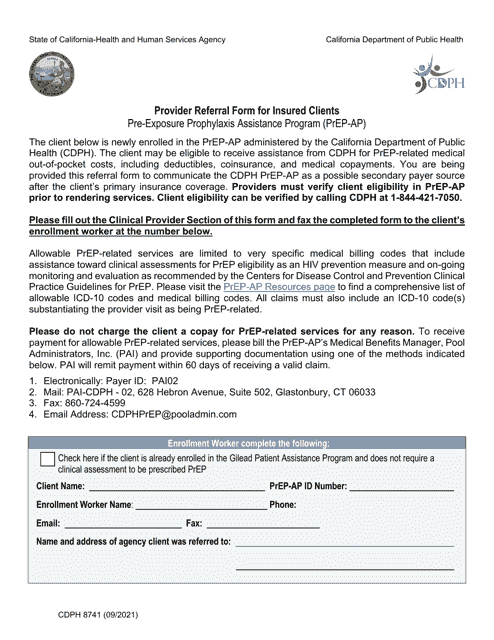
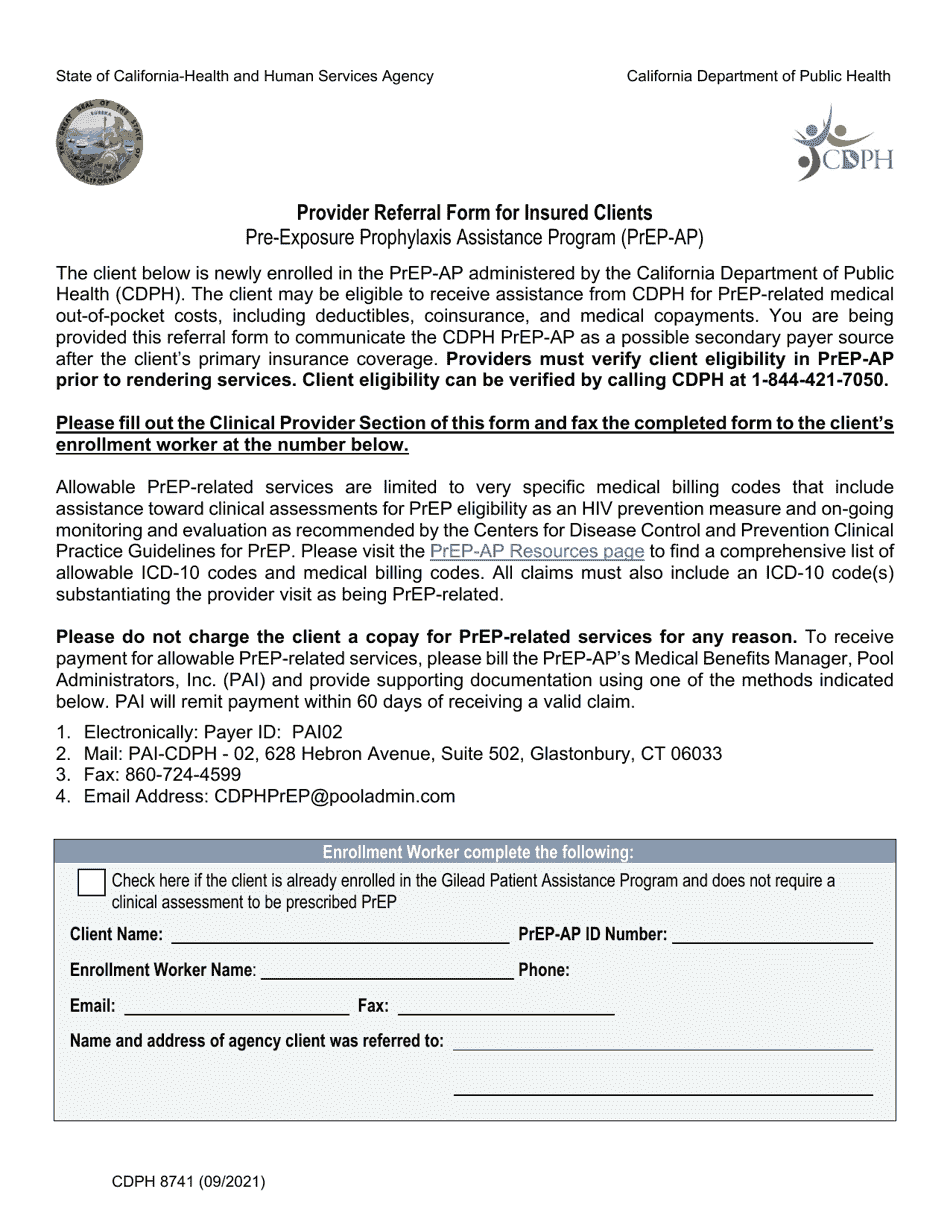
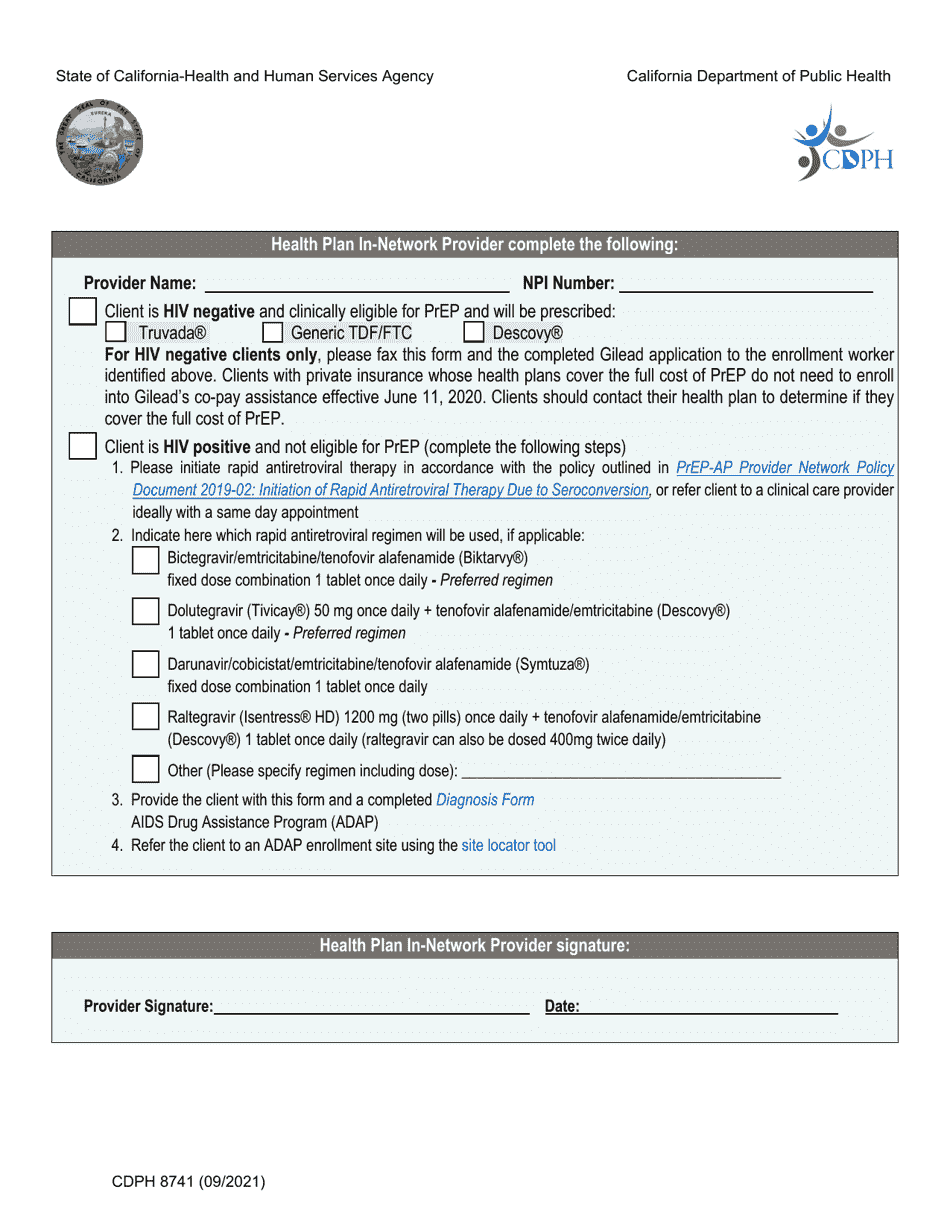
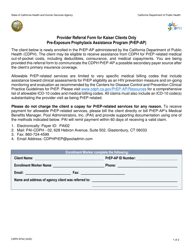
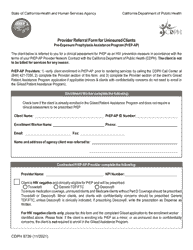
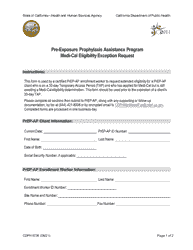
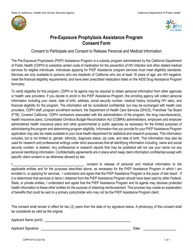
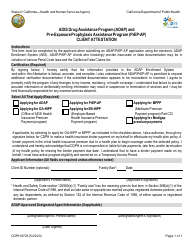
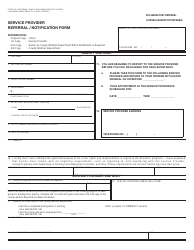
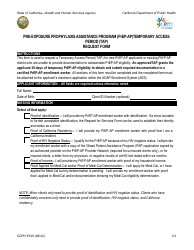
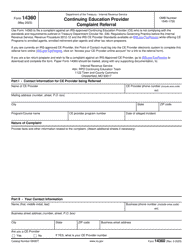
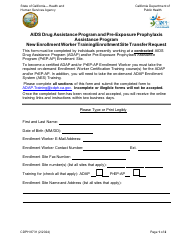
Form CDPH8741 Provider Referral Form for Insured Clients - Pre-exposure Prophylaxis Assistance Program (Prep-Ap) - California
Fill PDF Online
Fill out online for free
without registration or credit card
What Is Form CDPH8741?
This is a legal form that was released by the California Department of Public Health - a government authority operating within California. As of today, no separate filing guidelines for the form are provided by the issuing department.
Form Details:
- Released on September 1, 2021;
- The latest edition provided by the California Department of Public Health;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form CDPH8741 by clicking the link below or browse more documents and templates provided by the California Department of Public Health.