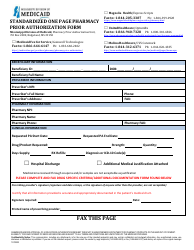
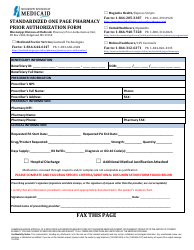
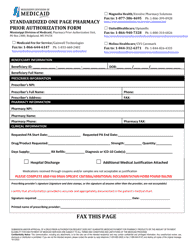
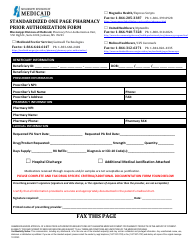
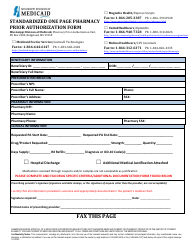
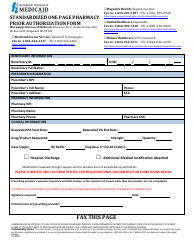
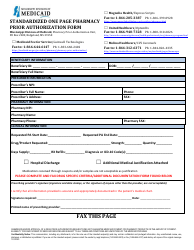
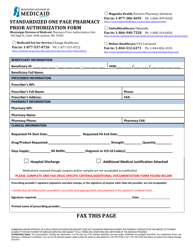
Prior Authorization Packet - Growth Hormone - Mississippi
Prior Authorization Packet - Growth Hormone is a legal document that was released by the Mississippi Division of Medicaid - a government authority operating within Mississippi.
FAQ
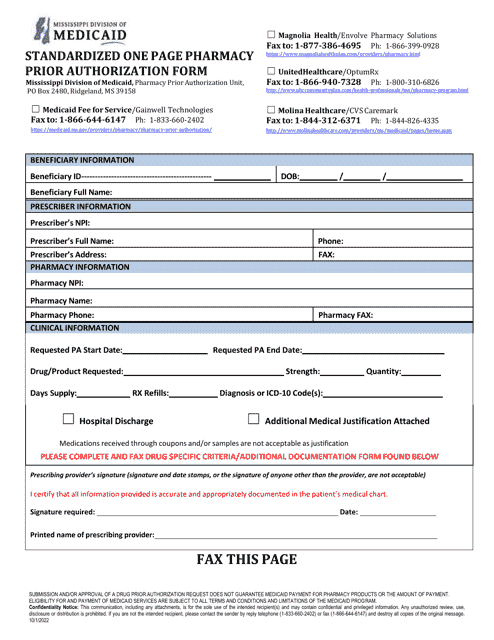
Q: What is a prior authorization packet?
A: A prior authorization packet is a collection of documents required by the insurance company to determine coverage for a specific medication or procedure.
Q: What is growth hormone?
A: Growth hormone is a hormone produced by the pituitary gland that stimulates growth, cell reproduction, and regeneration in humans.
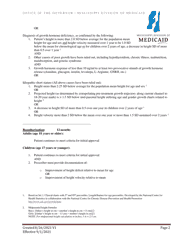
Q: Why would someone need growth hormone therapy?
A: Someone may need growth hormone therapy if they have a deficiency in growth hormone, which can cause stunted growth or other health issues.
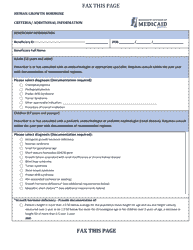
Q: What is the purpose of the prior authorization packet for growth hormone?
A: The purpose of the prior authorization packet for growth hormone is to provide the insurance company with the necessary information to determine if the therapy is medically necessary and should be covered.
Q: What documents are typically included in a growth hormone prior authorization packet?
A: Typically, a growth hormone prior authorization packet includes medical records, a prescription, documentation of growth hormone deficiency, and any other relevant clinical information.
Q: How long does it take for the insurance company to review a growth hormone prior authorization packet?
A: The time it takes for the insurance company to review a growth hormone prior authorization packet can vary, but it generally takes a few weeks.
Q: What happens if the prior authorization is approved?
A: If the prior authorization is approved, the insurance company will provide coverage for the growth hormone therapy.
Q: What happens if the prior authorization is denied?
A: If the prior authorization is denied, the insurance company will not provide coverage for the growth hormone therapy. However, there may be an appeal process available.
Q: Are there any alternative options to insurance coverage for growth hormone therapy?
A: Yes, there are alternative options to insurance coverage for growth hormone therapy, such as patient assistance programs or financial assistance programs offered by the medication manufacturer.
Q: Is a prior authorization packet required for every prescription medication?
A: No, a prior authorization packet is not required for every prescription medication. It is typically required for medications that are considered expensive or have specific usage guidelines.
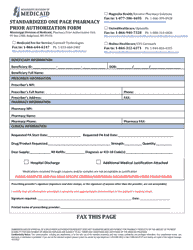
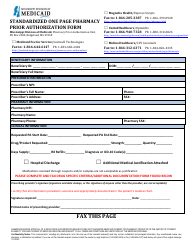
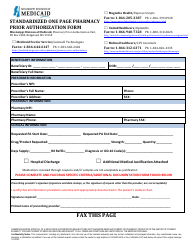
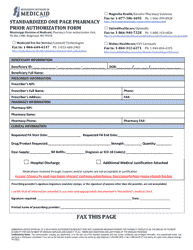
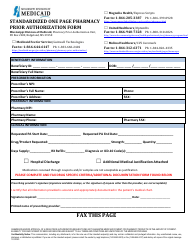
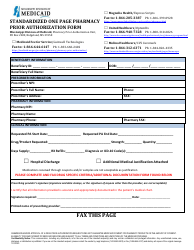
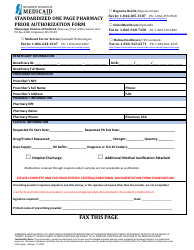
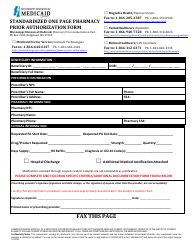
Form Details:
- Released on October 1, 2022;
- The latest edition currently provided by the Mississippi Division of Medicaid;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Mississippi Division of Medicaid.