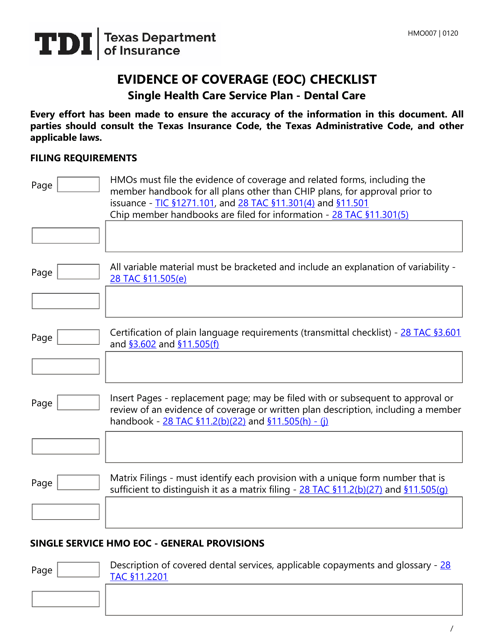
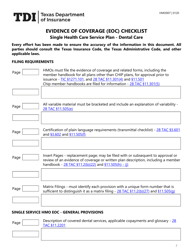
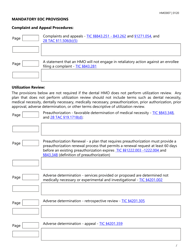
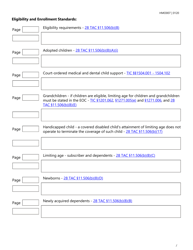
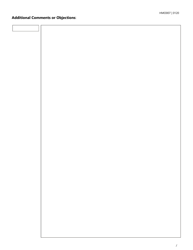
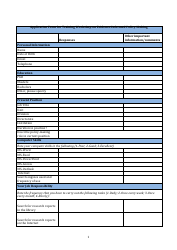
Form HMO007 Evidence of Coverage (Eoc) Checklist - Single Health Care Service Plan - Dental Care - Texas
What Is Form HMO007?
This is a legal form that was released by the Texas Department of Insurance - a government authority operating within Texas. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is HMO007?
A: HMO007 is an Evidence of Coverage (EOC) checklist for a Single Health Care Service Plan specifically for Dental Care in Texas.
Q: What is an Evidence of Coverage (EOC) checklist?
A: An Evidence of Coverage (EOC) checklist is a document that outlines the details of coverage provided by a health care service plan.
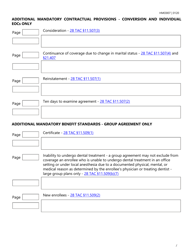
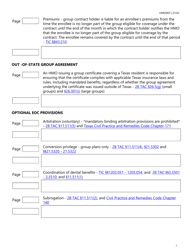
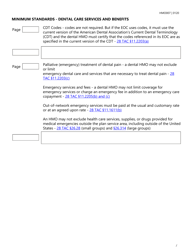
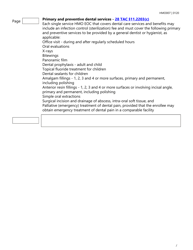
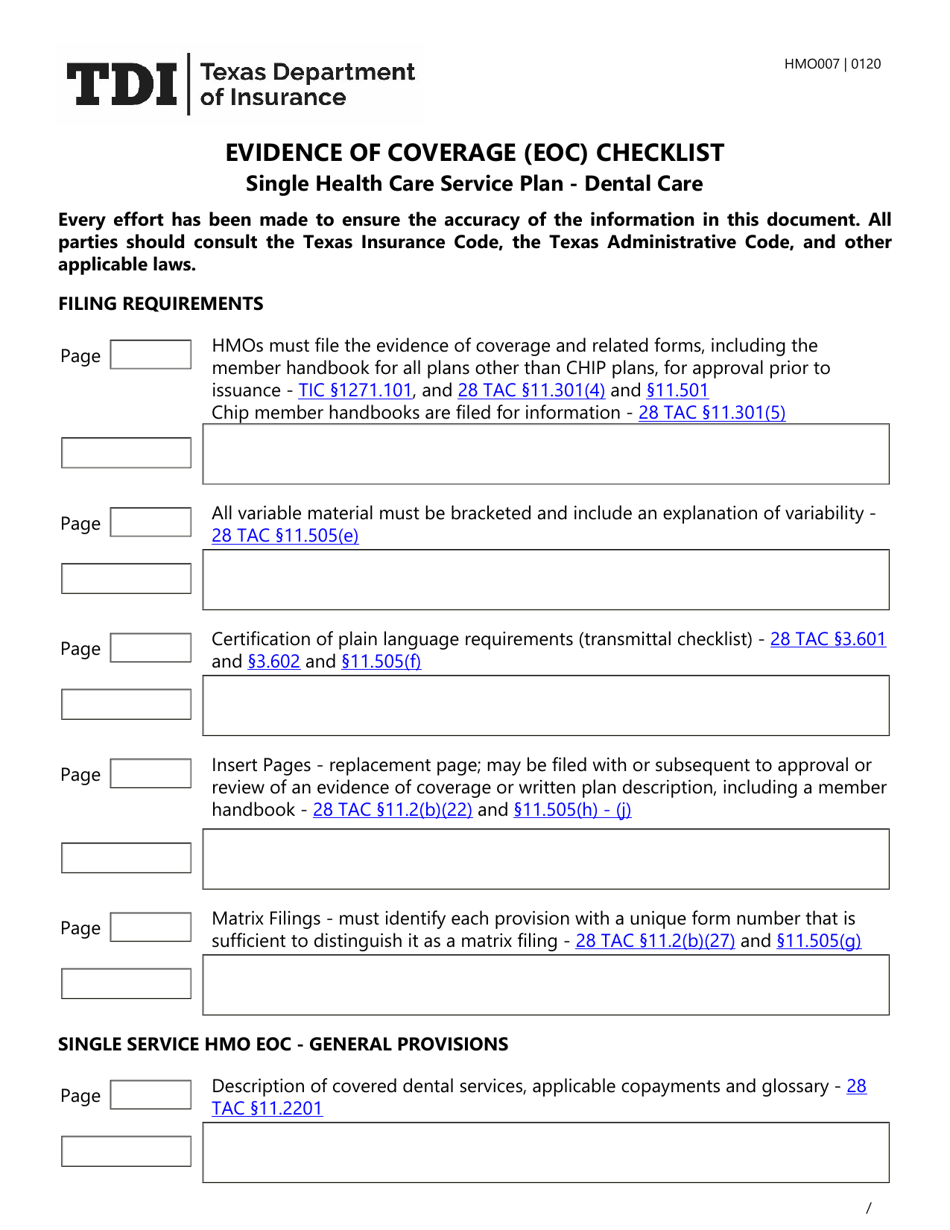
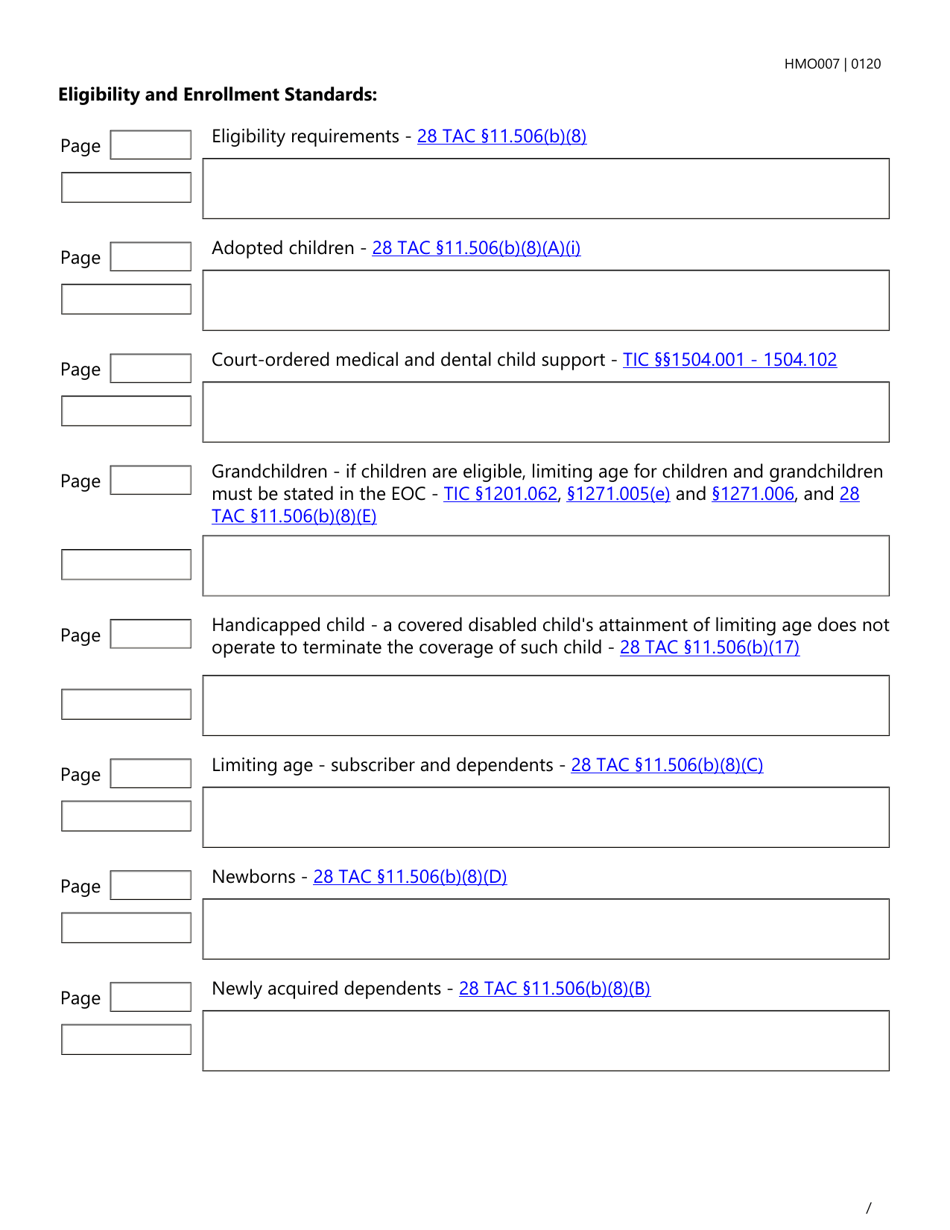
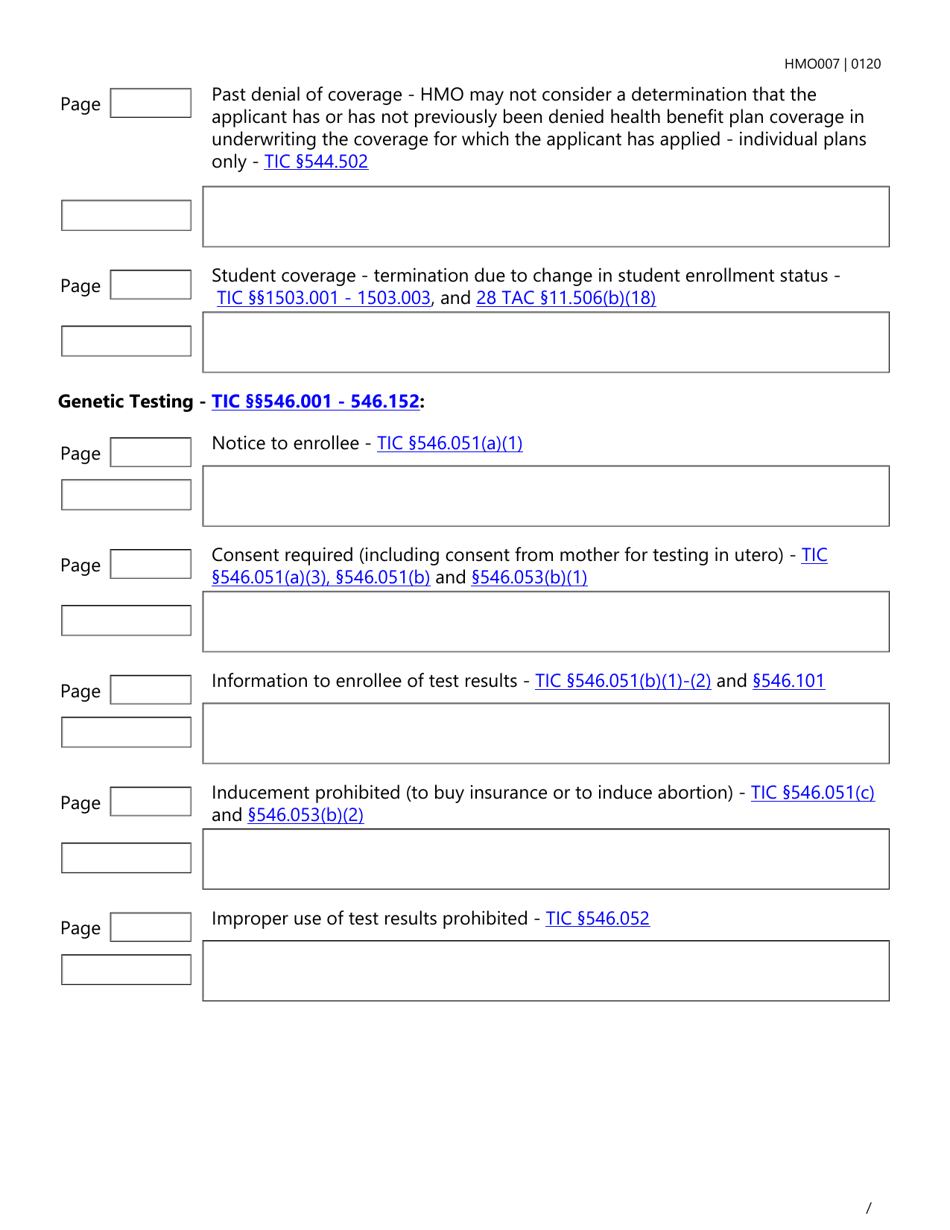
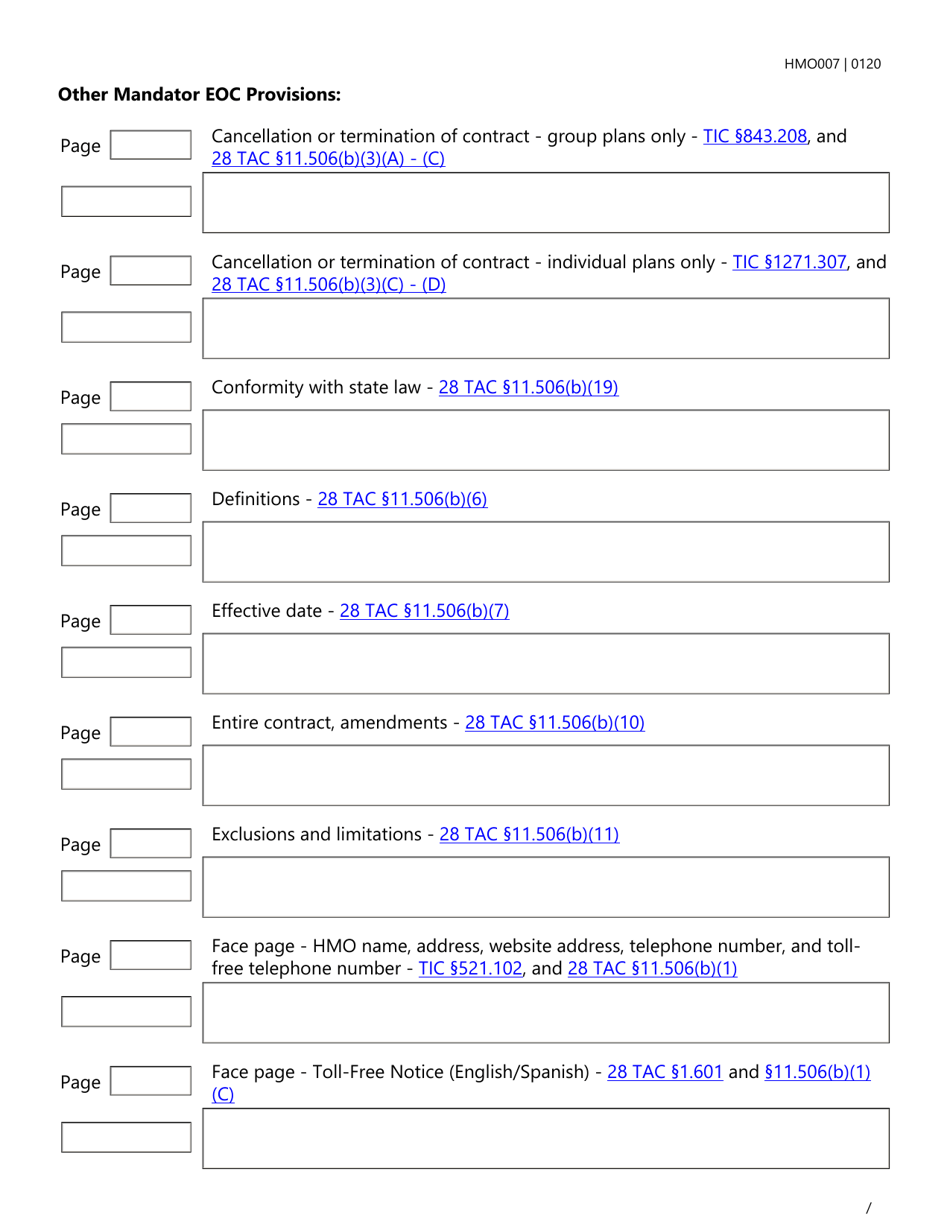
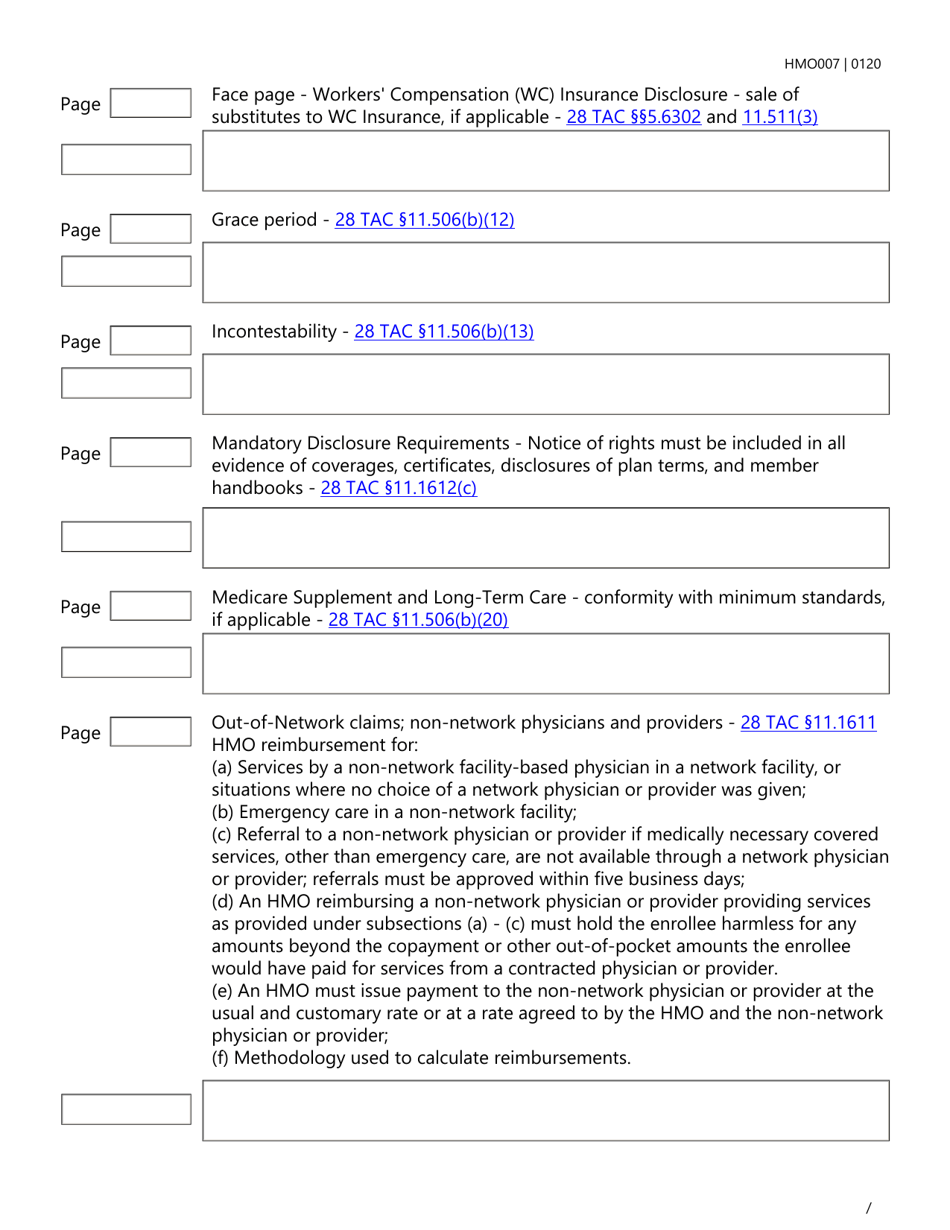
Q: What does the HMO007 EOC checklist cover?
A: The HMO007 EOC checklist specifically covers Dental Care services.
Q: Who is the intended audience for the HMO007 EOC checklist?
A: The HMO007 EOC checklist is intended for individuals who are choosing or already enrolled in a health care service plan that covers Dental Care in Texas.
Q: Why is the HMO007 EOC checklist important?
A: The HMO007 EOC checklist provides important information on the coverage details, benefits, limitations, and exclusions for Dental Care services.
Q: Is the HMO007 EOC checklist specific to Texas?
A: Yes, the HMO007 EOC checklist is specifically designed for Dental Care coverage in Texas.
Form Details:
- Released on January 1, 2020;
- The latest edition provided by the Texas Department of Insurance;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form HMO007 by clicking the link below or browse more documents and templates provided by the Texas Department of Insurance.