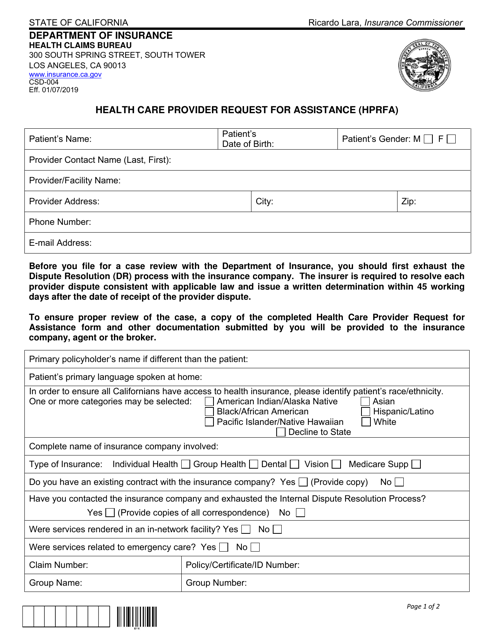
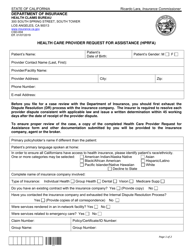
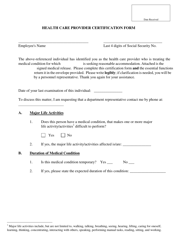
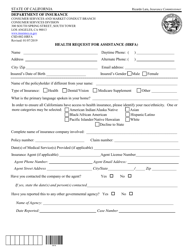
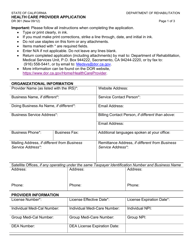
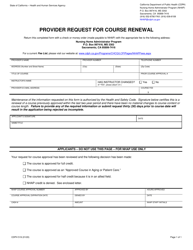
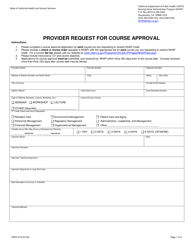
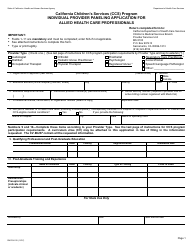
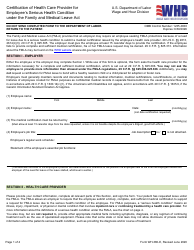
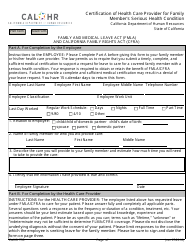
Form CSD-004 Health Care Provider Request for Assistance (Hprfa) - California
What Is Form CSD-004?
This is a legal form that was released by the California Department of Insurance - a government authority operating within California. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form CSD-004?
A: Form CSD-004 is the Health Care ProviderRequest for Assistance (HPRFA) form in California.
Q: What is the purpose of Form CSD-004?
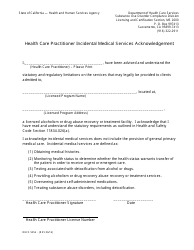
A: The purpose of Form CSD-004 is to request assistance from the California Department of Child Support Services (DCSS) in obtaining health care coverage for a child.
Q: Who can use Form CSD-004?
A: Health care providers in California can use Form CSD-004 to request assistance.
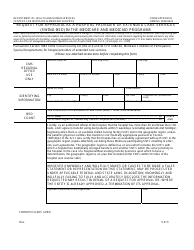
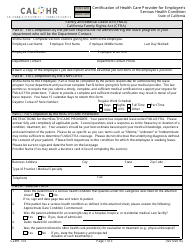
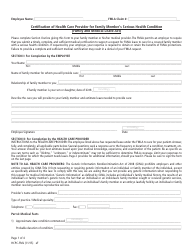
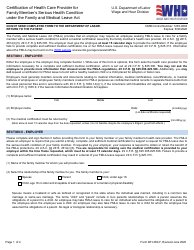
Q: What information is required on Form CSD-004?
A: Form CSD-004 requires information about the child, the custodial party, the noncustodial parent, the health care coverage being requested, and the health care provider.
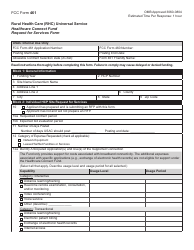
Q: How should I submit Form CSD-004?
A: Form CSD-004 should be completed and submitted to the California Department of Child Support Services (DCSS) by mail or fax.
Q: Is there a fee for submitting Form CSD-004?
A: No, there is no fee for submitting Form CSD-004.
Q: What happens after I submit Form CSD-004?
A: After submitting Form CSD-004, the California Department of Child Support Services (DCSS) will review the request and provide a response to the health care provider.
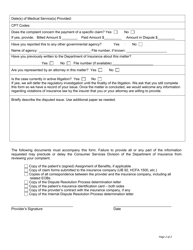
Q: Is Form CSD-004 confidential?
A: Yes, the information provided on Form CSD-004 is confidential and protected by law.
Q: Is there a deadline for submitting Form CSD-004?
A: There is no specific deadline for submitting Form CSD-004, but it is recommended to submit the form as soon as possible to avoid delays in obtaining health care coverage for the child.
Form Details:
- Released on January 7, 2019;
- The latest edition provided by the California Department of Insurance;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form CSD-004 by clicking the link below or browse more documents and templates provided by the California Department of Insurance.