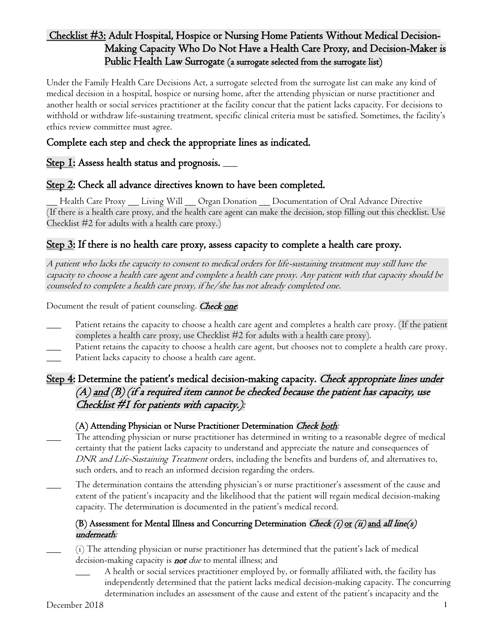
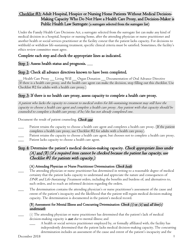
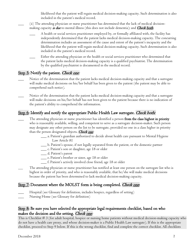
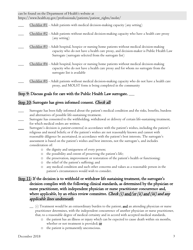
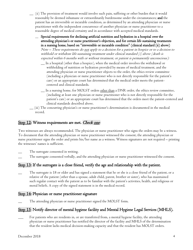
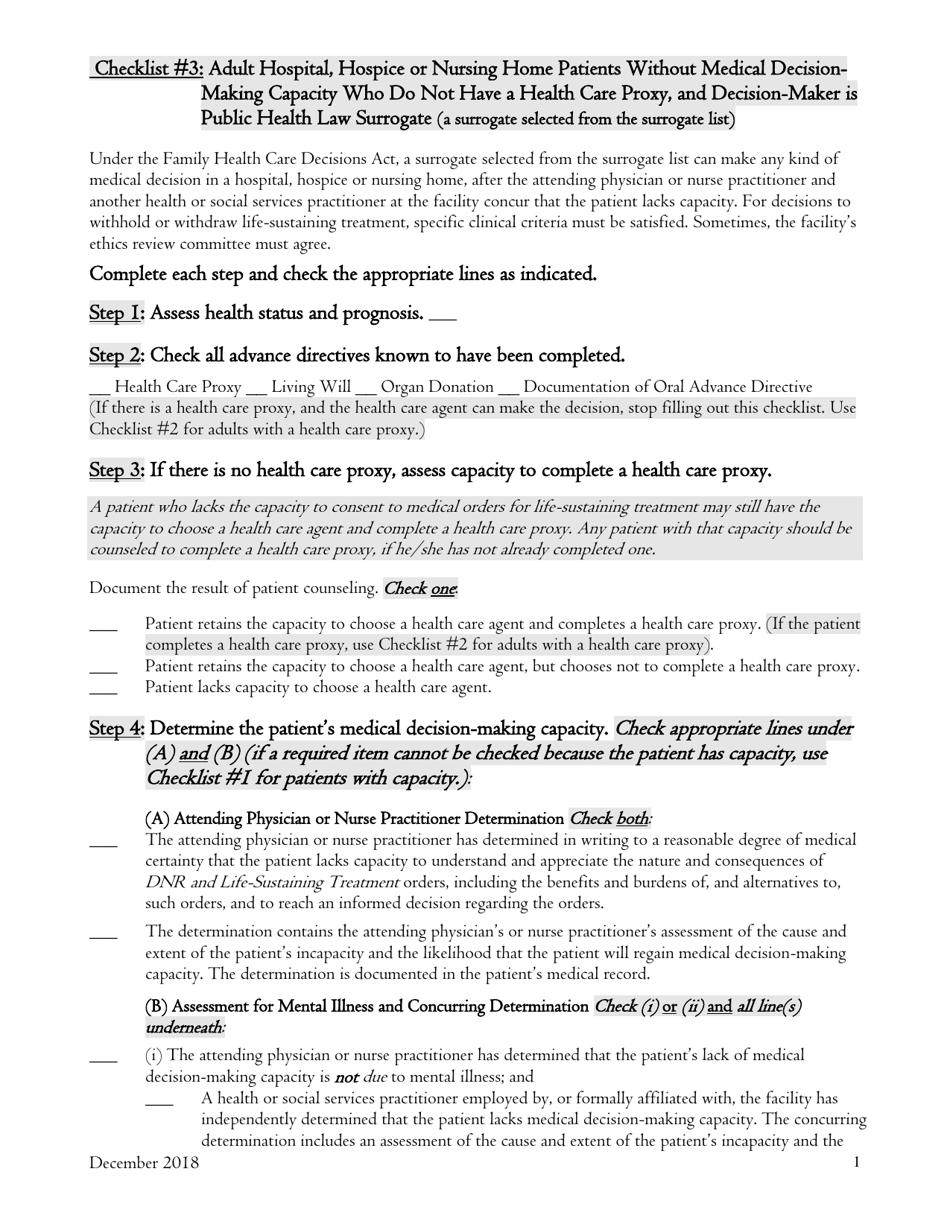
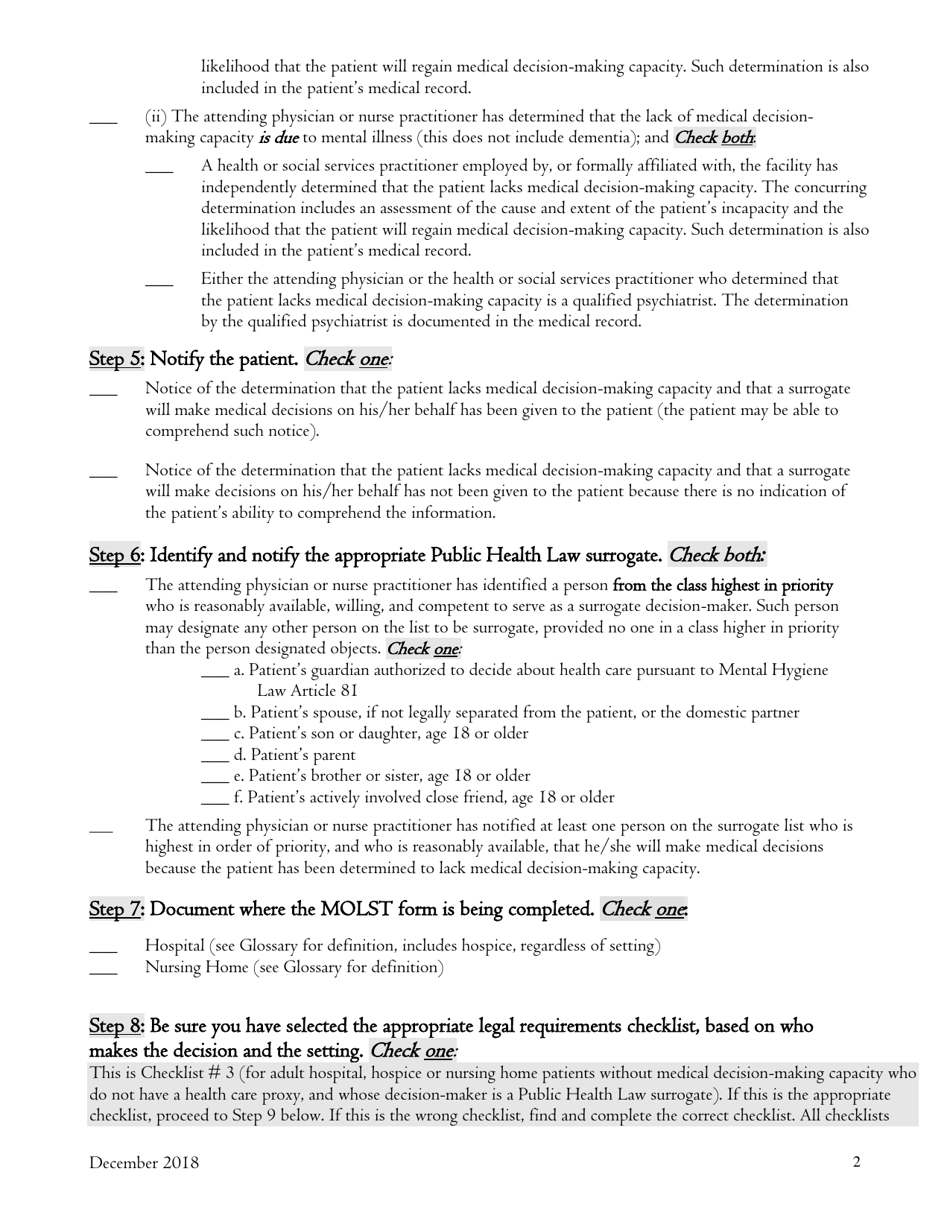
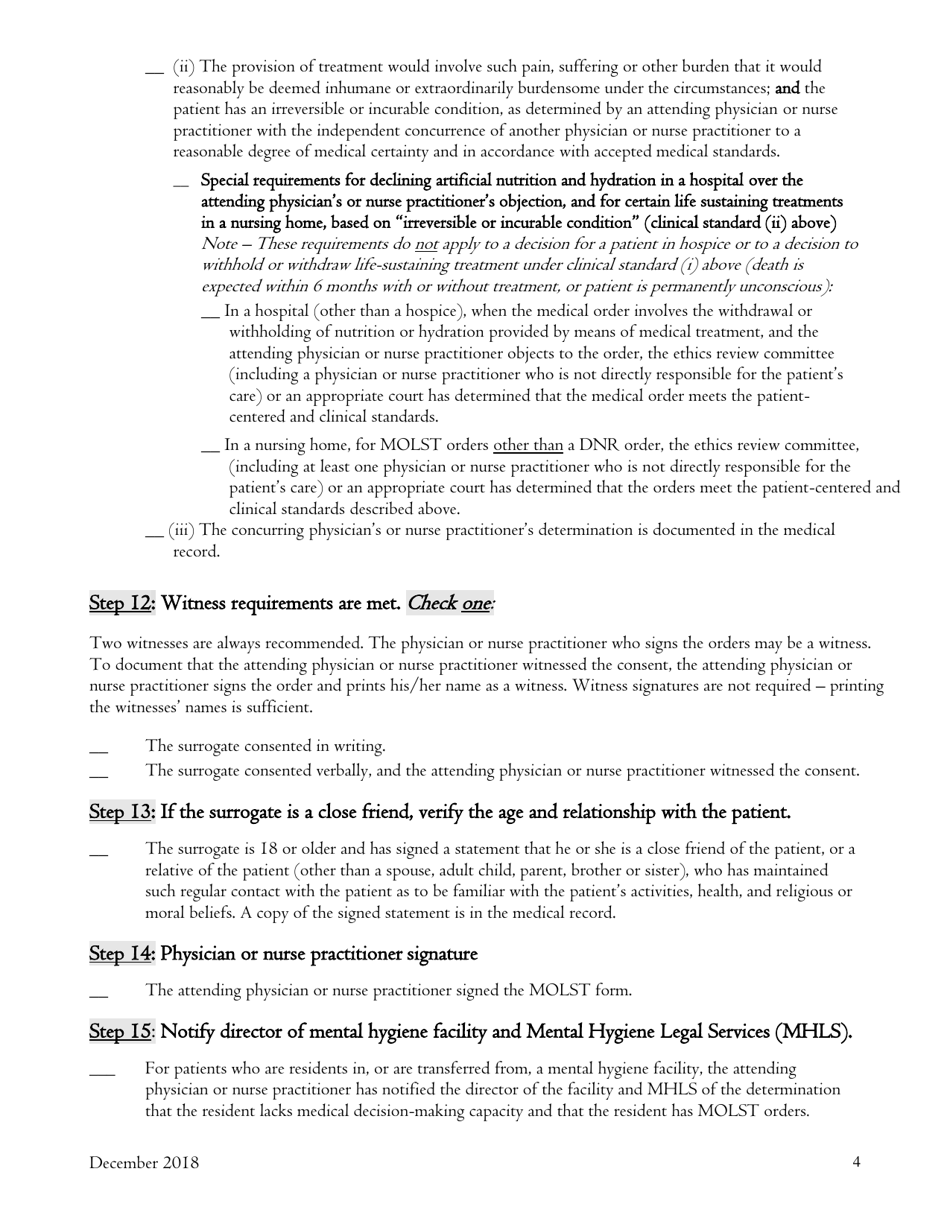
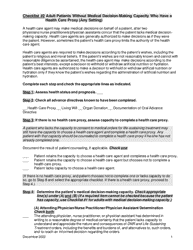
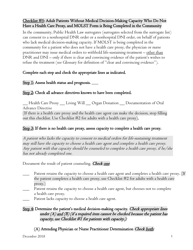
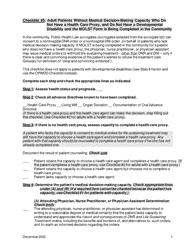
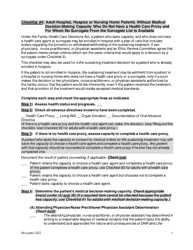
Checklist #3: Adult Hospital, Hospice or Nursing Home Patients Without Medical Decisionmaking Capacity Who Do Not Have a Health Care Proxy, and Decision-Maker Is Public Health Law Surrogate (A Surrogate Selected From the Surrogate List) - New York
Checklist #3: Adult Hospital, Hospice or Health Law Surrogate (A Surrogate Selected From the Surrogate List) is a legal document that was released by the New York State Department of Health - a government authority operating within New York.
FAQ
Q: Who does this checklist apply to?
A: This checklist applies to adult hospital, hospice, or nursing home patients in New York who do not have the capacity to make medical decisions and do not have a health care proxy.
Q: What is a health care proxy?
A: A health care proxy is a person appointed by an individual to make medical decisions on their behalf if they become unable to do so.
Q: What is a surrogate?
A: A surrogate is someone who is legally authorized to make medical decisions for a patient who lacks decision-making capacity and does not have a health care proxy.
Q: Who can be a surrogate for a patient without a health care proxy?
A: In New York, a surrogate can be selected from the surrogate list provided by public health law.
Q: Can a public health law surrogate make medical decisions for a patient without a health care proxy?
A: Yes, a public health law surrogate can make medical decisions for a patient without a health care proxy in New York.
Q: What is the purpose of this checklist?
A: The purpose of this checklist is to guide caregivers and healthcare providers in managing medical decisions for patients without medical decision-making capacity and without a health care proxy in New York.
Form Details:
- Released on December 1, 2018;
- The latest edition currently provided by the New York State Department of Health;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the New York State Department of Health.