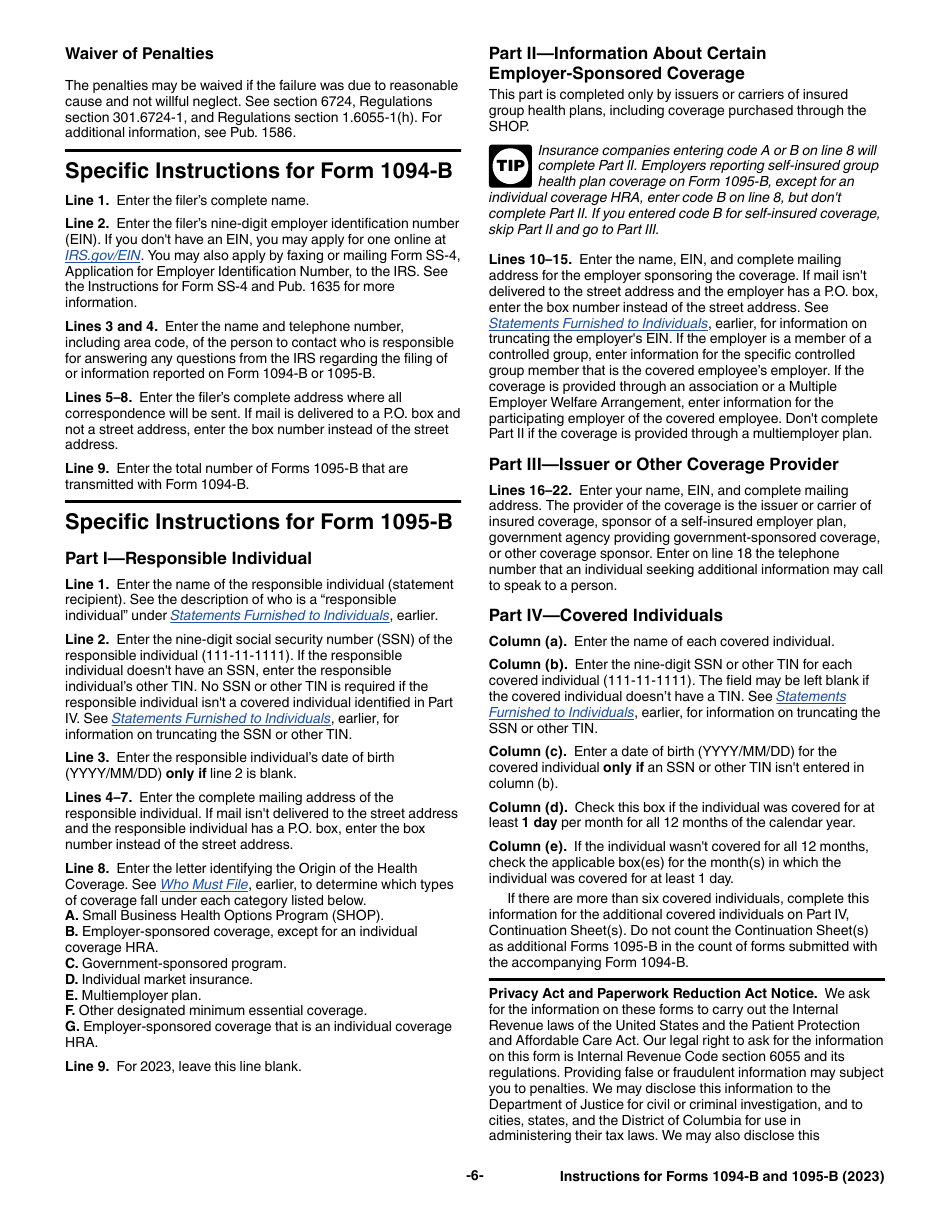
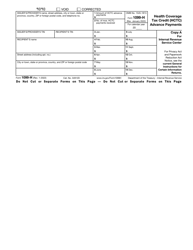
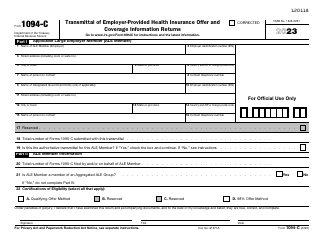
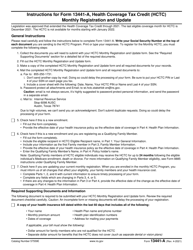
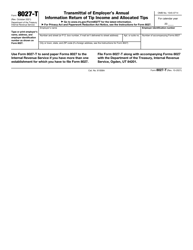
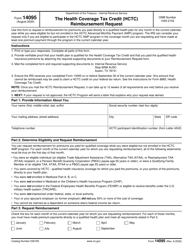
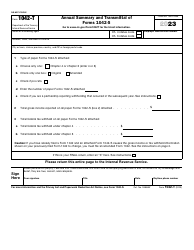
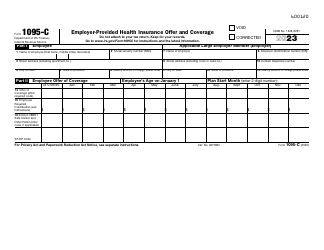
Instructions for IRS Form 1094-B, 1095-B
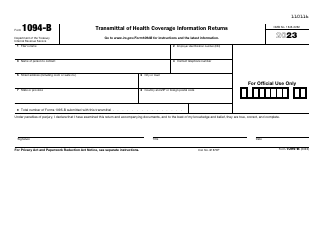
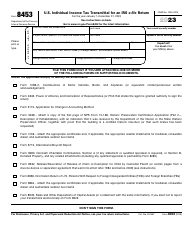
This document contains official instructions for IRS Form 1094-B , and IRS Form 1095-B . Both forms are released and collected by the Internal Revenue Service (IRS), a subdivision of the U.S. Department of the Treasury. An up-to-date fillable IRS Form 1094-B is available for download through this link. The latest available IRS Form 1095-B can be downloaded through this link.
Instruction Details:
- This 7-page document is available for download in PDF;
- Actual and applicable for filing 2023 taxes;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library of IRS-released tax documents.