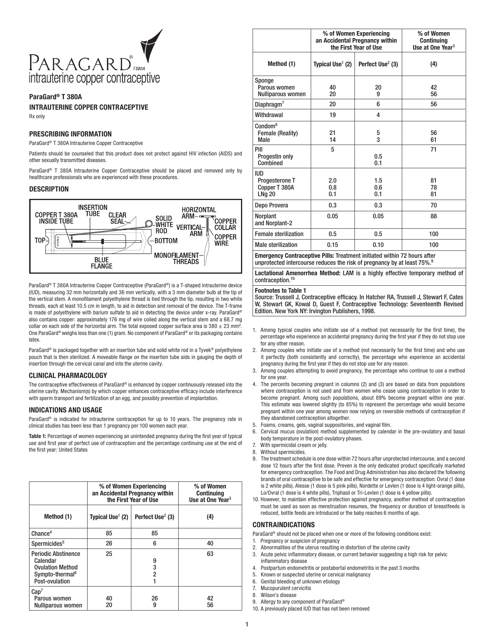
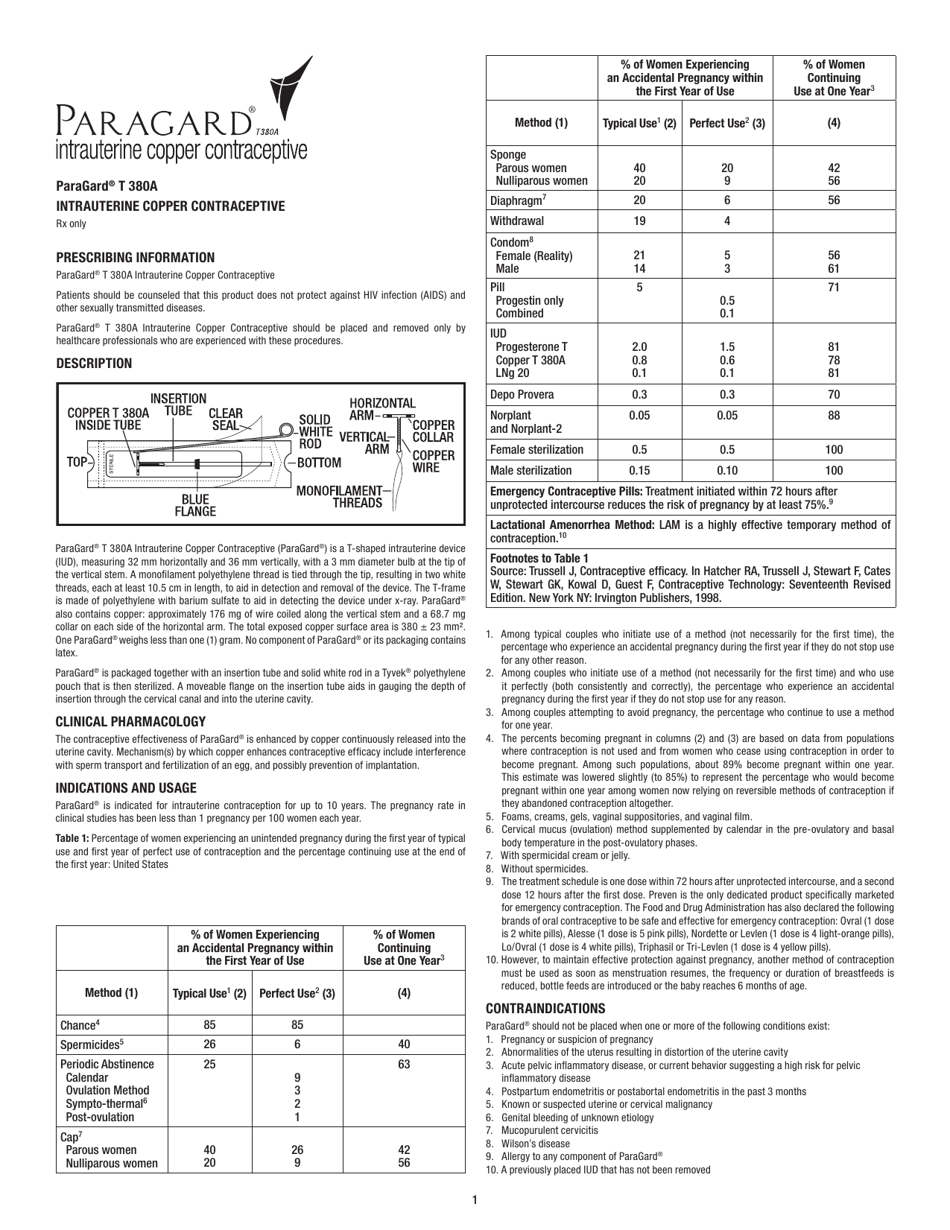
Paragard T380a Intrauterine Copper Contraceptive Information
Paragard T380a Intrauterine Copper Contraceptive Information is a 5-page legal document that was released by the U.S. Department of Health and Human Services - U.S. Food and Drug Administration and used nation-wide.
FAQ
Q: What is Paragard T380a?
A: Paragard T380a is an intrauterine copper contraceptive.
Q: How does Paragard T380a work?
A: Paragard T380a works by releasing copper ions that prevent pregnancy.
Q: How long does Paragard T380a last?
A: Paragard T380a can last for up to 10 years.
Q: Is Paragard T380a effective?
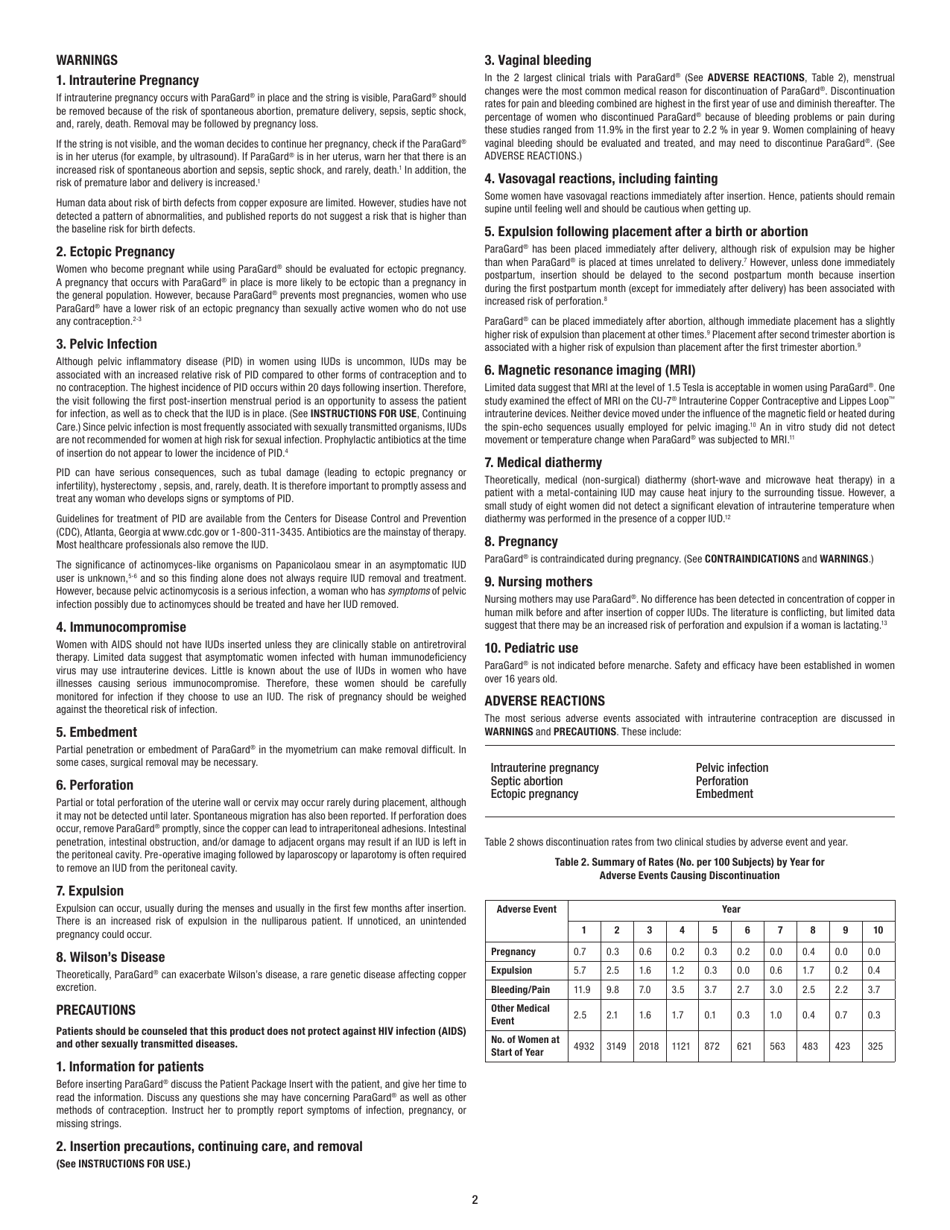
A: Yes, Paragard T380a is highly effective at preventing pregnancy.
Q: Is Paragard T380a reversible?
A: Yes, Paragard T380a is reversible and can be removed by a healthcare professional.
Q: What are the side effects of Paragard T380a?
A: Common side effects of Paragard T380a include heavier and longer periods.
Q: Is Paragard T380a covered by insurance?
A: Coverage for Paragard T380a may vary depending on your insurance plan.
Q: Is Paragard T380a available over-the-counter?
A: No, Paragard T380a requires a prescription from a healthcare provider.
Form Details:
- The latest edition currently provided by the U.S. Department of Health and Human Services - U.S. Food and Drug Administration;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more legal forms and templates provided by the issuing department.