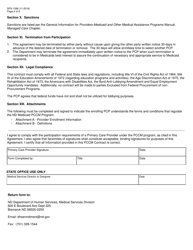
This version of the form is not currently in use and is provided for reference only. Download this version of
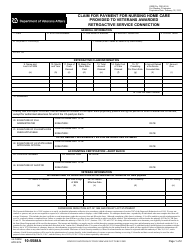
Form SFN1296
for the current year.
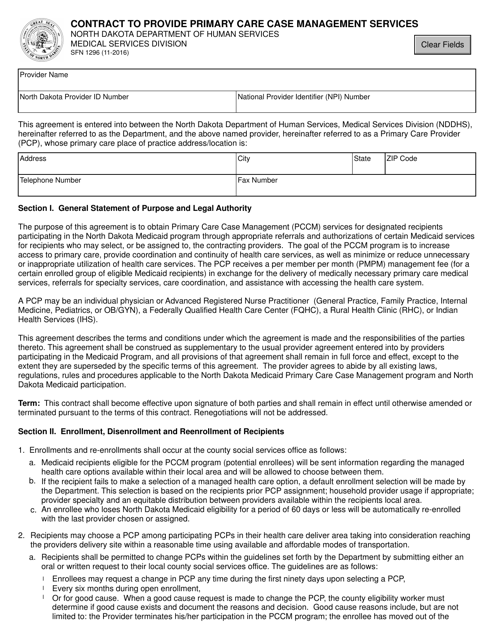
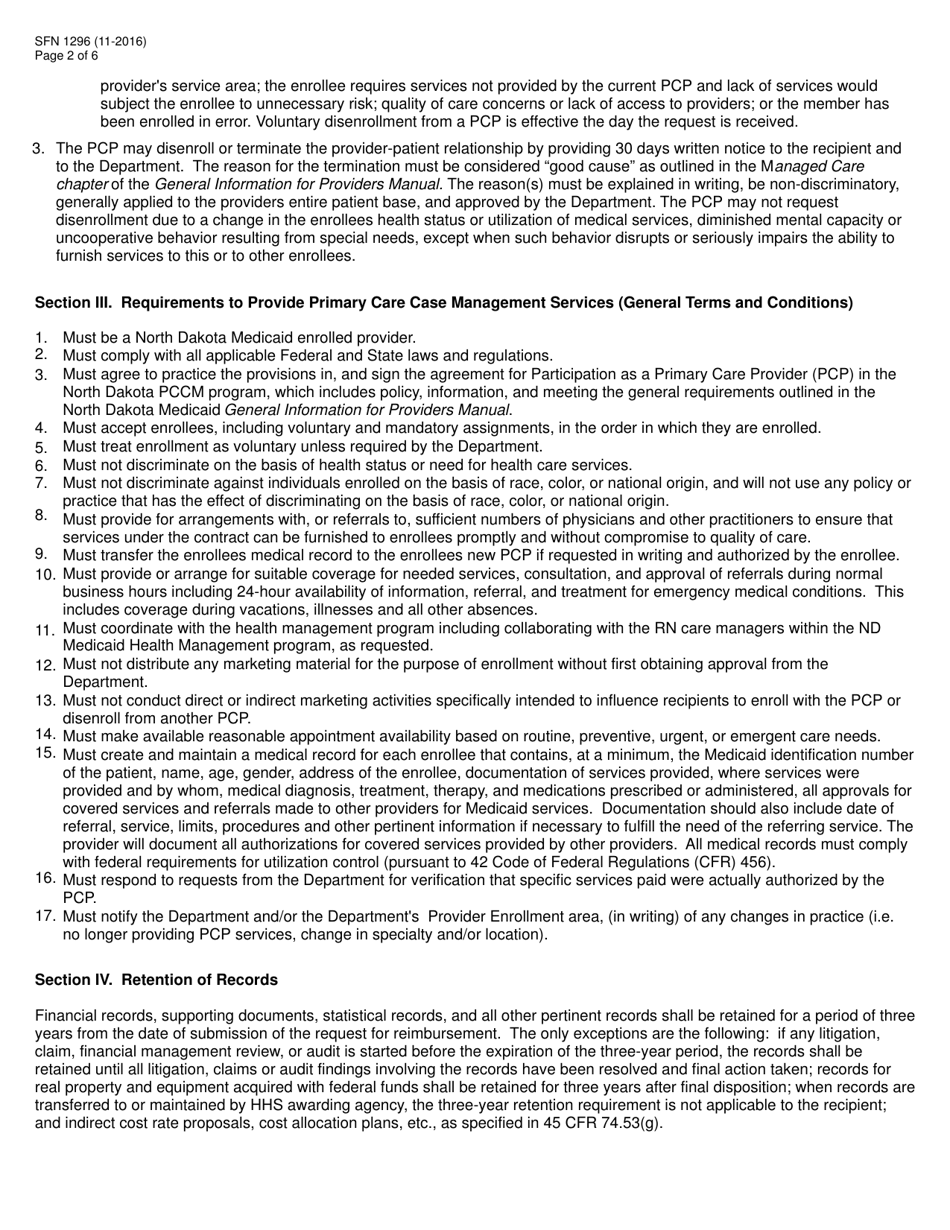
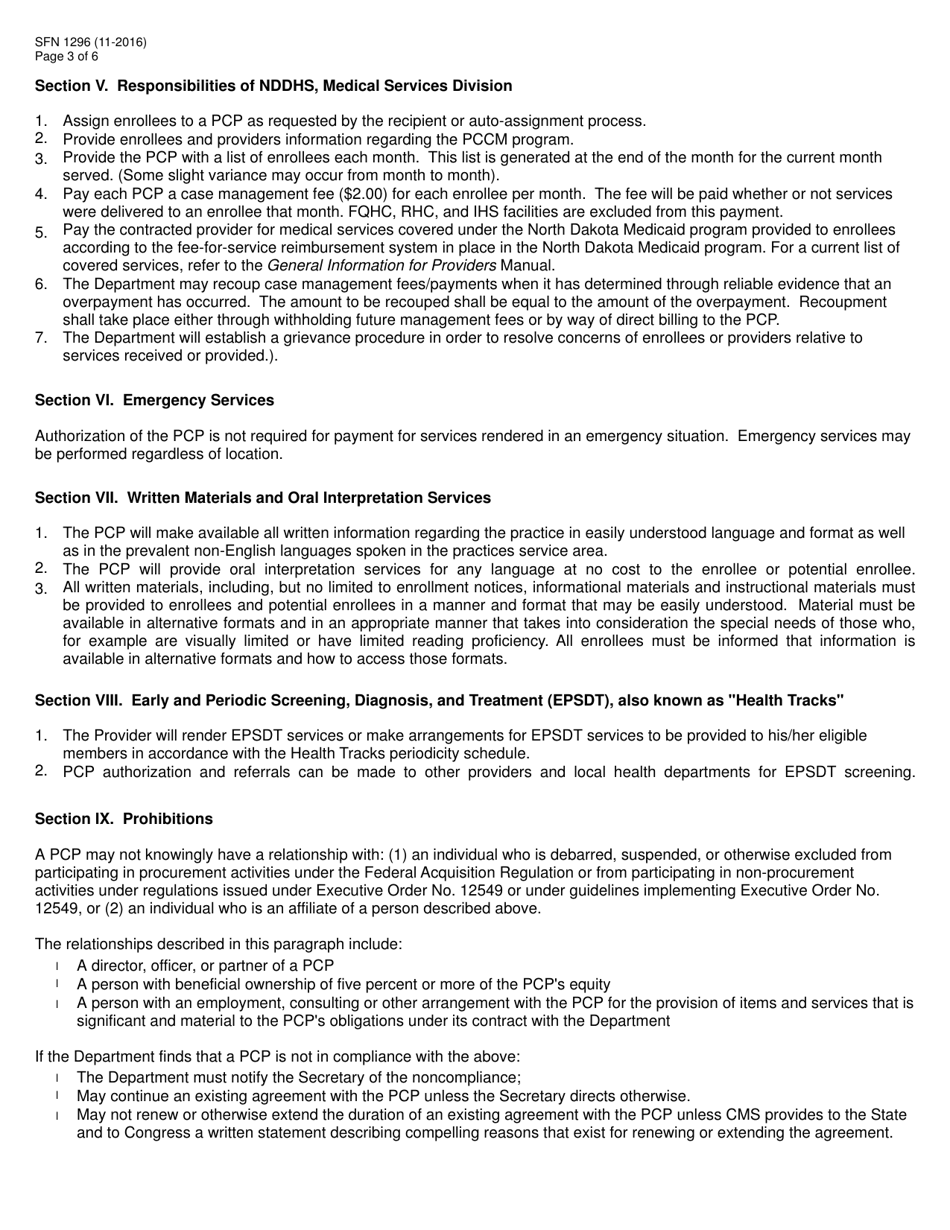
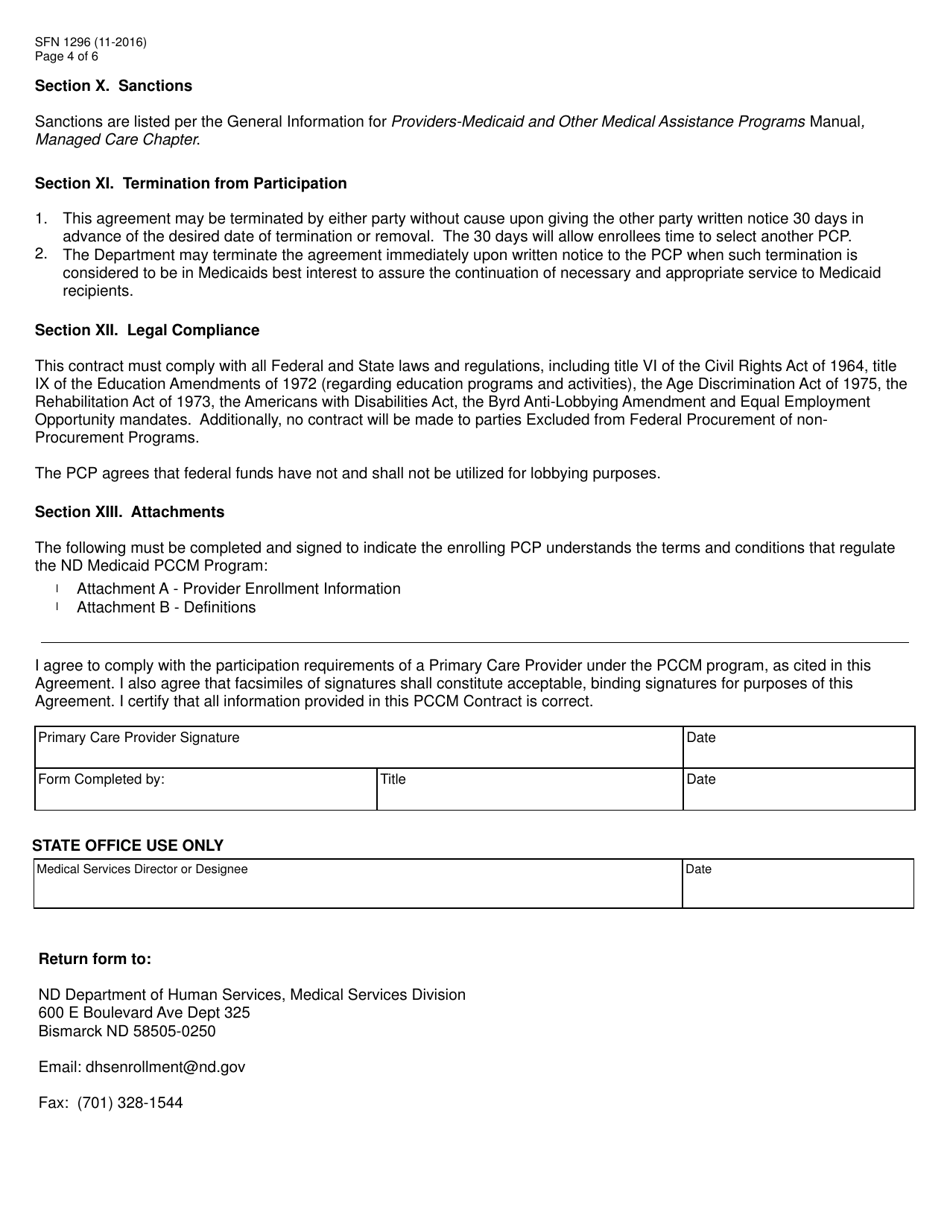
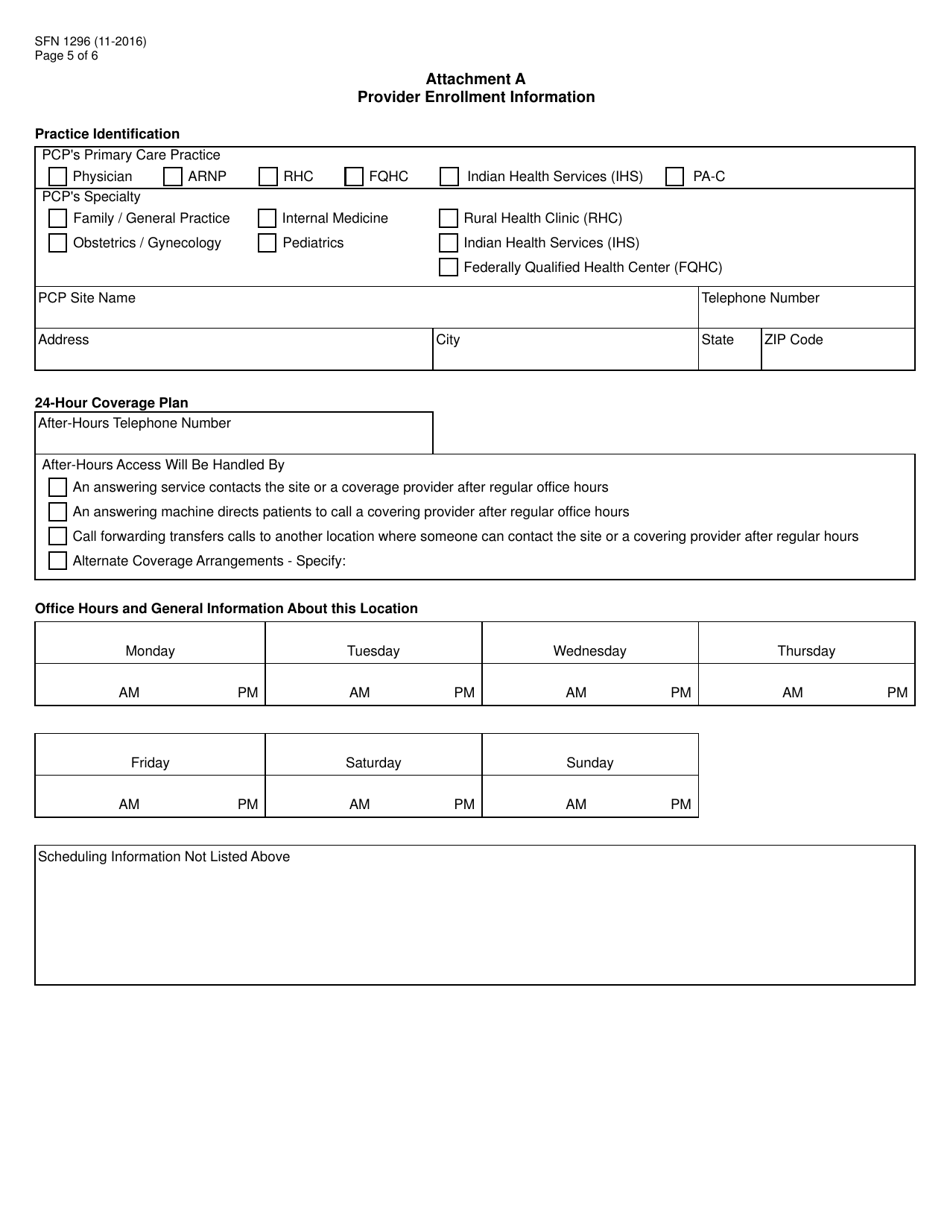
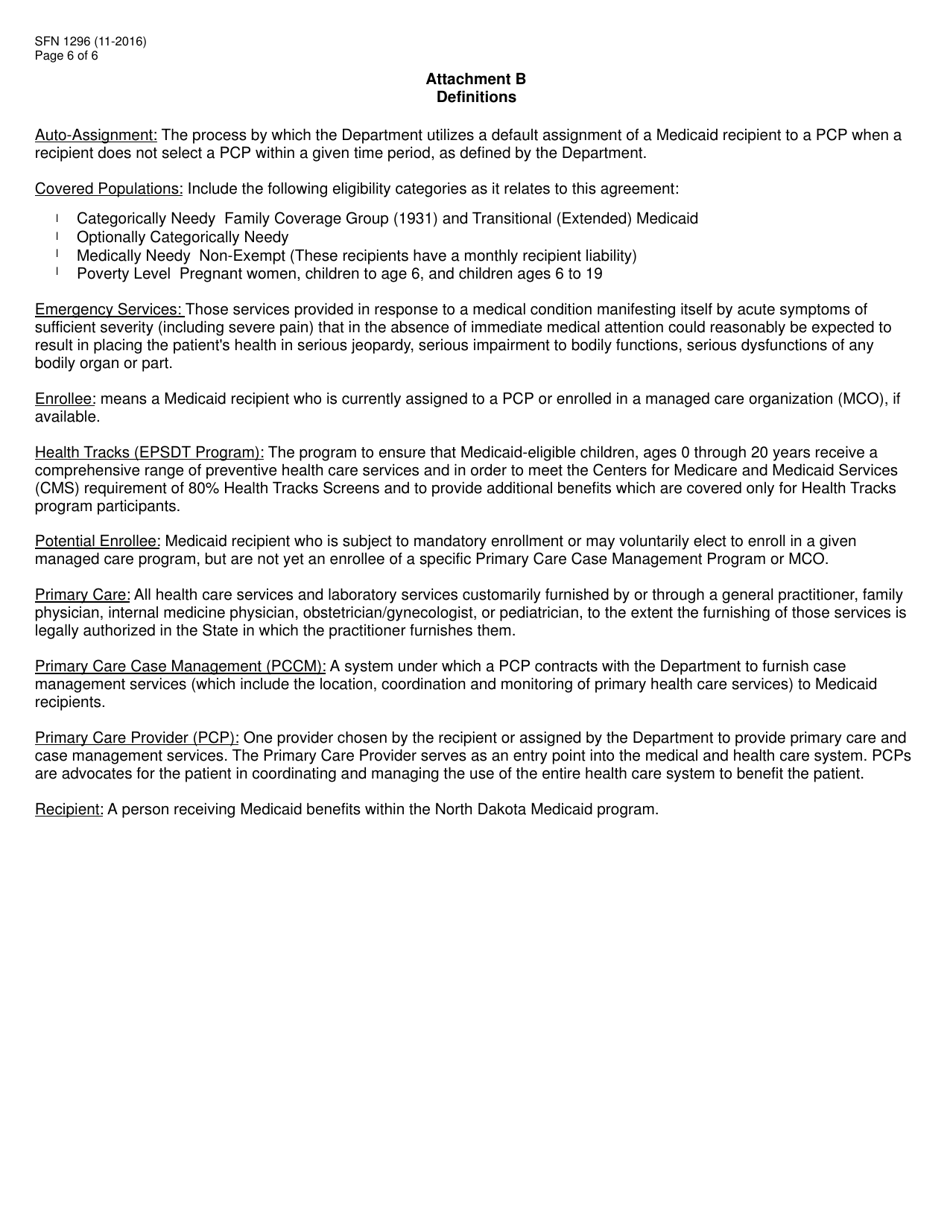
Form SFN1296 Contract to Provide Primary Care Case Management Services - North Dakota
What Is Form SFN1296?
This is a legal form that was released by the North Dakota Department of Labor and Human Rights - a government authority operating within North Dakota. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
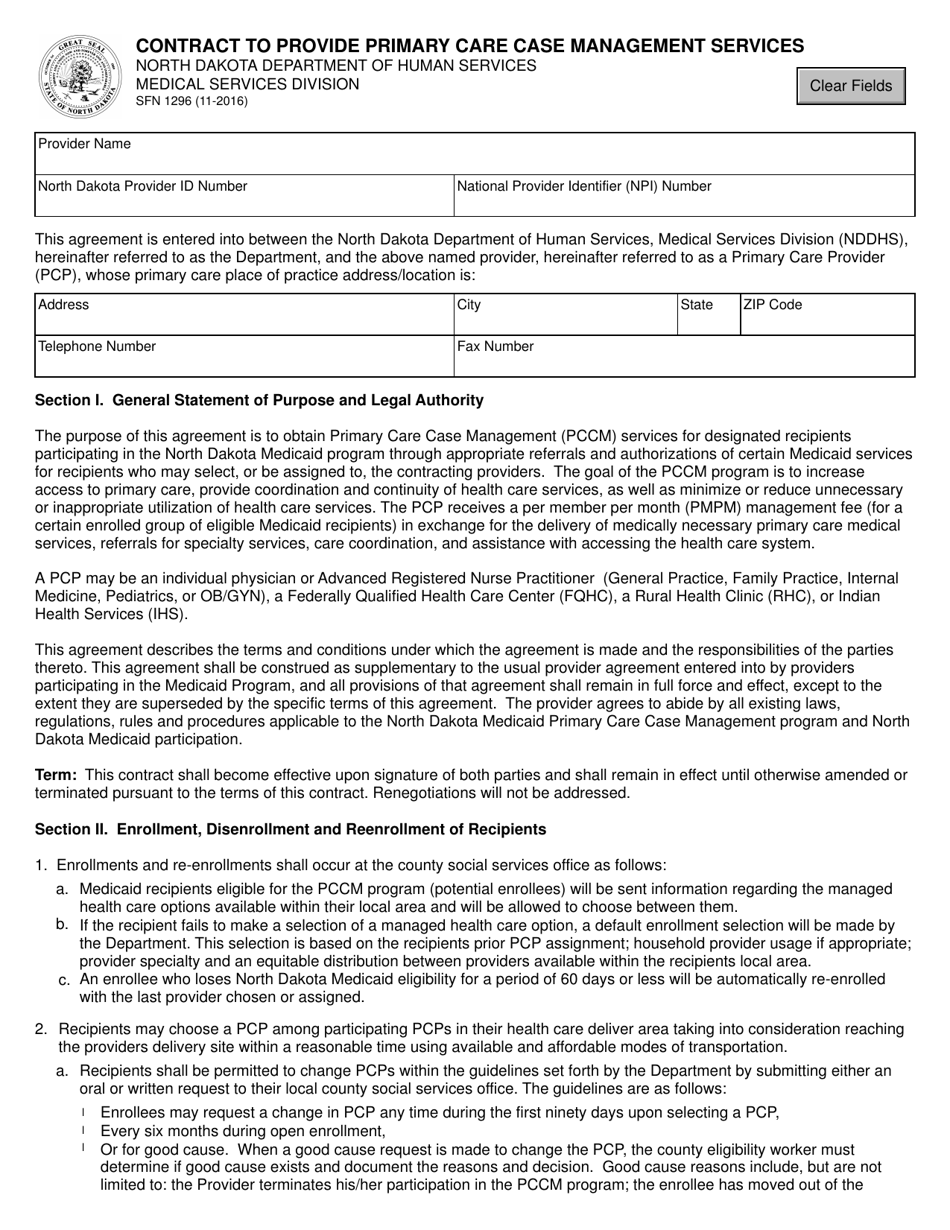
Q: What is the SFN1296 Contract?
A: The SFN1296 Contract is a document used in North Dakota to provide Primary Care Case Management Services.
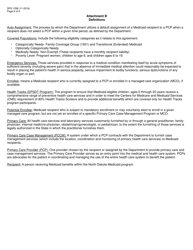
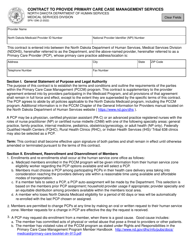
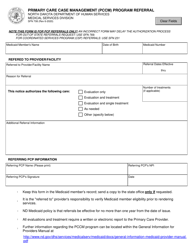
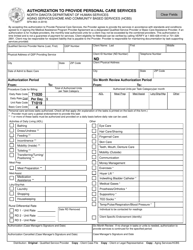
Q: What are Primary Care Case Management Services?
A: Primary Care Case Management Services are services that help individuals coordinate and manage their healthcare.
Q: Who can provide Primary Care Case Management Services?
A: Qualified healthcare providers or organizations can provide Primary Care Case Management Services.
Q: How do I obtain a SFN1296 Contract?
A: To obtain a SFN1296 Contract, you can contact the appropriate North Dakota government agency.
Q: What are the responsibilities of a Primary Care Case Management Service provider?
A: The responsibilities of a Primary Care Case Management Service provider include coordinating healthcare services, developing care plans, and advocating for the individual's health needs.
Q: Are there any eligibility requirements to provide Primary Care Case Management Services?
A: Yes, there may be eligibility requirements such as specific qualifications or certifications.
Q: Can I bill for Primary Care Case Management Services?
A: Yes, Primary Care Case Management Services are billable.
Form Details:
- Released on November 1, 2016;
- The latest edition provided by the North Dakota Department of Labor and Human Rights;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form SFN1296 by clicking the link below or browse more documents and templates provided by the North Dakota Department of Labor and Human Rights.