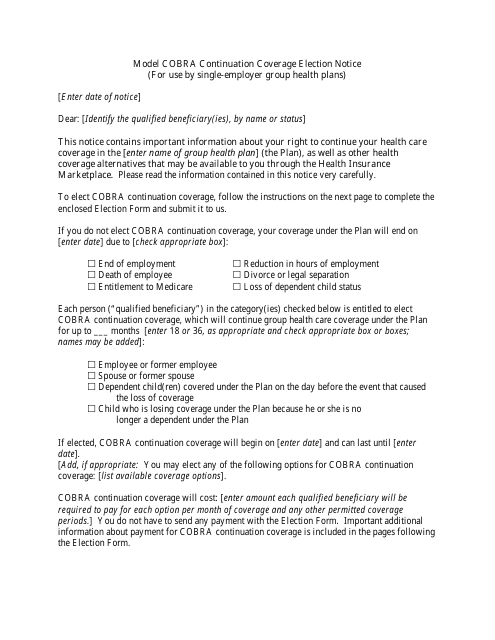
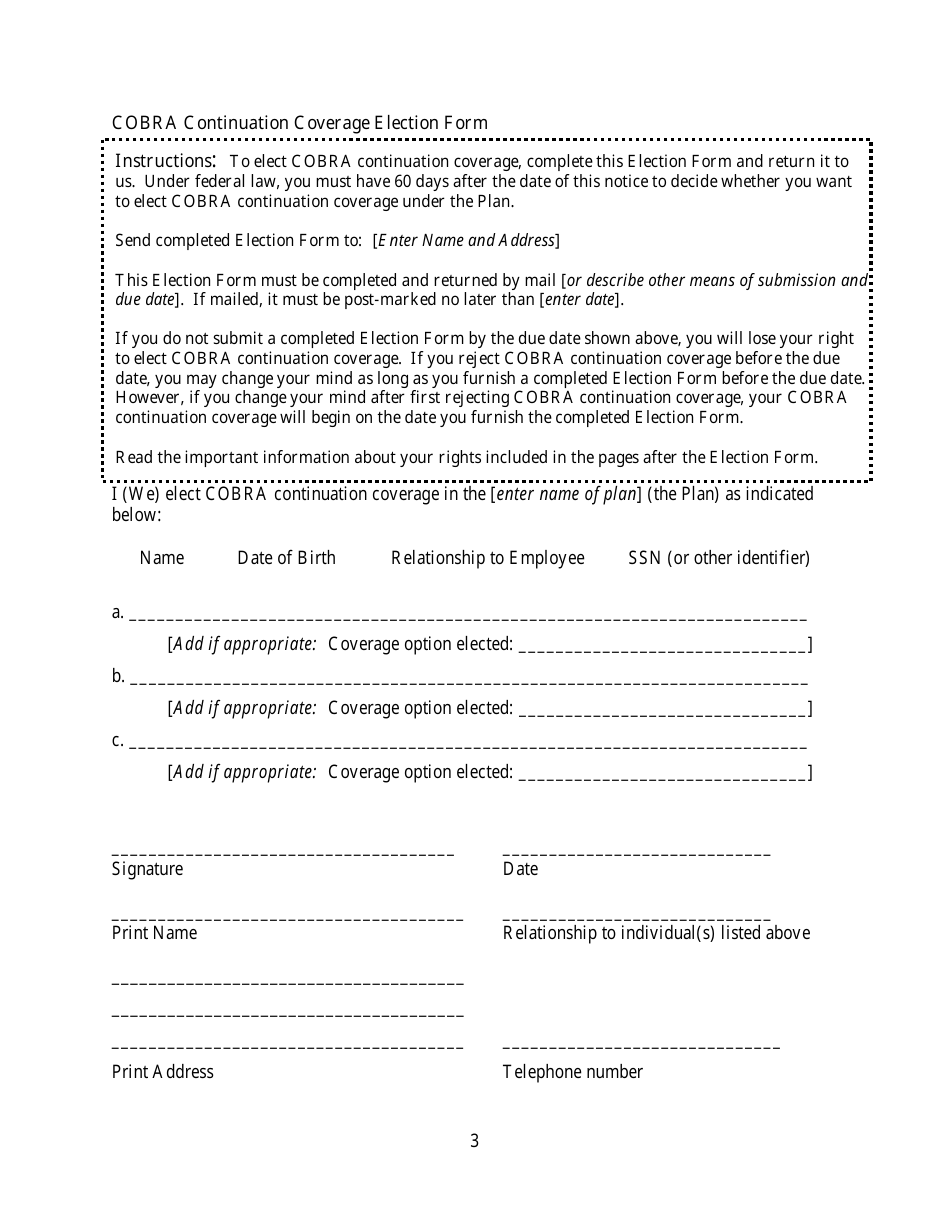
Model Cobra Continuation Coverage Election Notice Form
Model Cobra Continuation Coverage Election Notice Form is a 8-page legal document that was released by the U.S. Department of Labor and used nation-wide.
FAQ
Q: What is a Model Cobra Continuation Coverage Election Notice Form?
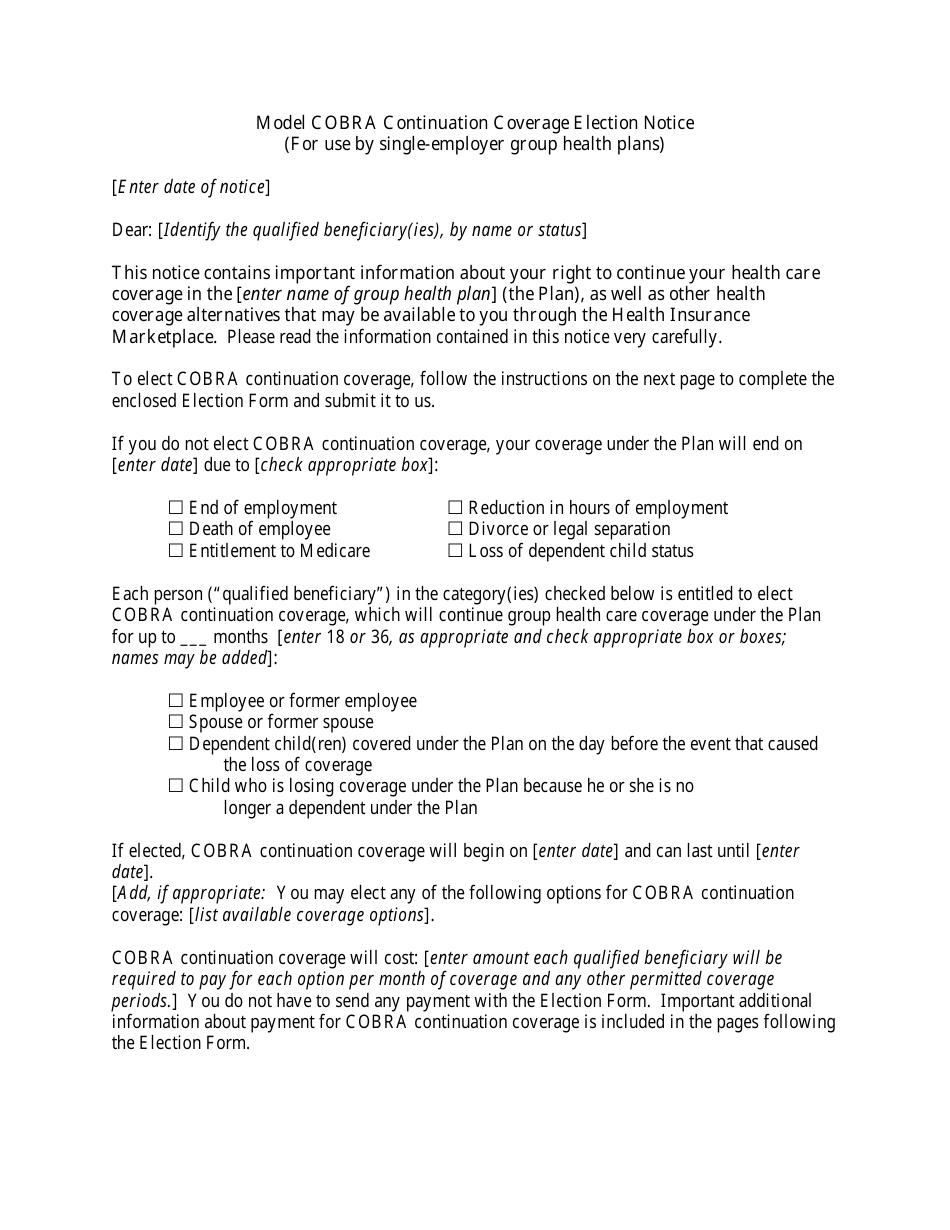
A: The Model Cobra Continuation Coverage Election Notice Form is a standard template provided by the Department of Labor to help employers comply with the notification requirements under COBRA.
Q: What is COBRA?
A: COBRA stands for Consolidated Omnibus Budget Reconciliation Act. It is a federal law that allows individuals to continue their employer-sponsored health insurance coverage for a limited period of time after certain qualifying events, such as job loss or divorce.
Q: Who needs to use the Model Cobra Continuation Coverage Election Notice Form?
A: Employers who are subject to COBRA regulations and are required to offer continuation coverage to their employees and their dependents must use the Model Cobra Continuation Coverage Election Notice Form or an equivalent notice that meets the requirements set by the Department of Labor.
Q: What does the Model Cobra Continuation Coverage Election Notice Form include?
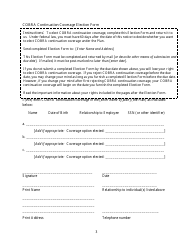
A: The form includes important information about the individual's rights and options for continuing their health insurance coverage under COBRA, such as how to elect coverage, the deadlines for making elections, and the costs associated with continuation coverage.
Form Details:
- The latest edition currently provided by the U.S. Department of Labor;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more legal forms and templates provided by the issuing department.