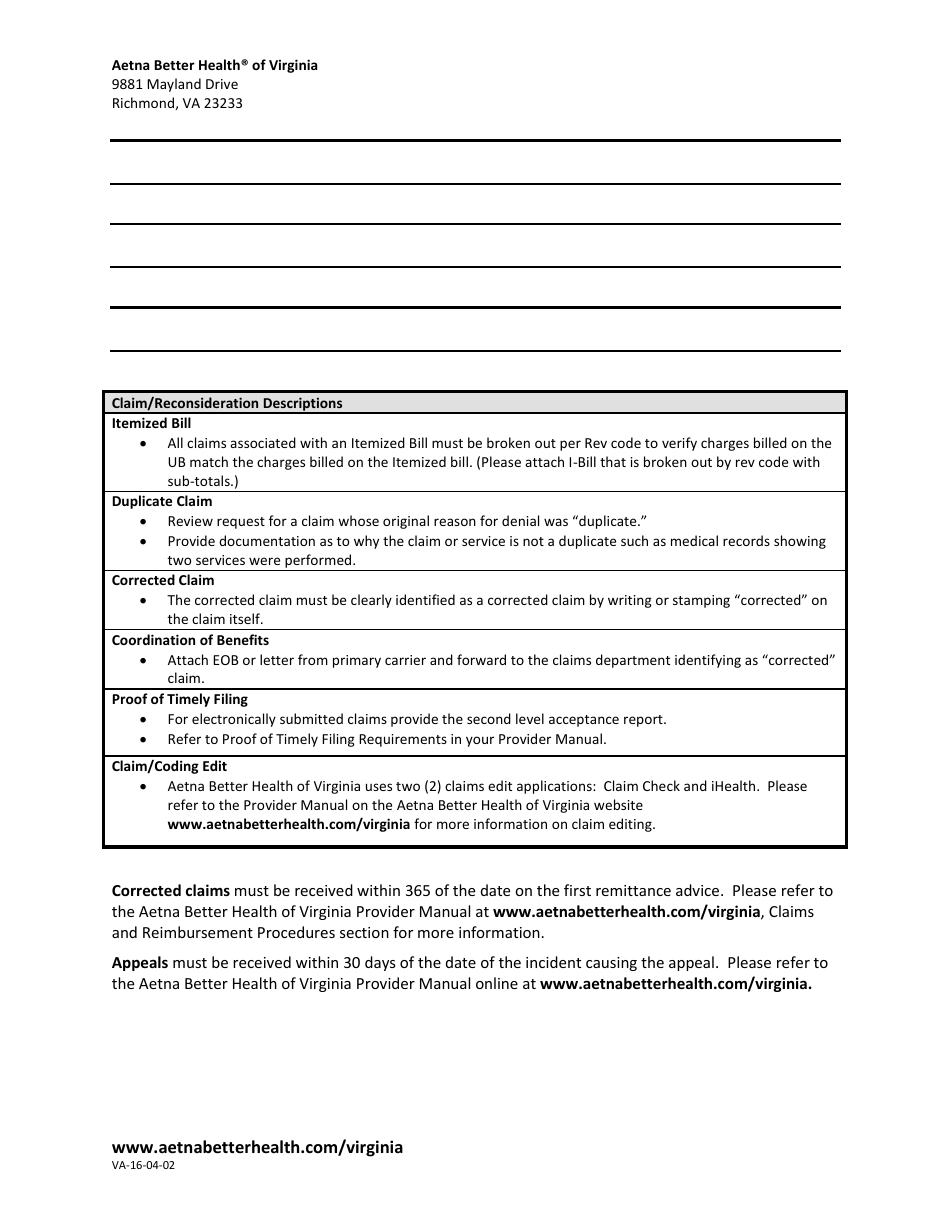
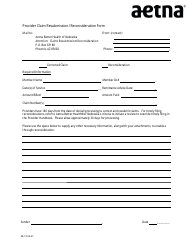
Form VA-16-04-02 Provider Claim Reconsideration
Fill PDF Online
Fill out online for free
without registration or credit card
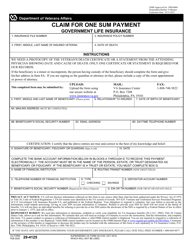
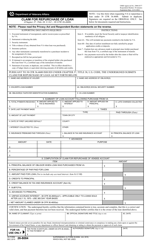
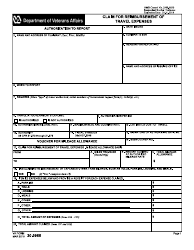
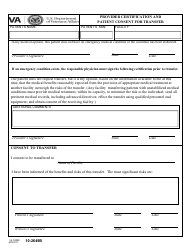
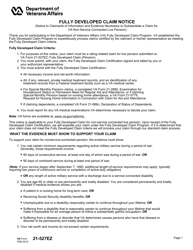
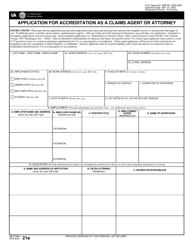
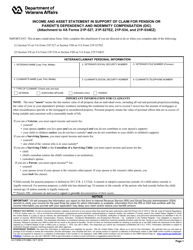
What Is Form VA-16-04-02?
This is a legal form that was released by the CVS Health Corporation - Aetna on April 16, 2002 and used country-wide. As of today, no separate filing guidelines for the form are provided by the issuing department.
Form Details:
- Released on April 16, 2002;
- The latest available edition released by the CVS Health Corporation - Aetna;
- Easy to use and ready to print;
- Yours to fill out and keep for your records;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of Form VA-16-04-02 by clicking the link below or browse more documents and templates provided by the CVS Health Corporation - Aetna.