This version of the form is not currently in use and is provided for reference only. Download this version of
Instructions for Form DHCS3100
for the current year.
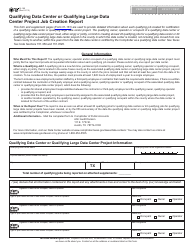
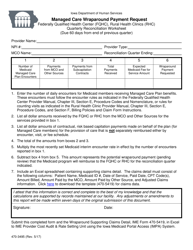
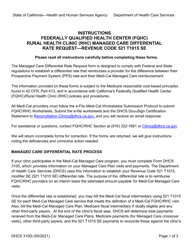
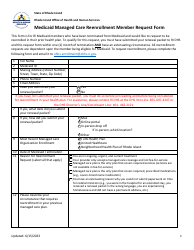
Instructions for Form DHCS3100 Federally Qualified Health Center / Rural Health Clinic Managed Care Differential Rate Request Form - California
This document contains official instructions for Form DHCS3100 , Federally Qualified Health Center/Rural Health Clinic Managed Care Differential Rate Request Form - a form released and collected by the California Department of Health Care Services.
FAQ
Q: What is Form DHCS3100?
A: Form DHCS3100 is a document used in California for Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) to request a managed care differential rate.
Q: Who uses Form DHCS3100?
A: Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) in California use Form DHCS3100.
Q: What is a managed care differential rate?
A: A managed care differential rate is a payment rate that FQHCs and RHCs receive from managed care plans for providing services to Medi-Cal beneficiaries.
Q: Why would FQHCs/RHCs need to request a managed care differential rate?
A: FQHCs/RHCs need to request a managed care differential rate if they want to receive a higher payment rate from managed care plans for their services.
Q: What information is required in Form DHCS3100?
A: Form DHCS3100 requires information such as the FQHC/RHC name, provider number, contact information, managed care plan information, and requested managed care differential rate.
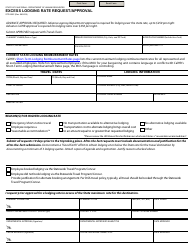
Q: Are there any supporting documents required with Form DHCS3100?
A: Yes, FQHCs/RHCs need to submit supporting documents such as cost reports, audited financial statements, and other required documentation to support their request for a managed care differential rate.
Q: Is there a deadline for submitting Form DHCS3100?
A: Yes, FQHCs/RHCs need to submit Form DHCS3100 by the specified deadline stated by DHCS.
Q: What happens after submitting Form DHCS3100?
A: After submitting Form DHCS3100, DHCS will review the request and supporting documents to determine eligibility for a managed care differential rate and notify the FQHC/RHC of their decision.
Instruction Details:
- This 2-page document is available for download in PDF;
- Actual and applicable for the current year;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library of forms released by the California Department of Health Care Services.