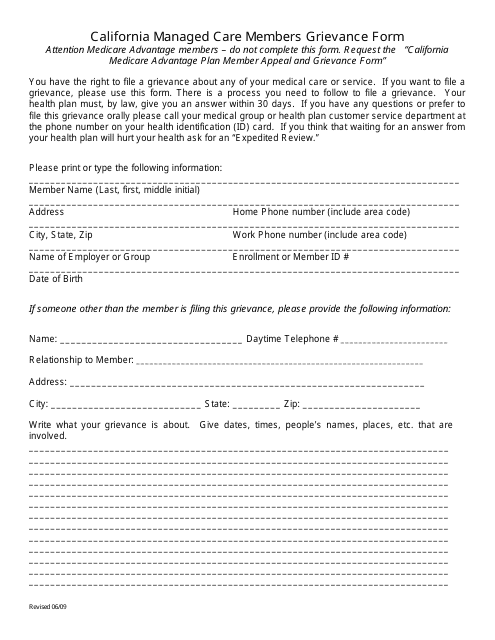
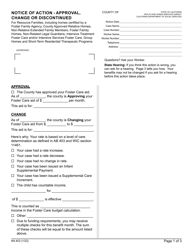
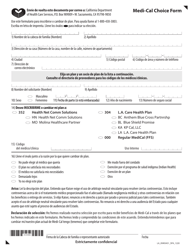
California Managed Care Members Grievance Form - California
California Managed Care Members Grievance Form is a legal document that was released by the California Department of Managed Health Care - a government authority operating within California.
FAQ
Q: What is the California Managed Care Members Grievance Form?
A: The California Managed Care Members Grievance Form is a form used by members of managed care plans in California to file a complaint or grievance.
Q: Who can use the California Managed Care Members Grievance Form?
A: Any member of a managed care plan in California can use the California Managed Care Members Grievance Form.
Q: What can I use the California Managed Care Members Grievance Form for?
A: You can use the California Managed Care Members Grievance Form to file a complaint or grievance about your managed care plan.
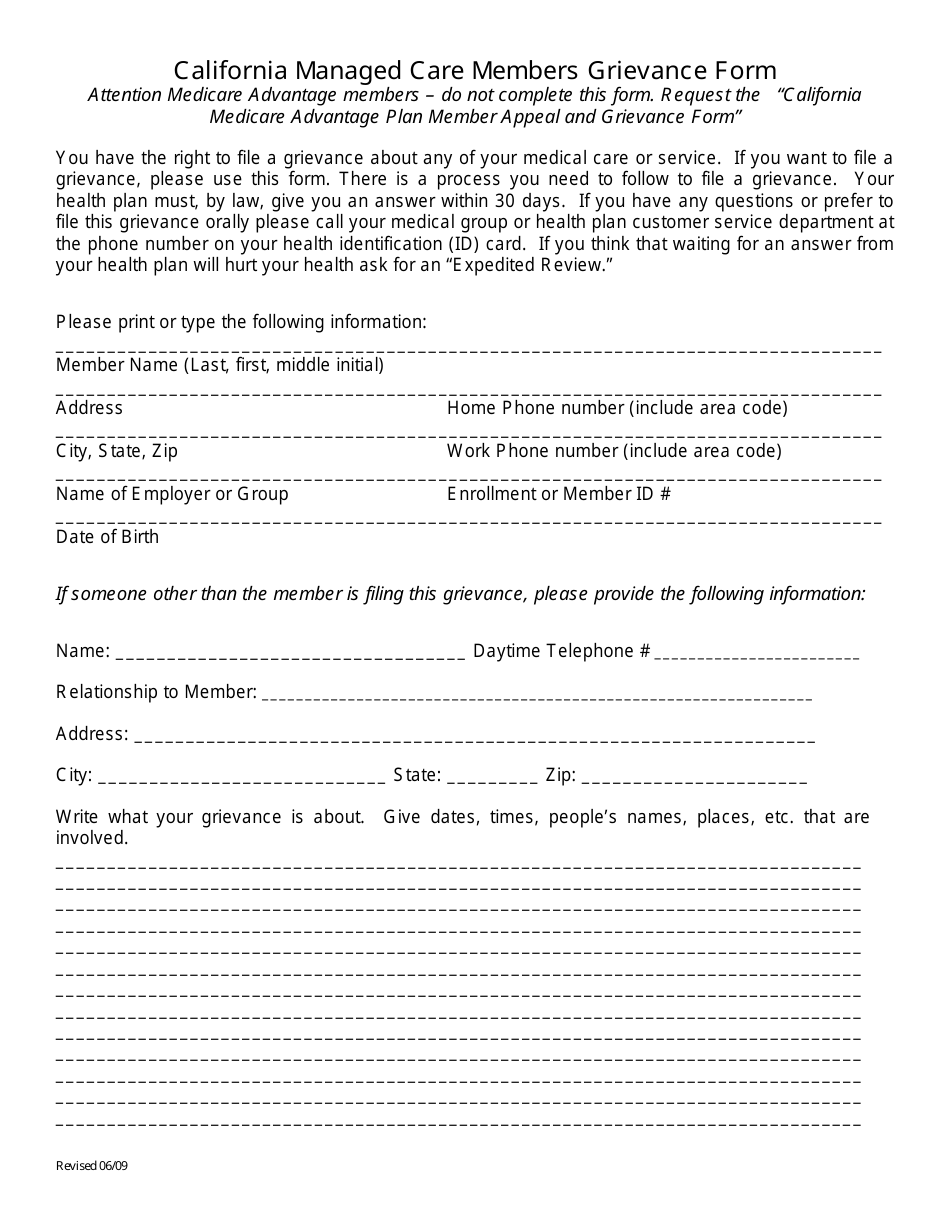
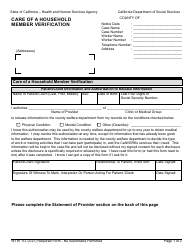
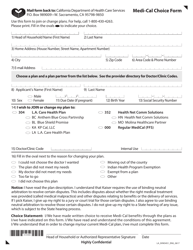
Q: What information do I need to provide on the California Managed Care Members Grievance Form?
A: You will need to provide your personal information, details about the complaint or grievance, and any supporting documentation.
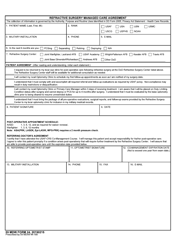
Q: What happens after I submit the California Managed Care Members Grievance Form?
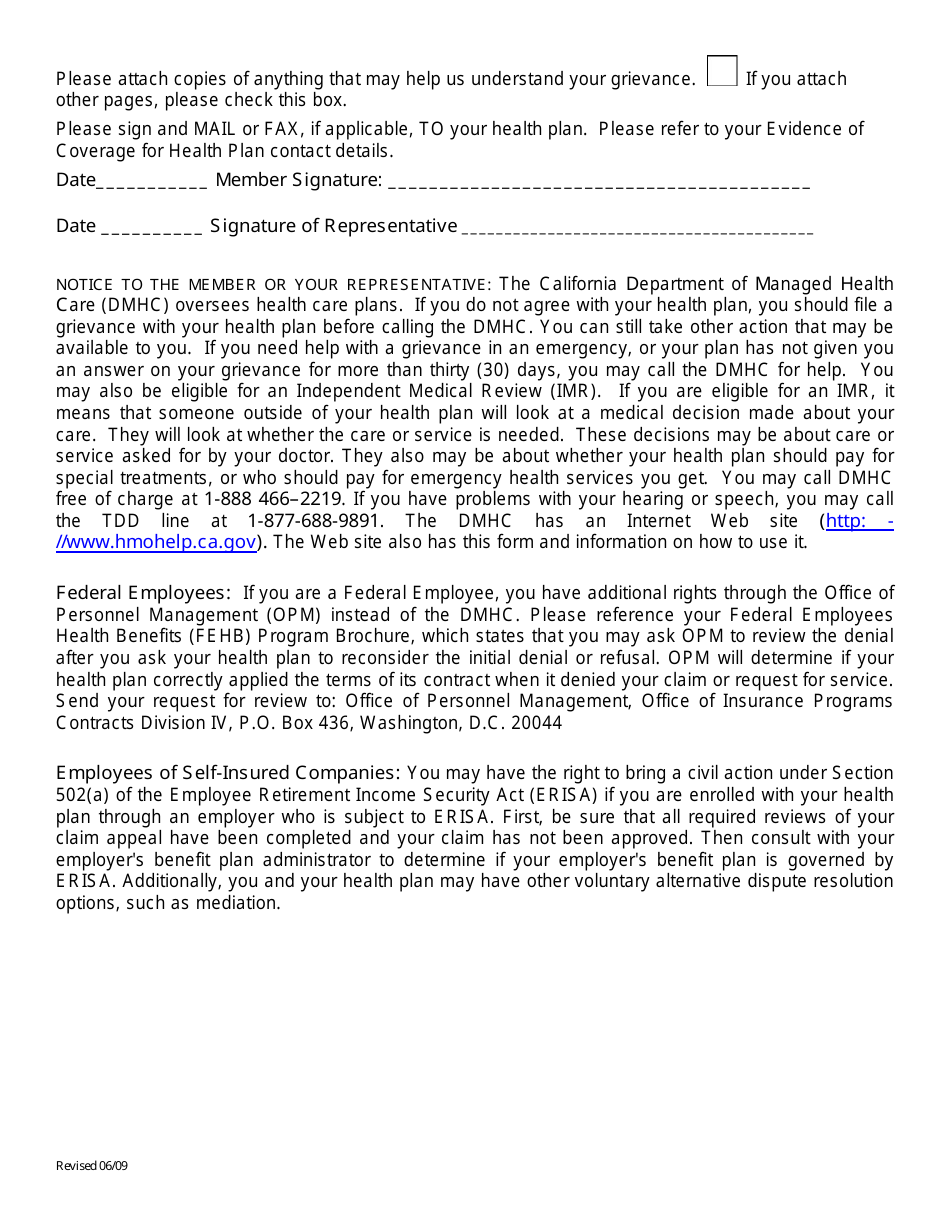
A: After you submit the California Managed Care Members Grievance Form, your managed care plan provider will review your complaint or grievance and respond to you within a certain timeframe.
Q: What if I am not satisfied with the response from my managed care plan provider?
A: If you are not satisfied with the response from your managed care plan provider, you can contact the California Department of Managed Health Care for further assistance.
Q: Is there a deadline for submitting the California Managed Care Members Grievance Form?
A: There is no specific deadline for submitting the California Managed Care Members Grievance Form, but it is recommended to file your complaint or grievance as soon as possible.
Q: Are there any fees associated with filing the California Managed Care Members Grievance Form?
A: No, there are no fees associated with filing the California Managed Care Members Grievance Form.
Form Details:
- Released on June 1, 2009;
- The latest edition currently provided by the California Department of Managed Health Care;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the California Department of Managed Health Care.