This version of the form is not currently in use and is provided for reference only. Download this version of
Form BCRF-1
for the current year.
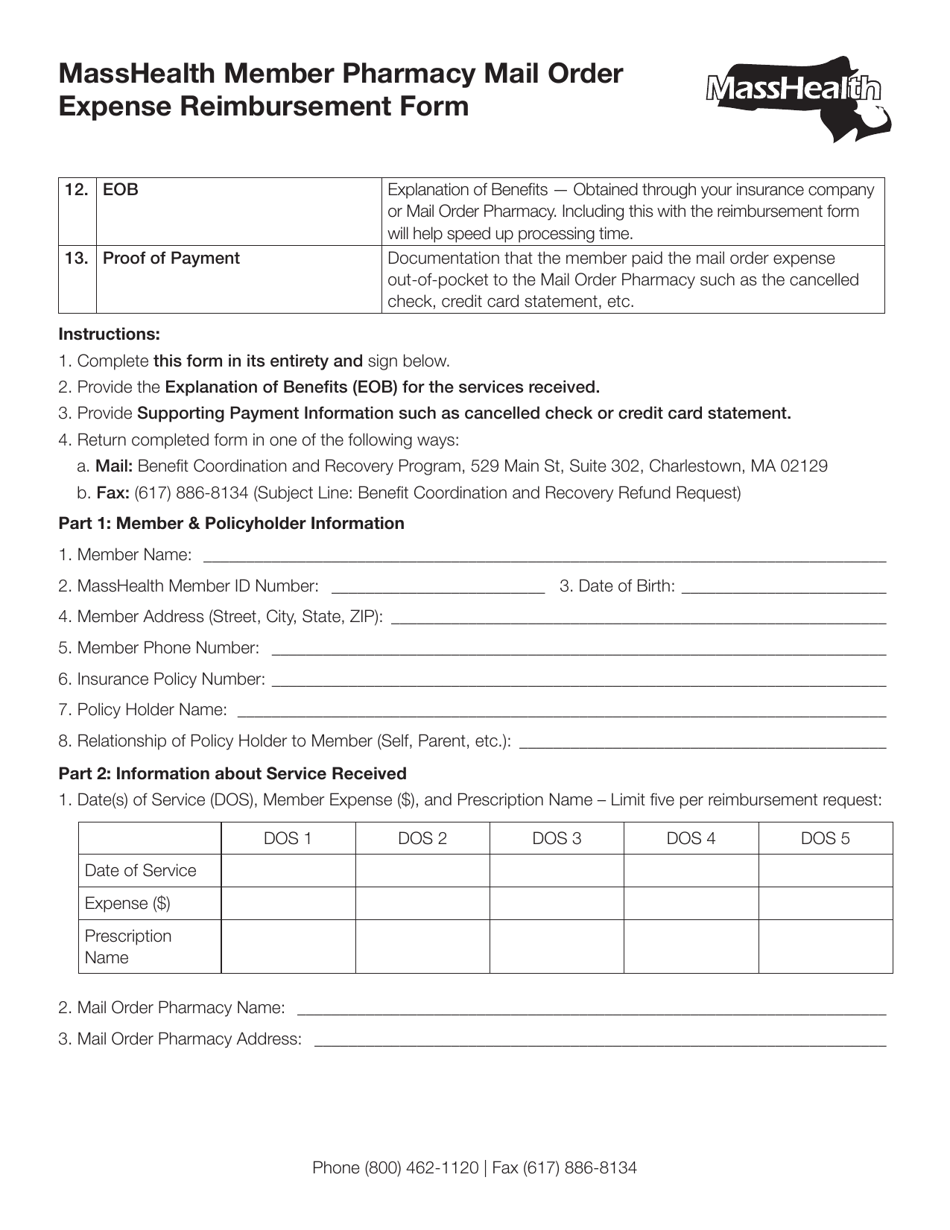
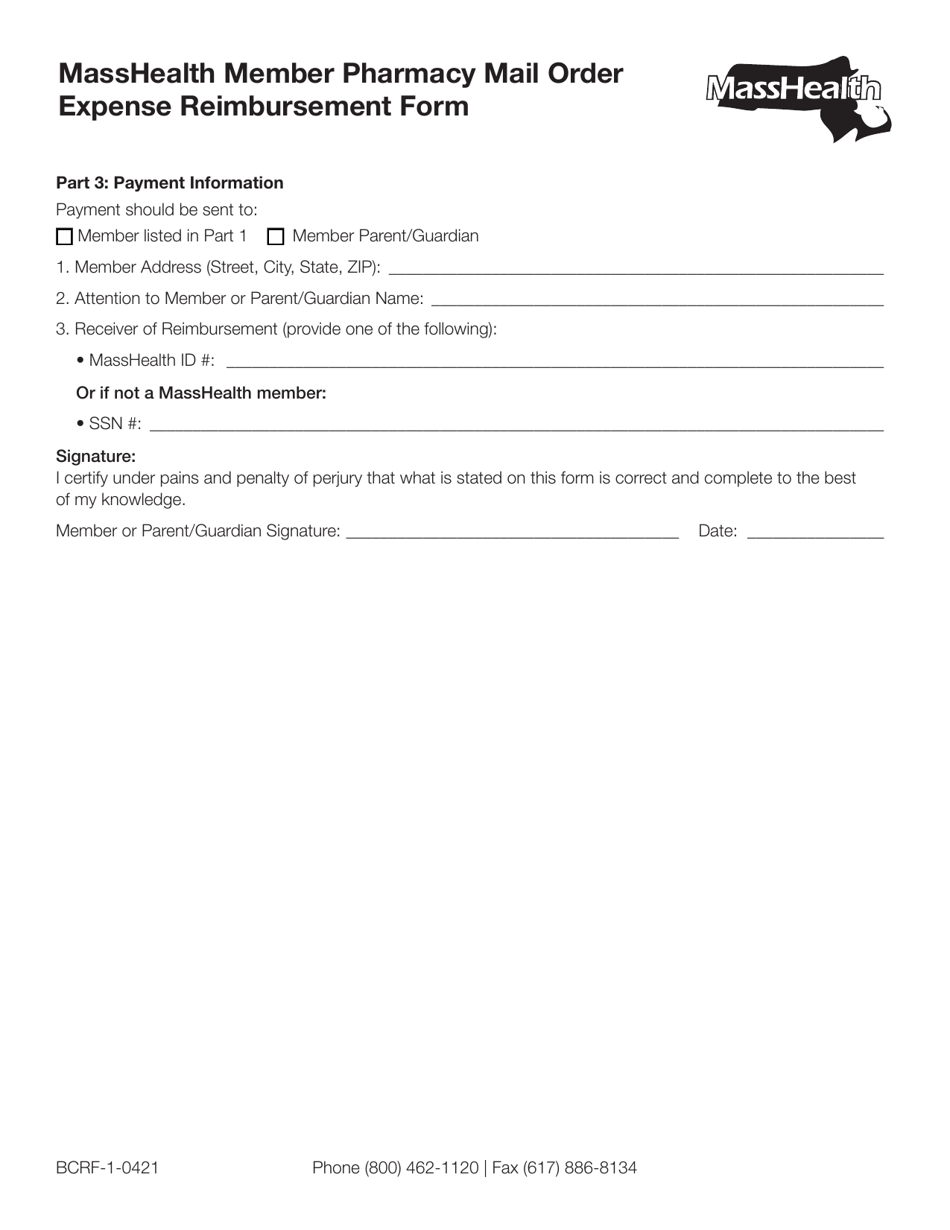
Form BCRF-1 Masshealth Member Pharmacy Mail Order Expense Reimbursement Form - Massachusetts
Fill PDF Online
Fill out online for free
without registration or credit card
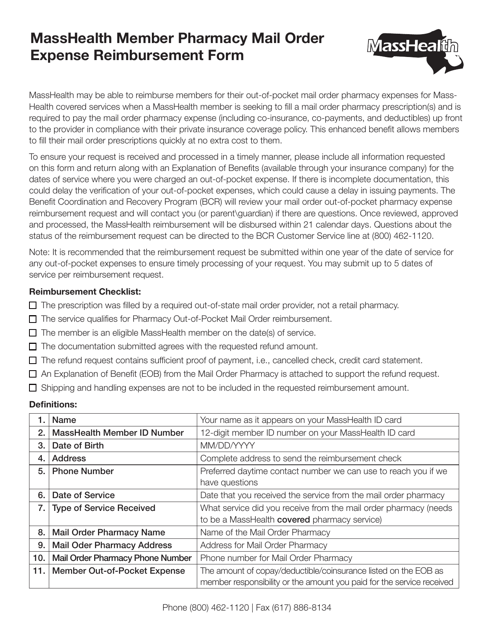
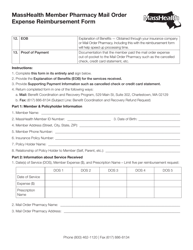
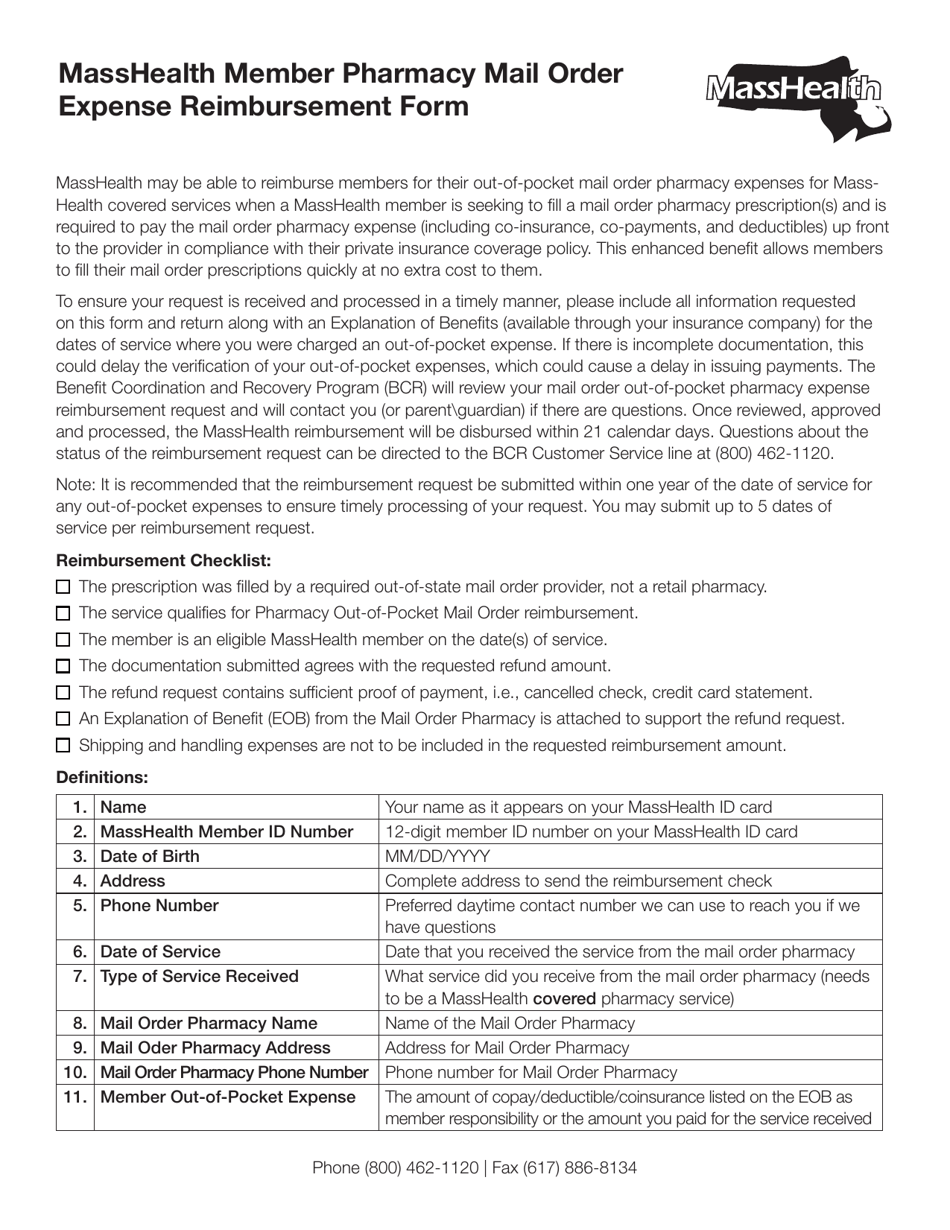
What Is Form BCRF-1?
This is a legal form that was released by the Massachusetts MassHealth - a government authority operating within Massachusetts. As of today, no separate filing guidelines for the form are provided by the issuing department.
Form Details:
- Released on April 1, 2021;
- The latest edition provided by the Massachusetts MassHealth;
- Easy to use and ready to print;
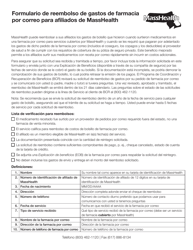
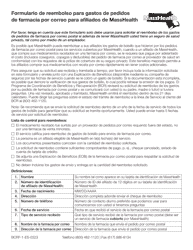
- Available in Spanish;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form BCRF-1 by clicking the link below or browse more documents and templates provided by the Massachusetts MassHealth.