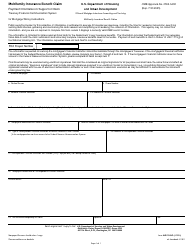
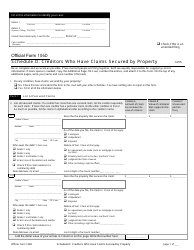
Instructions for Waiver / Rehab Claim Form - Rhode Island
This document was released by Rhode Island Executive Office of Health and Human Services and contains official instructions for Waiver/Rehab Claim Form . The up-to-date fillable form is available for download through this link.
FAQ
Q: What is a Waiver/Rehab Claim Form?
A: A Waiver/Rehab Claim Form is a document used to request a waiver or rehabilitation of a specific requirement or policy.
Q: Why would I need to submit a Waiver/Rehab Claim Form?
A: You would need to submit a Waiver/Rehab Claim Form if you are seeking an exception to a certain requirement or policy.
Q: How can I obtain a Waiver/Rehab Claim Form?
A: You can obtain a Waiver/Rehab Claim Form by contacting the relevant department or agency responsible for the requirement or policy you are seeking a waiver or rehabilitation for.
Q: What information should I include in a Waiver/Rehab Claim Form?
A: You should include your personal information, the specific requirement or policy you are seeking a waiver or rehabilitation for, and any supporting documentation that may be required.
Q: Is there a deadline for submitting a Waiver/Rehab Claim Form?
A: There may be a deadline for submitting a Waiver/Rehab Claim Form. It is important to check with the relevant department or agency for any specific deadlines or timeframes.
Q: How long does it take to process a Waiver/Rehab Claim Form?
A: The processing time for a Waiver/Rehab Claim Form can vary. It is best to check with the relevant department or agency for an estimated timeframe.
Q: What happens after I submit a Waiver/Rehab Claim Form?
A: After you submit a Waiver/Rehab Claim Form, it will be reviewed by the relevant department or agency. They will determine whether to grant the waiver or rehabilitation based on the information provided.
Q: Can a Waiver/Rehab Claim be denied?
A: Yes, a Waiver/Rehab Claim can be denied if the department or agency determines that the request does not meet the necessary requirements or criteria.
Q: Can I appeal a denial of a Waiver/Rehab Claim?
A: Yes, you may be able to appeal a denial of a Waiver/Rehab Claim. The specific appeals process will vary depending on the department or agency handling the request.
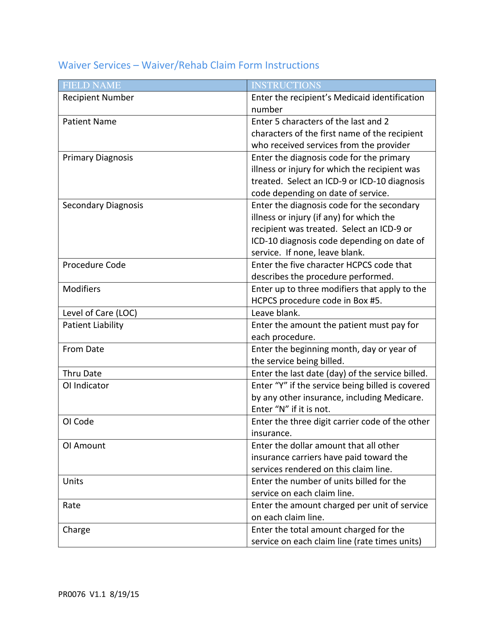
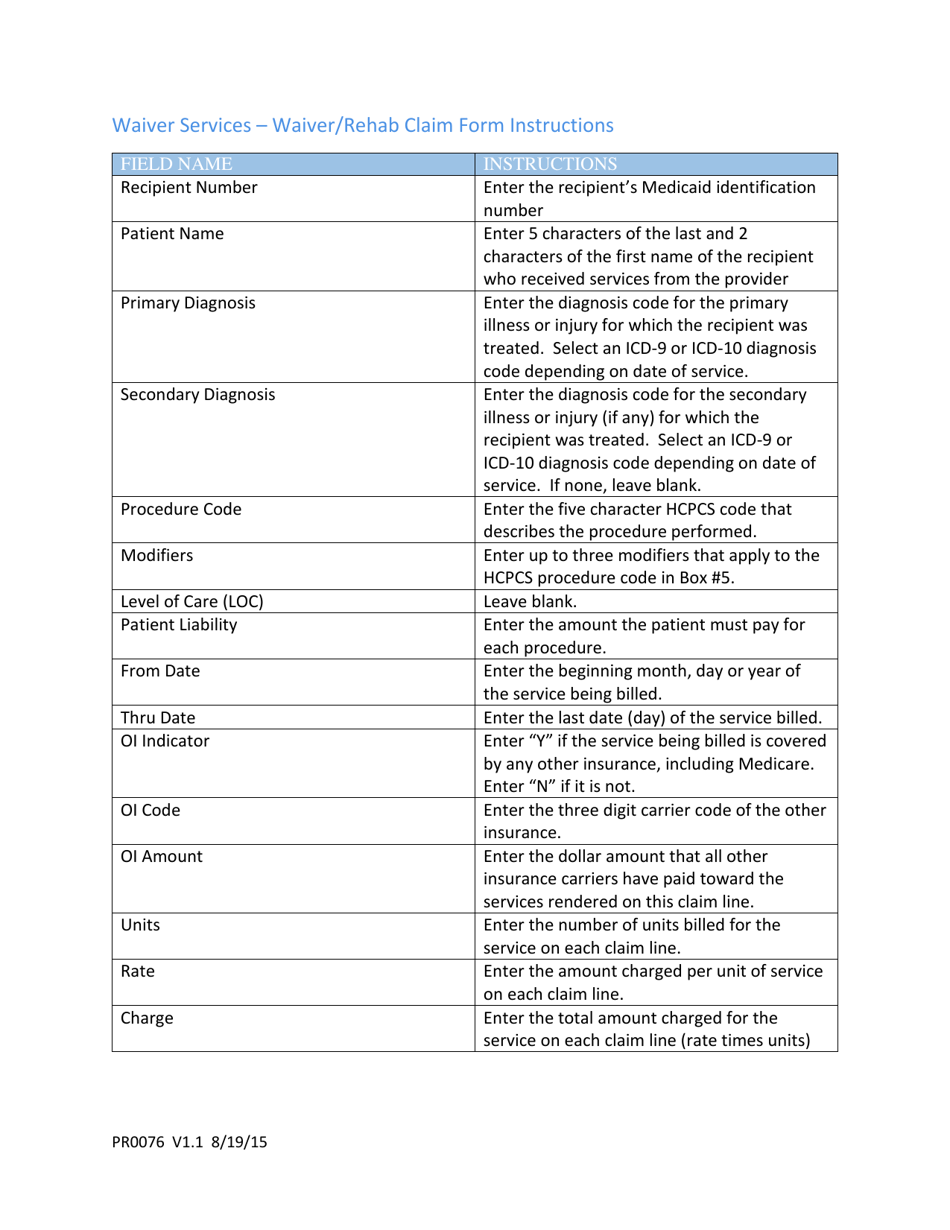
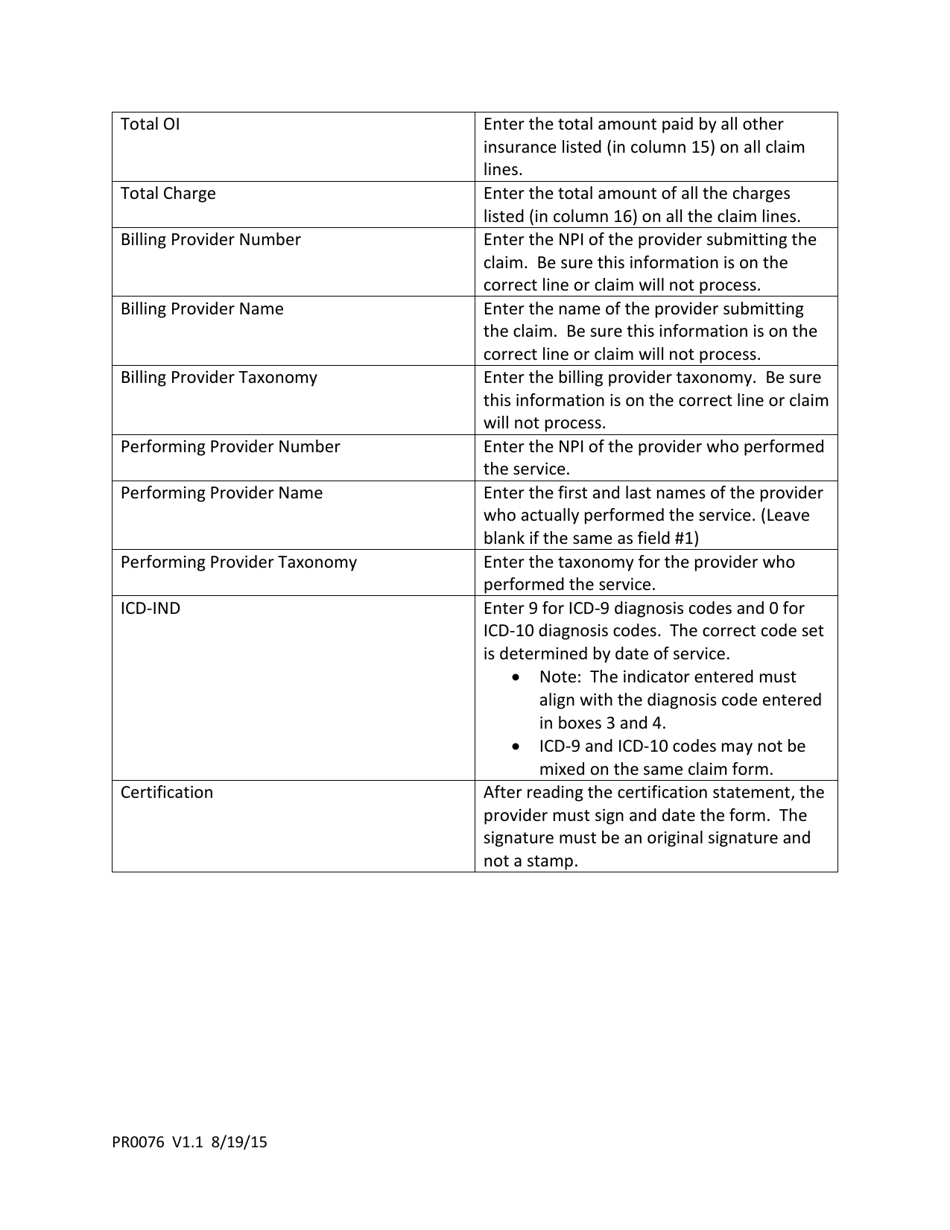
Instruction Details:
- This 2-page document is available for download in PDF;
- Actual and applicable for the current year;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library legal documents released by the Rhode Island Executive Office of Health and Human Services.