This version of the form is not currently in use and is provided for reference only. Download this version of
Instructions for IRS Form 8885
for the current year.
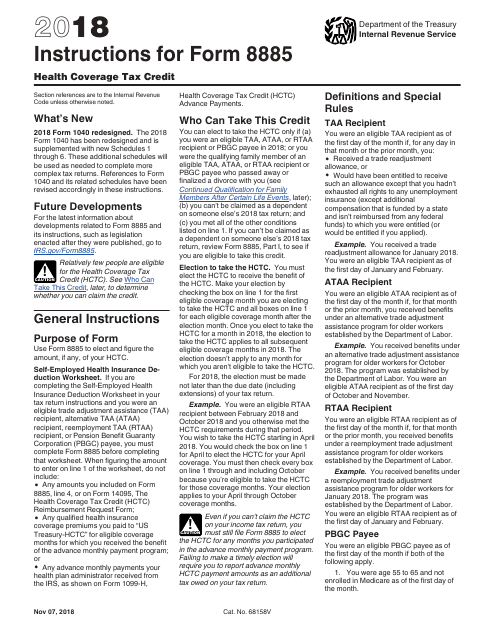
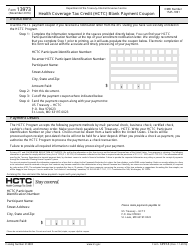
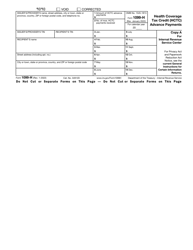
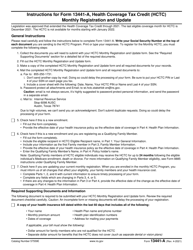
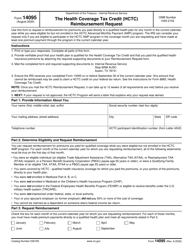
Instructions for IRS Form 8885 Health Coverage Tax Credit
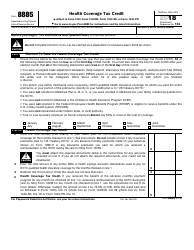
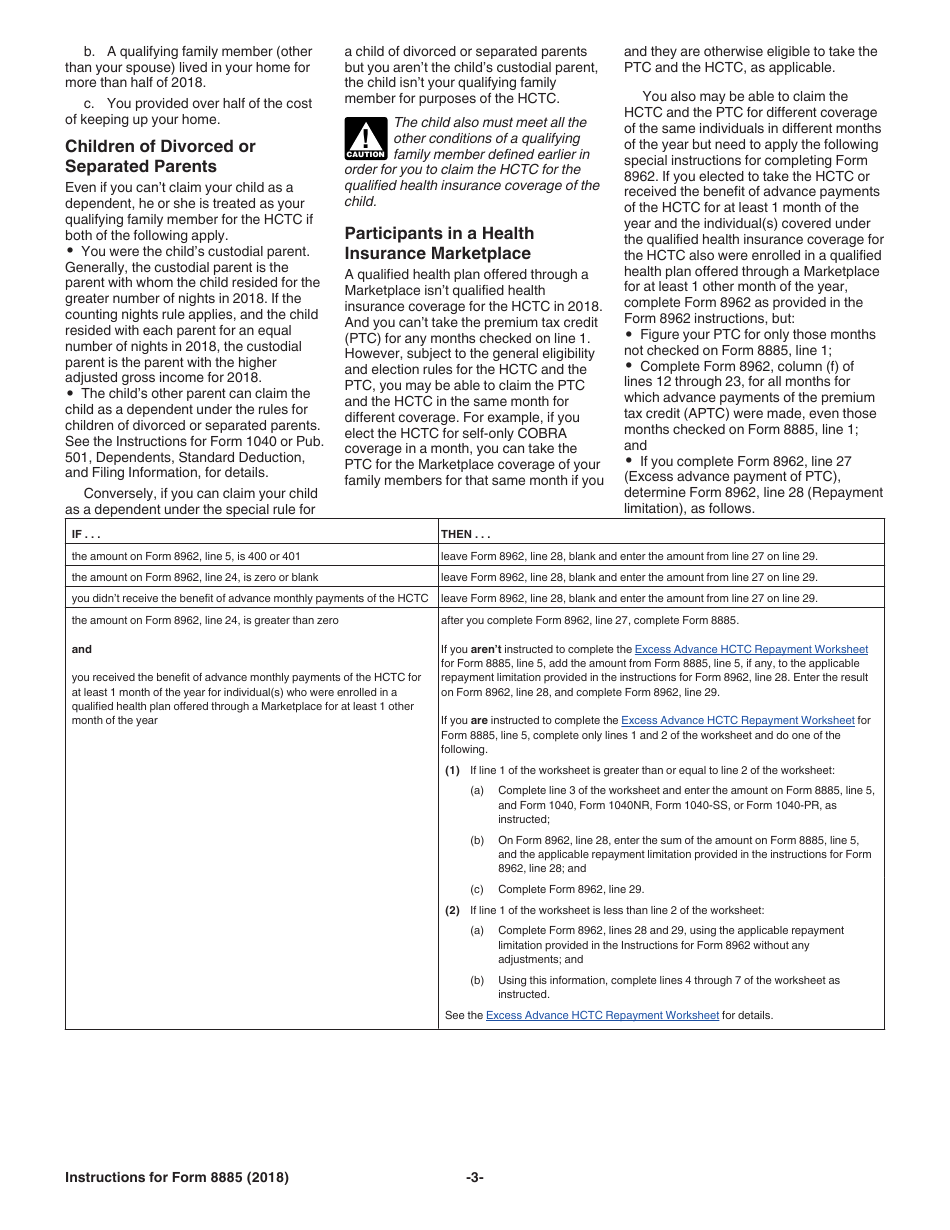
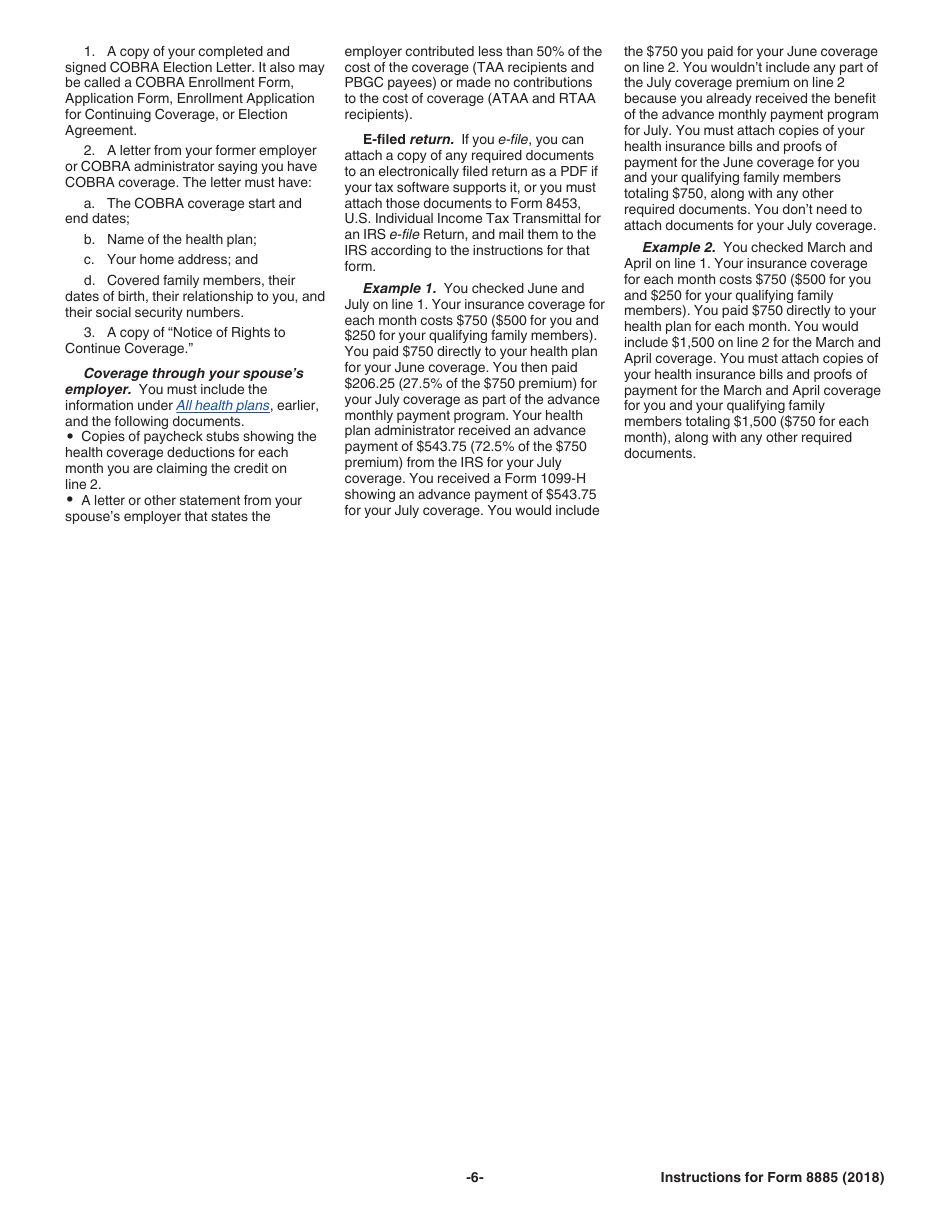
This document contains official instructions for IRS Form 8885 , Health Coverage Tax Credit - a tax form released and collected by the Internal Revenue Service (IRS), a subdivision of the U.S. Department of the Treasury. An up-to-date fillable IRS Form 8885 is available for download through this link.
FAQ
Q: What is IRS Form 8885?
A: IRS Form 8885 is a tax form used to claim the Health Coverage Tax Credit.
Q: Who can claim the Health Coverage Tax Credit?
A: Individuals who are eligible for the Health Coverage Tax Credit can claim it.
Q: What is the purpose of the Health Coverage Tax Credit?
A: The Health Coverage Tax Credit helps eligible individuals pay for qualified health insurance.
Q: How do I qualify for the Health Coverage Tax Credit?
A: You may qualify for the Health Coverage Tax Credit if you are receiving Trade Adjustment Assistance, Alternative Trade Adjustment Assistance, or pension benefit payments from the Pension Benefit Guaranty Corporation (PBGC).
Q: What expenses does the Health Coverage Tax Credit cover?
A: The Health Coverage Tax Credit can help cover a portion of your monthly premium for qualified health insurance.
Q: How do I claim the Health Coverage Tax Credit?
A: To claim the Health Coverage Tax Credit, you need to complete IRS Form 8885 and include it with your tax return.
Q: Is the Health Coverage Tax Credit a refundable credit?
A: No, the Health Coverage Tax Credit is a non-refundable credit, meaning it can reduce your tax liability but will not result in a refund if the credit exceeds your tax owed.
Instruction Details:
- This 6-page document is available for download in PDF;
- Not applicable for the current tax year. Choose a more recent version to file this year's taxes;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library of IRS-released tax documents.