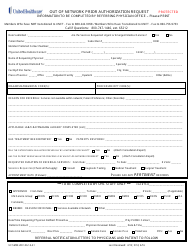
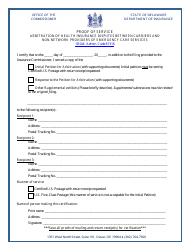
Justification for Use of out-Of-Network Provider - Delaware
Justification for Use of out-Of-Network Provider is a legal document that was released by the Delaware Department of Services for Children, Youth and their Families - a government authority operating within Delaware.
FAQ
Q: Can I use an out-of-network provider in Delaware?
A: Yes, you can use an out-of-network provider in Delaware.
Q: What is the justification for using an out-of-network provider in Delaware?
A: The justification for using an out-of-network provider in Delaware may vary depending on individual circumstances. Some reasons could include specialized medical treatment or services not available within the network, preference for a specific provider, or emergencies when immediate care is needed and an in-network provider is not readily accessible.
Q: Do I need prior authorization to use an out-of-network provider in Delaware?
A: Prior authorization requirements for using an out-of-network provider may vary depending on your insurance plan. It is essential to check with your insurance provider or review your plan documents to understand the specific requirements.
Q: Will my insurance cover the costs of using an out-of-network provider in Delaware?
A: Coverage for out-of-network providers varies among insurance plans. It is crucial to review your plan documents or contact your insurance provider to understand the extent of coverage for out-of-network services in Delaware.
Q: Are there any additional costs associated with using an out-of-network provider in Delaware?
A: Yes, using an out-of-network provider may result in additional costs, such as higher deductibles, co-pays, or coinsurance. It is important to understand your insurance plan's out-of-network coverage and associated costs.
Q: What steps should I take if I want to use an out-of-network provider in Delaware?
A: If you want to use an out-of-network provider in Delaware, it is advisable to contact your insurance provider first to understand the coverage and any required pre-authorization processes. Additionally, consider discussing your options with your primary care physician for guidance and recommendations.
Form Details:
- Released on September 1, 2011;
- The latest edition currently provided by the Delaware Department of Services for Children, Youth and their Families;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Delaware Department of Services for Children, Youth and their Families.