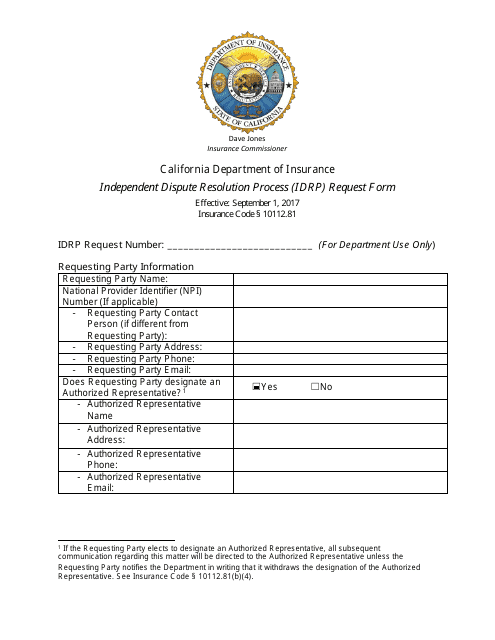
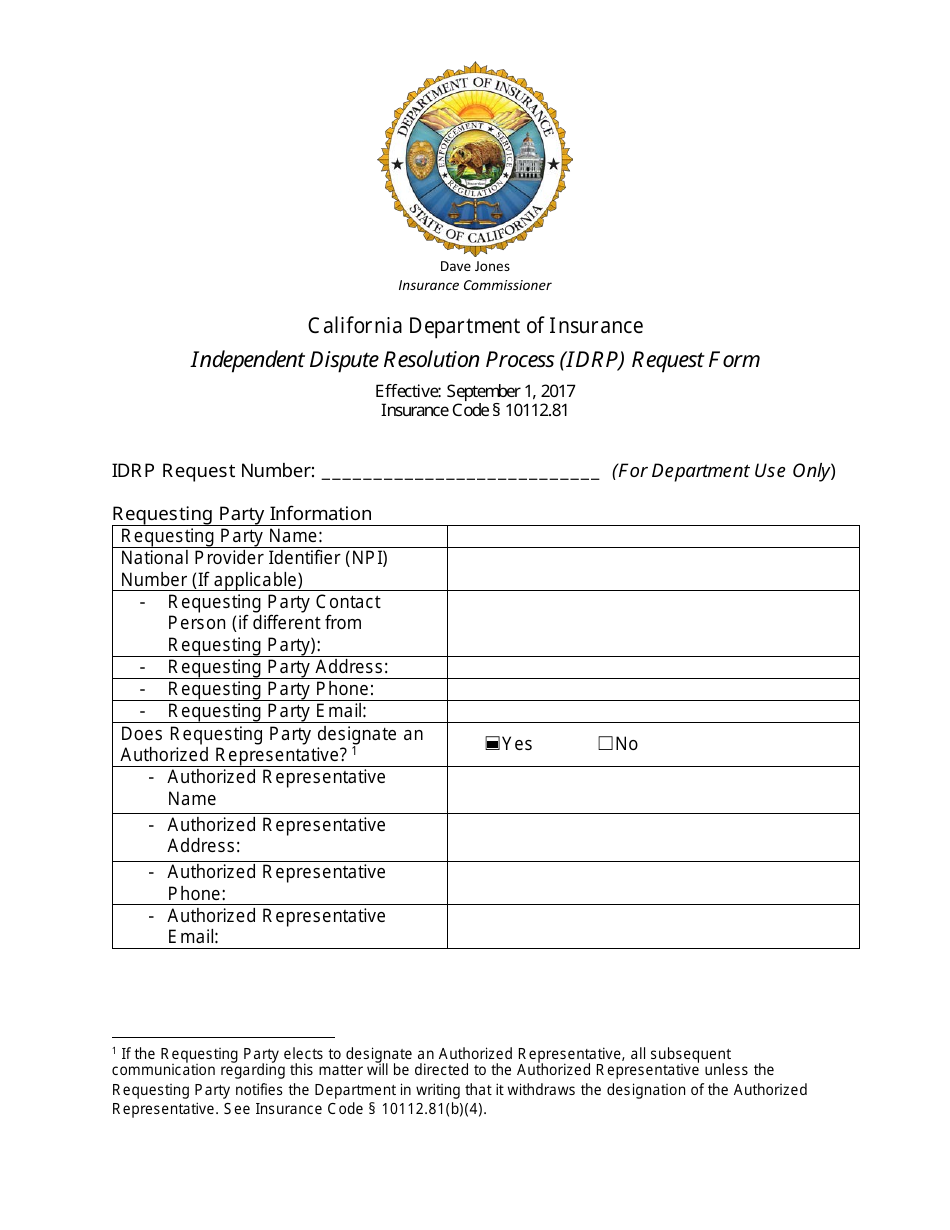
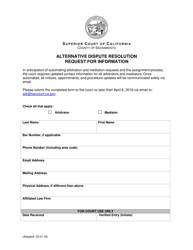
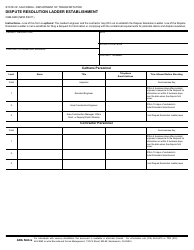
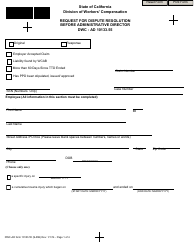
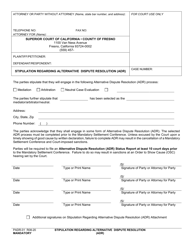
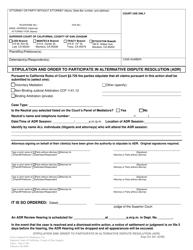
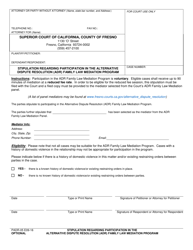
Independent Dispute Resolution Process (Idrp) Request Form - California
Independent Dispute Resolution Process (Idrp) Request Form is a legal document that was released by the California Department of Insurance - a government authority operating within California.
FAQ
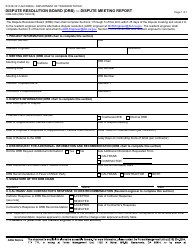
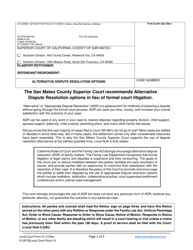
Q: What is the Independent Dispute Resolution Process (IDRP)?
A: The IDRP is a process in California that allows individuals to resolve disputes with their health insurance plans.
Q: How can I initiate the IDRP?
A: You can initiate the IDRP by filling out and submitting the IDRP Request Form.
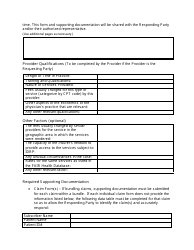
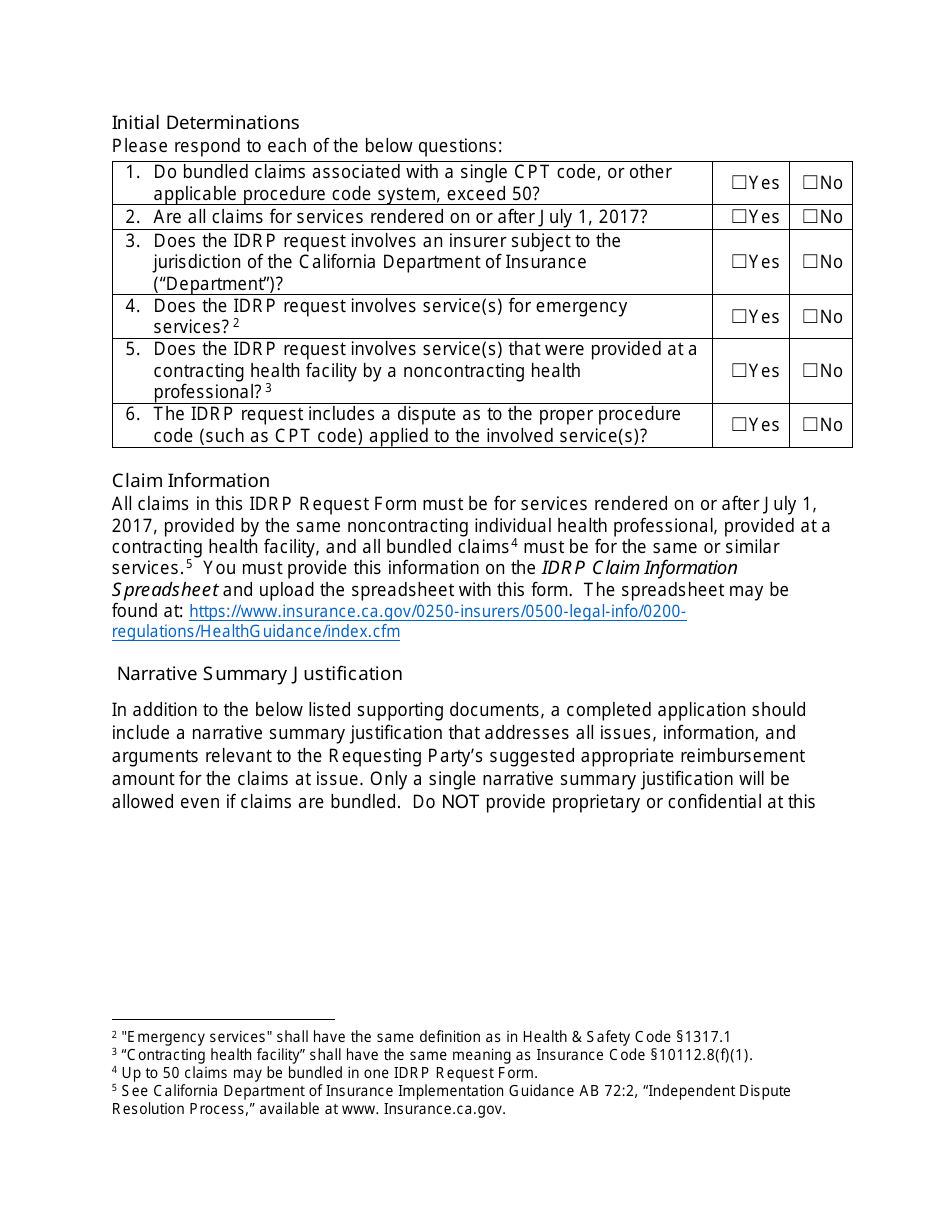
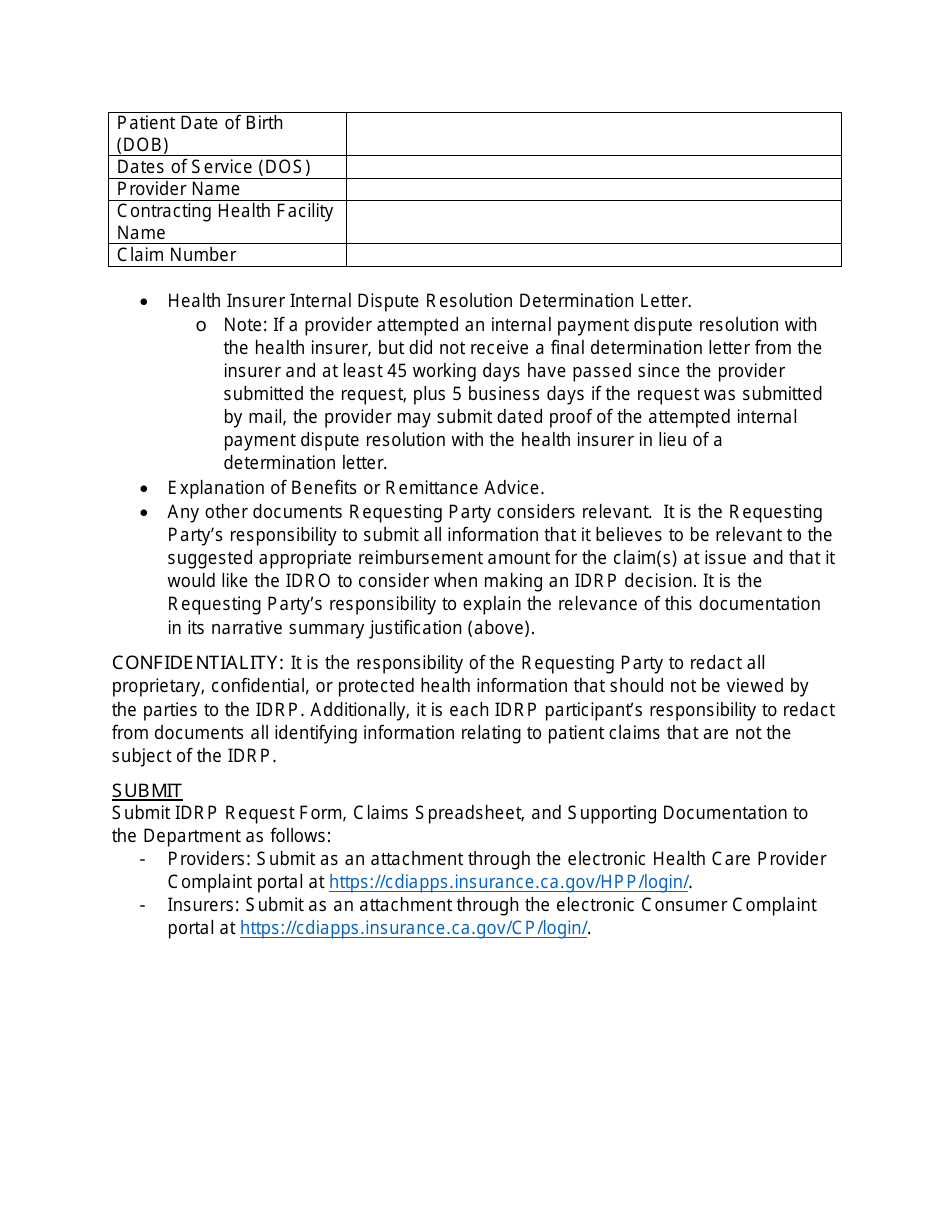
Q: What information do I need to provide on the IDRP Request Form?
A: You need to provide your personal information, health plan information, a brief explanation of the dispute, and any supporting documents.
Q: Is there a deadline for submitting the IDRP Request Form?
A: Yes, you must submit the IDRP Request Form within 6 months from the date of the final health plan decision.
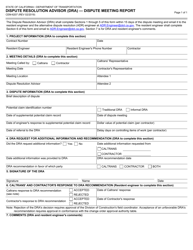
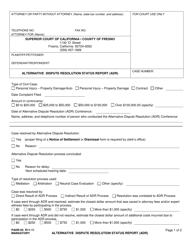
Q: What happens after I submit the IDRP Request Form?
A: After submitting the IDRP Request Form, an independent reviewer will be assigned to your case to evaluate the dispute.
Q: How long does the IDRP process take?
A: The IDRP process typically takes about 30 days, but it can vary depending on the complexity of the dispute.
Q: What are the possible outcomes of the IDRP?
A: The possible outcomes of the IDRP include upholding the health plan's decision, overturning the health plan's decision, or reaching a settlement agreement.
Q: Is the decision made through IDRP binding?
A: Yes, the decision made through IDRP is binding on both you and your health plan.
Q: Can I appeal the decision made through IDRP?
A: Yes, you have the right to appeal the decision made through IDRP to the appropriate court.
Q: Is there a fee for using the IDRP?
A: No, there is no fee for using the IDRP.
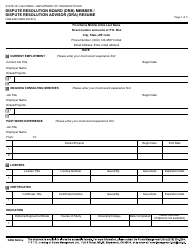
Form Details:
- Released on September 1, 2017;
- The latest edition currently provided by the California Department of Insurance;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the California Department of Insurance.