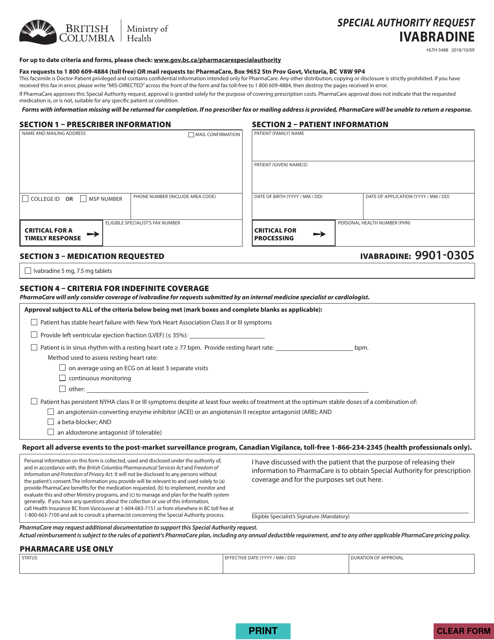
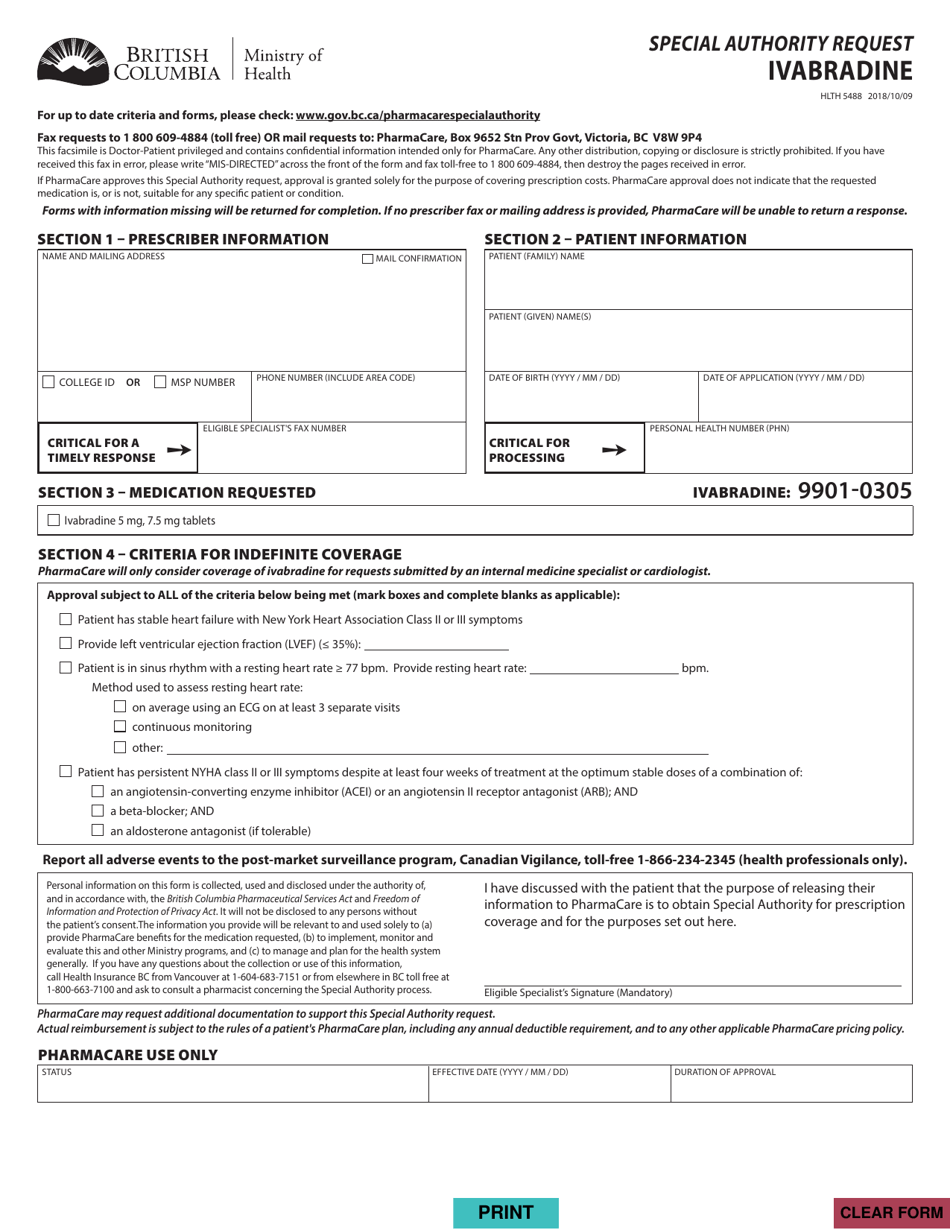
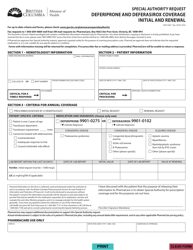
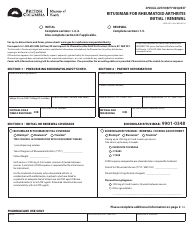
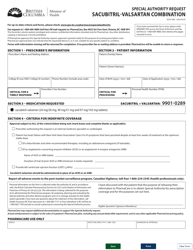
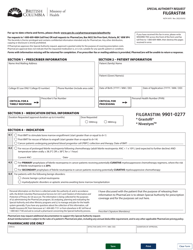
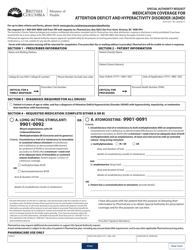
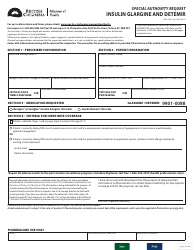
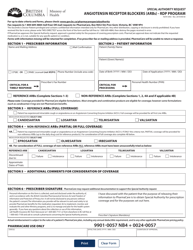
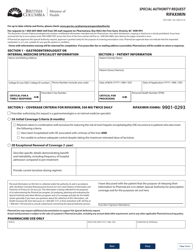
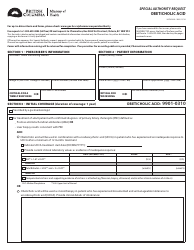
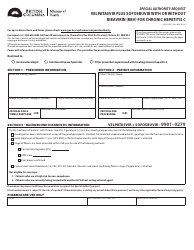
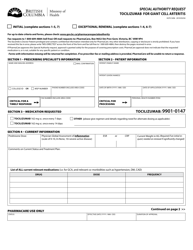
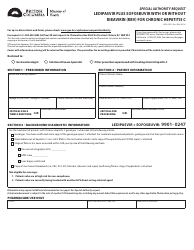
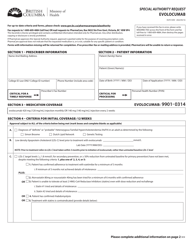
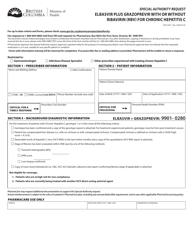
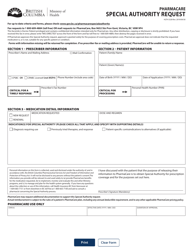
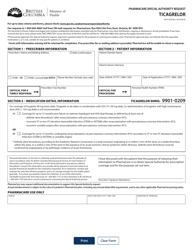
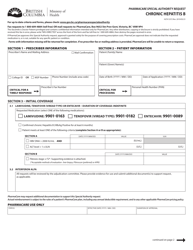
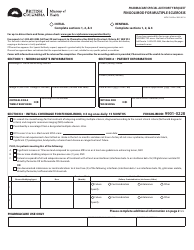
Form HLTH5488 Special Authority Request - Ivabradine - British Columbia, Canada
Form HLTH5488 Special Authority Request - Ivabradine is used in the province of British Columbia, Canada. It is a form for requesting special authority to access the medication Ivabradine. Special authority requests are typically made when a medication is not covered under the regular drug benefits program but is necessary for a patient's specific medical condition. Ivabradine is a medication used to treat chronic heart failure and is prescribed under certain circumstances.
The Form HLTH5488 Special Authority Request - Ivabradine in British Columbia, Canada is typically filed by healthcare professionals such as physicians or nurse practitioners on behalf of their patients. It is used to request special authority coverage for the medication Ivabradine, which is used to treat certain heart conditions.
FAQ
Q: What is a Special Authority Request?
A: A Special Authority Request is a process in British Columbia, Canada, where physicians can request coverage for medications that are not normally covered by the provincial government's drug benefit program.
Q: What is Ivabradine?
A: Ivabradine is a medication used to treat certain heart conditions, such as chronic heart failure and chronic stable angina.
Q: Why would someone need to submit a Special Authority Request for Ivabradine?
A: Ivabradine is not automatically covered by the provincial government's drug benefit program in British Columbia. Therefore, patients would need to submit a Special Authority Request to request coverage for this medication.
Q: Who can submit a Special Authority Request?
A: Special Authority Requests can be submitted by physicians on behalf of their patients.
Q: How can a physician submit a Special Authority Request for Ivabradine?
A: Physicians can submit a Special Authority Request for Ivabradine by completing the appropriate form, such as the HLTH5488 form, and submitting it to the provincial government's drug program.
Q: What information is required in a Special Authority Request for Ivabradine?
A: A Special Authority Request for Ivabradine typically requires information such as the patient's name, contact information, relevant medical history, diagnosis, and any supporting documentation or justification for the request.
Q: What happens after a Special Authority Request for Ivabradine is submitted?
A: After a Special Authority Request for Ivabradine is submitted, it will be reviewed by the provincial government's drug program to determine if coverage will be approved. The physician and patient will be notified of the decision.
Q: Is there a fee for submitting a Special Authority Request for Ivabradine?
A: There is no fee for submitting a Special Authority Request for Ivabradine in British Columbia.
Q: How long does it take to receive a decision on a Special Authority Request for Ivabradine?
A: The time it takes to receive a decision on a Special Authority Request for Ivabradine can vary. It usually takes several weeks for the request to be reviewed and a decision to be made.
Q: What happens if a Special Authority Request for Ivabradine is approved?
A: If a Special Authority Request for Ivabradine is approved, the medication will be covered under the provincial government's drug benefit program and the patient will be able to obtain the medication with coverage.
Q: What happens if a Special Authority Request for Ivabradine is denied?
A: If a Special Authority Request for Ivabradine is denied, the patient and physician will be notified of the denial. The patient may have to explore other options for obtaining the medication, such as private insurance coverage or self-payment.