Instructions for Form DHCS6065A Good Cause Certification - California
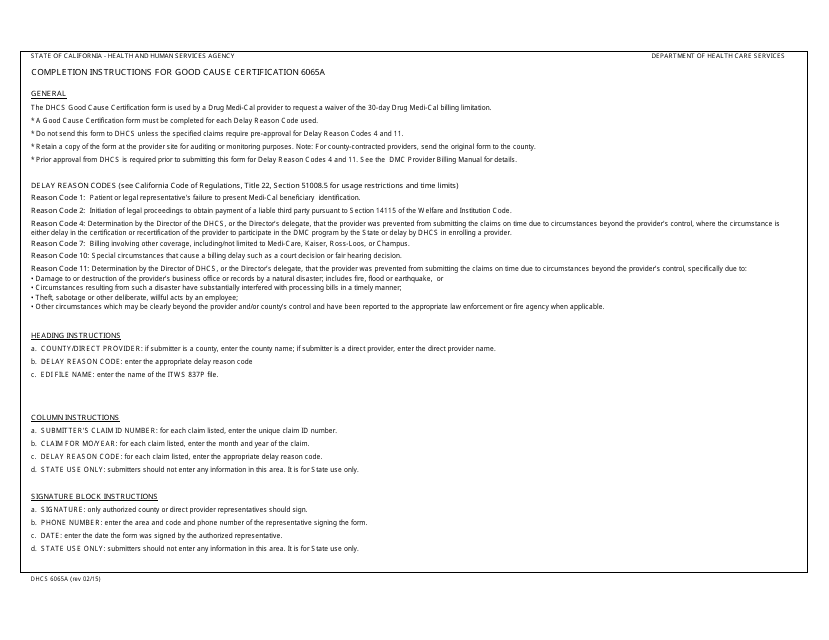
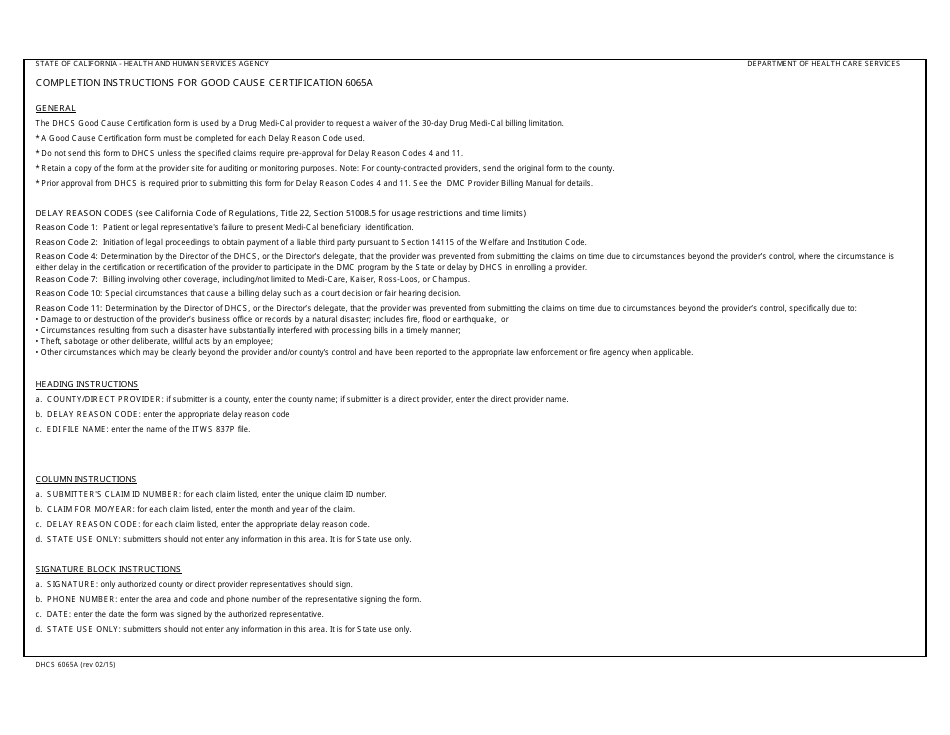
This document contains official instructions for Form DHCS6065A , Good Cause Certification - a form released and collected by the California Department of Health Care Services. An up-to-date fillable Form DHCS6065A is available for download through this link.
FAQ
Q: What is Form DHCS6065A?
A: Form DHCS6065A is a Good Cause Certification form in California.
Q: What is the purpose of Form DHCS6065A?
A: The purpose of Form DHCS6065A is to certify that an individual meets the criteria for good cause for not cooperating with child support services.
Q: Who needs to fill out Form DHCS6065A?
A: The individual who is requesting an exemption from cooperating with child support services needs to fill out Form DHCS6065A.
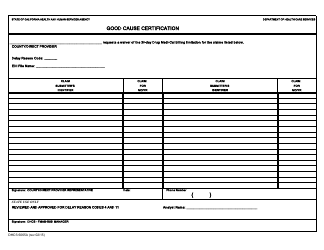
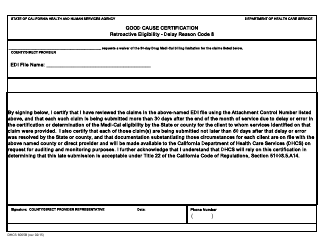
Q: What information is required on Form DHCS6065A?
A: Form DHCS6065A requires the individual's personal information, the reason for not cooperating with child support services, and any supporting documentation.
Q: Are there any fees associated with Form DHCS6065A?
A: No, there are no fees associated with Form DHCS6065A.
Q: What happens after I submit Form DHCS6065A?
A: After submitting Form DHCS6065A, it will be reviewed by the California Department of Health Care Services, and a decision will be made regarding the individual's exemption from cooperating with child support services.
Instruction Details:
- This 1-page document is available for download in PDF;
- Actual and applicable for the current year;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library of forms released by the California Department of Health Care Services.