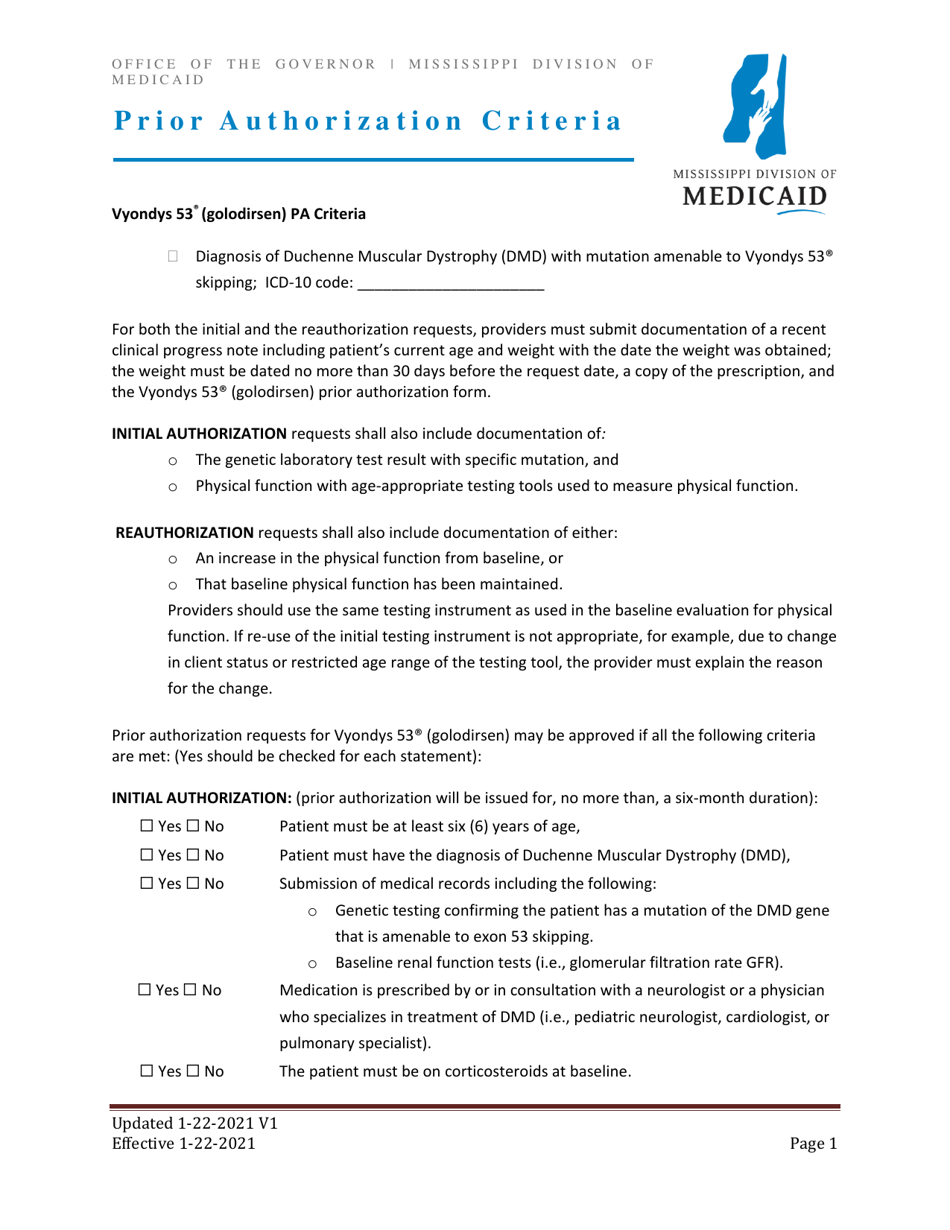
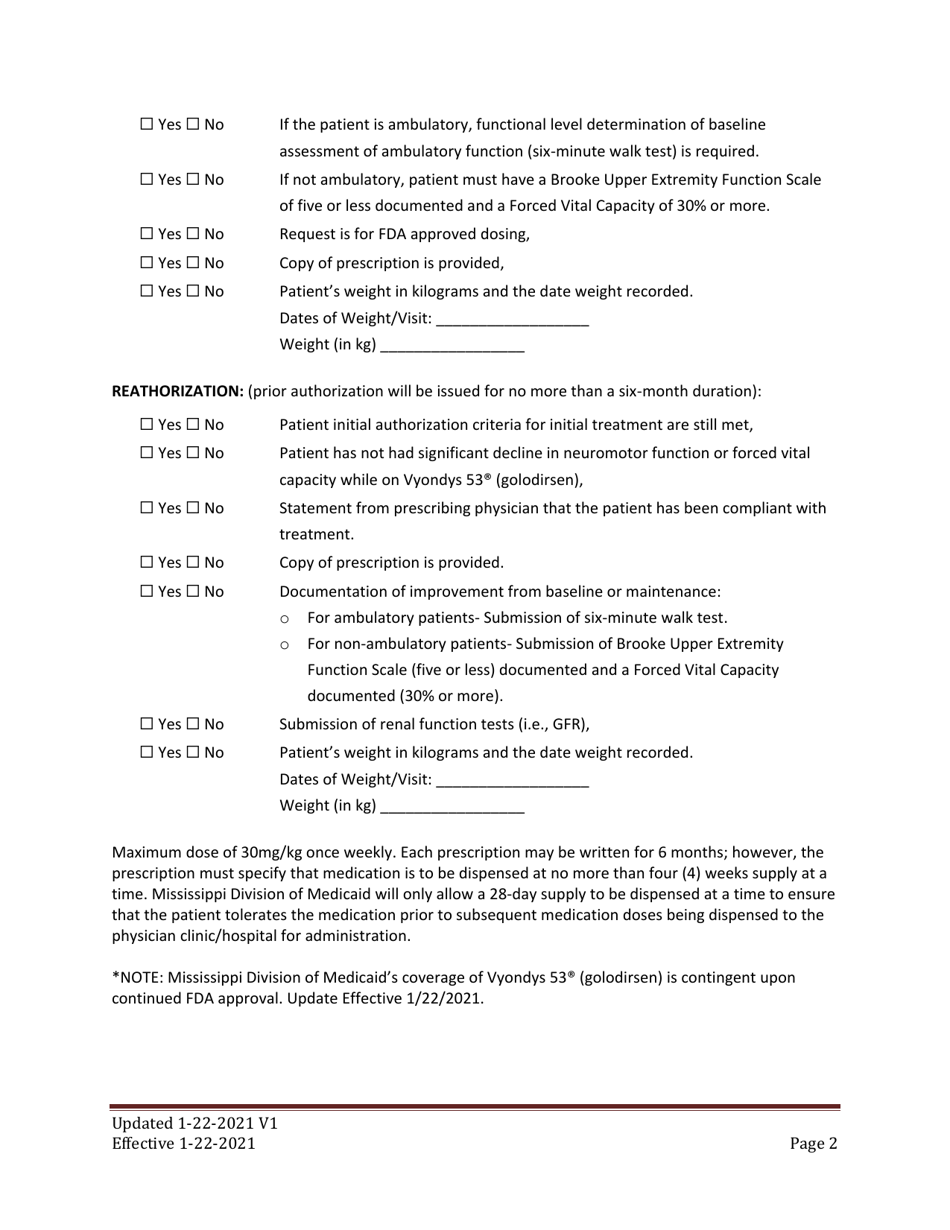
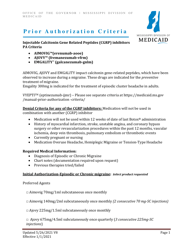
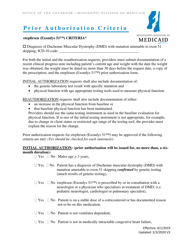
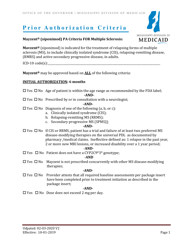
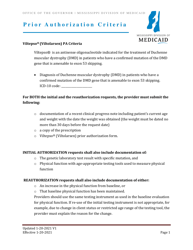
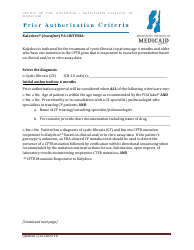
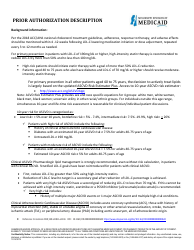
Prior Authorization Criteria - Vyondys 53 (Golodirsen) - Mississippi
Prior Authorization Criteria - Vyondys 53 (Golodirsen) is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
Q: What is Vyondys 53 (Golodirsen)?
A: Vyondys 53 (Golodirsen) is a medication used to treat certain patients with Duchenne muscular dystrophy (DMD).
Q: What is Prior Authorization?
A: Prior Authorization is a process by which your healthcare provider needs to get approval from your insurance company before they can prescribe Vyondys 53 (Golodirsen).
Q: Why is Prior Authorization required?
A: Insurance companies typically require Prior Authorization to ensure that medications like Vyondys 53 (Golodirsen) are being prescribed appropriately and are medically necessary.
Q: Who needs Prior Authorization for Vyondys 53 (Golodirsen)?
A: Certain patients with Duchenne muscular dystrophy (DMD) may need Prior Authorization for Vyondys 53 (Golodirsen). Your healthcare provider can determine if you are eligible.
Q: How can my healthcare provider request Prior Authorization?
A: Your healthcare provider will need to contact your insurance company and provide the necessary documentation and information to request Prior Authorization for Vyondys 53 (Golodirsen).
Q: What criteria do insurance companies use for Prior Authorization of Vyondys 53 (Golodirsen) in Mississippi?
A: The specific criteria used for Prior Authorization of Vyondys 53 (Golodirsen) in Mississippi may vary. It is best to contact your insurance company or healthcare provider for the most accurate information.
Q: What if my Prior Authorization for Vyondys 53 (Golodirsen) is denied?
A: If your Prior Authorization for Vyondys 53 (Golodirsen) is denied, you may have options to appeal the decision. Your healthcare provider can assist you with the appeals process.
Q: Is Vyondys 53 (Golodirsen) covered by insurance?
A: Coverage for Vyondys 53 (Golodirsen) may vary depending on your insurance plan. It is important to check with your insurance company to determine your coverage.
Q: How much does Vyondys 53 (Golodirsen) cost?
A: The cost of Vyondys 53 (Golodirsen) may vary. It is best to check with your healthcare provider or pharmacy for the most accurate pricing information.
Q: Are there any assistance programs available for Vyondys 53 (Golodirsen)?
A: There may be assistance programs available for Vyondys 53 (Golodirsen) to help with the cost. You can reach out to the manufacturer of Vyondys 53 (Golodirsen) or your healthcare provider for more information.
Form Details:
- Released on January 22, 2021;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.