Prior Authorization Templates
Prior authorization is a process used by health insurance companies to determine if they will cover the cost of certain medications, procedures, or treatments. It requires healthcare providers to obtain approval from the insurance company before they can proceed with a particular service or medication. The purpose of prior authorization is to ensure that the requested treatment is medically necessary, appropriate, and cost-effective. It helps insurance companies manage healthcare costs by ensuring that only necessary and effective treatments are covered.
Documents:
390
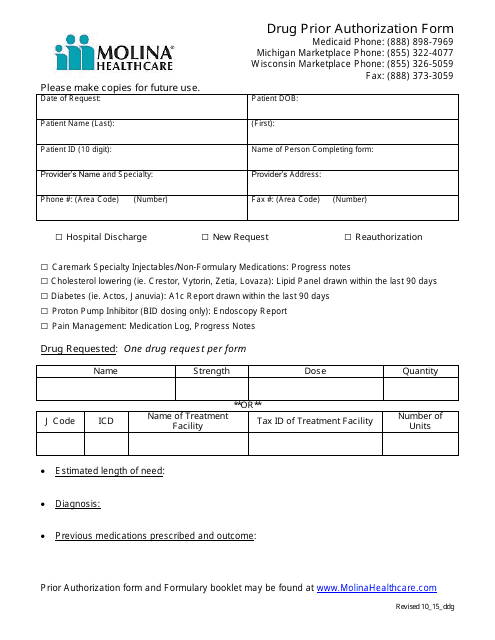
This form is used for requesting prior authorization for drugs through Molina Healthcare.
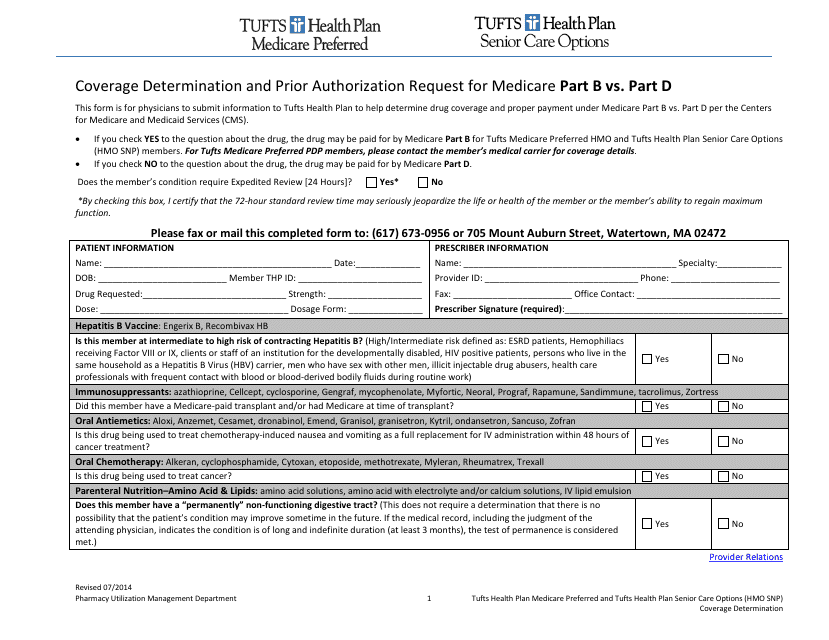
This Form is used for submitting a coverage determination request or prior authorization request for Medicare Part B or Part D benefits under Tufts insurance.
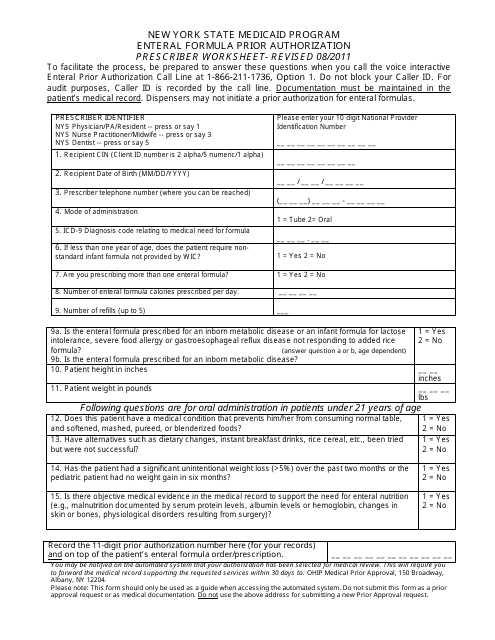
This Form is used for prior authorization of enteral formula prescription in the New York State Medicaid Program.
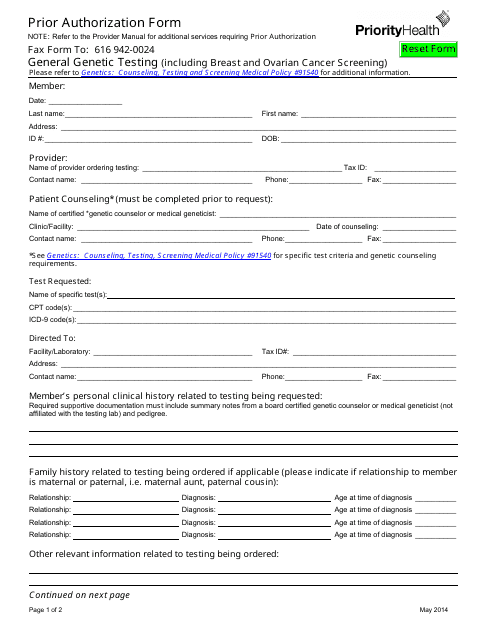
This form is used for requesting prior authorization from Priority Health for certain medical treatments or services.
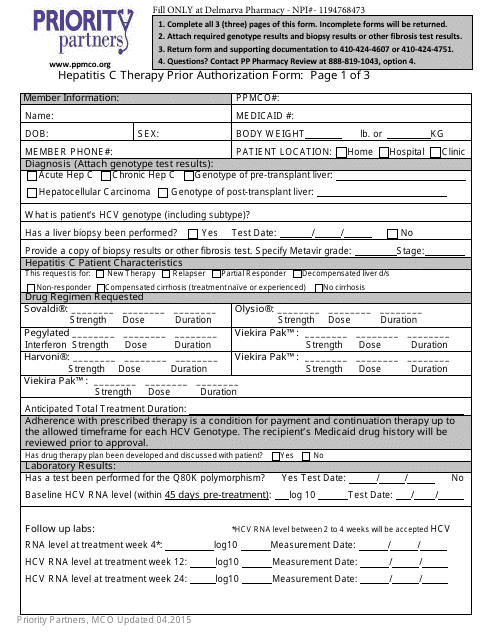
This form is used to request prior authorization for Hepatitis C therapy with Priority Partners.
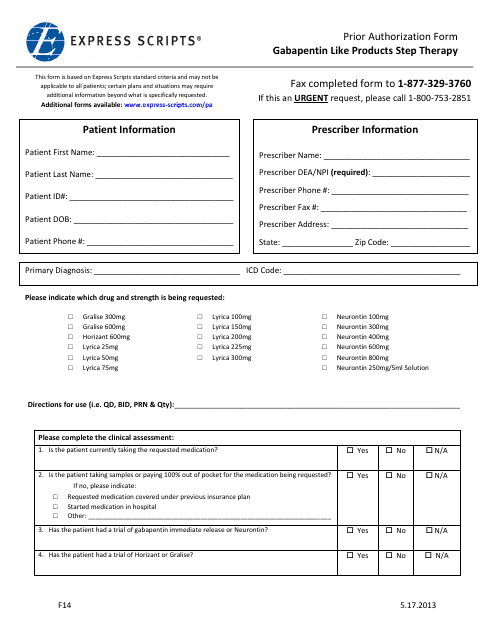
This form is used for requesting prior authorization for Gabapentin-like products through Express Scripts' step therapy program.
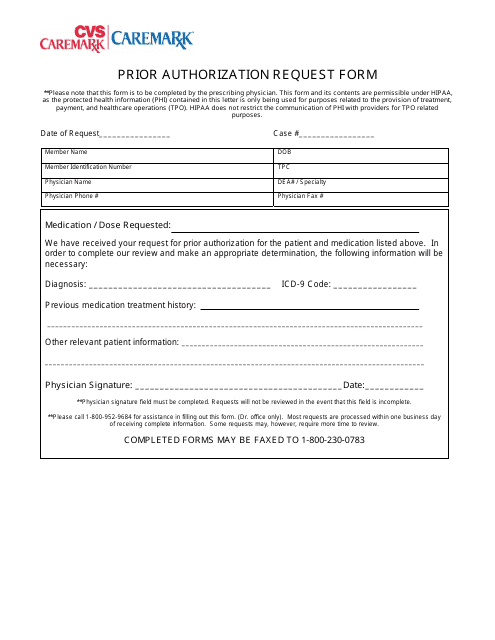
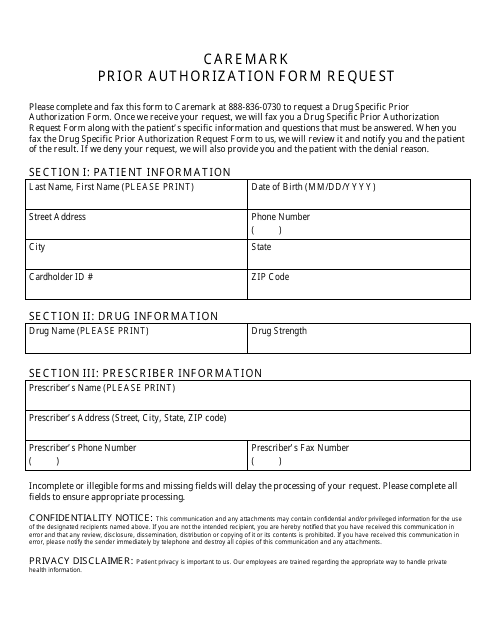
This Form is used for requesting prior authorization for medications through CVS Caremark.
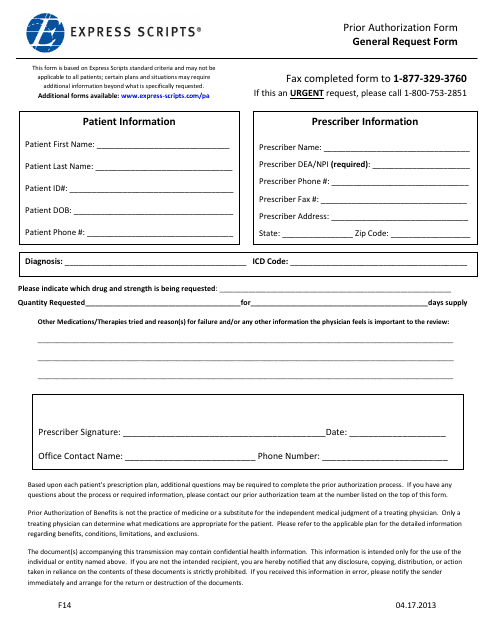
This form is used for requesting prior authorization from Express Scripts for medications or medical treatments.
This Form is used for requesting prior authorization for medications through Cvs Caremark.
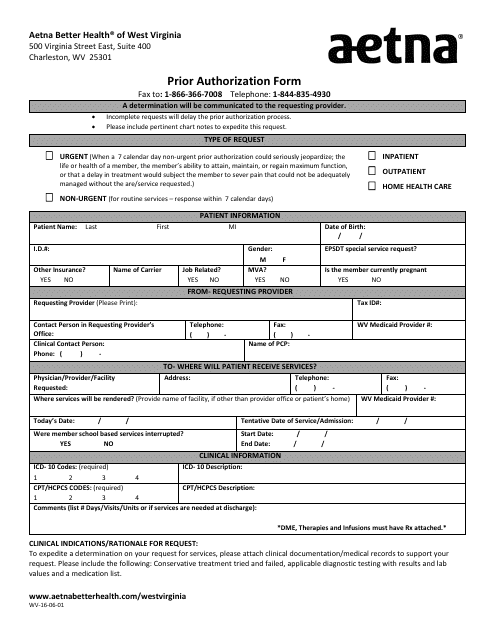
This form is used for obtaining prior authorization from Aetna for medical services in Charleston, West Virginia.
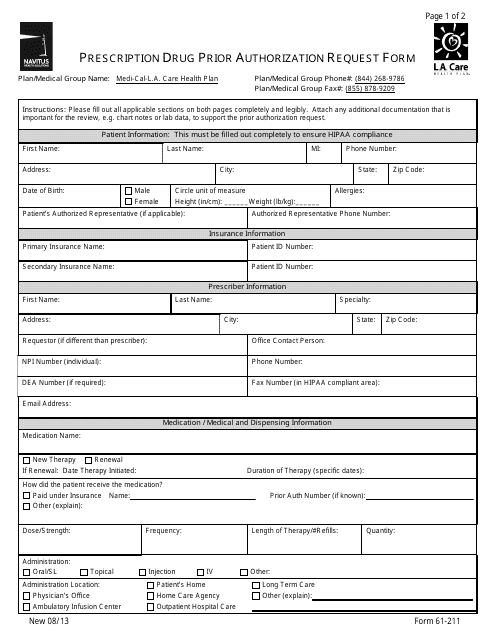
This form is used for requesting prior authorization for prescription drugs from L.A. Care Health Plan.
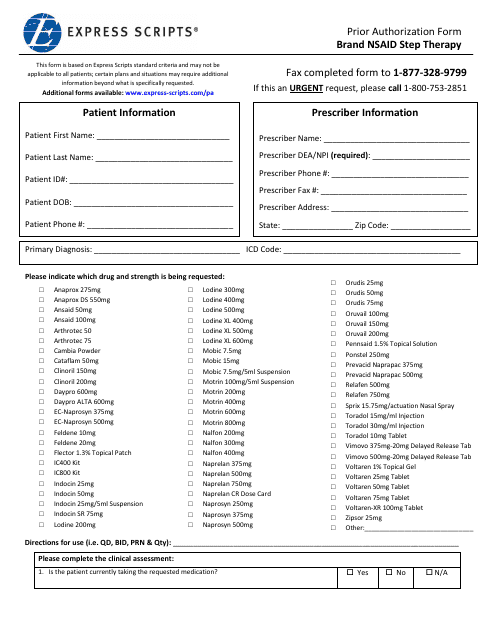
This Form is used for requesting prior authorization for brand name nonsteroidal anti-inflammatory drugs (NSAIDs) as part of step therapy process through Express Scripts.
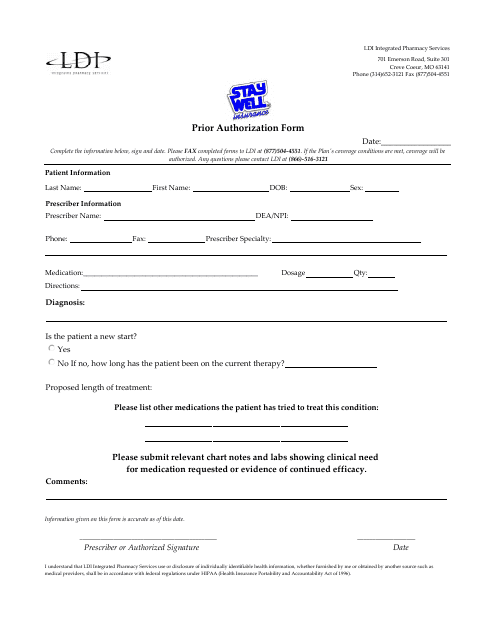
This form is used for requesting prior authorization for medications through LDI Integrated Pharmacy Services in Missouri.
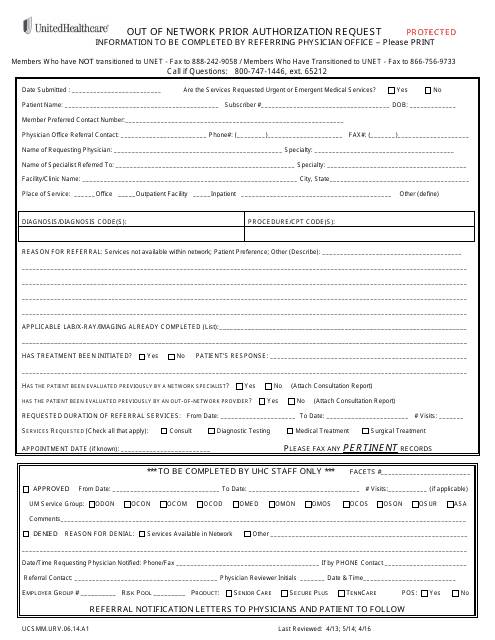
This document is a form used by Unitedhealthcare to request prior authorization for out-of-network healthcare services.
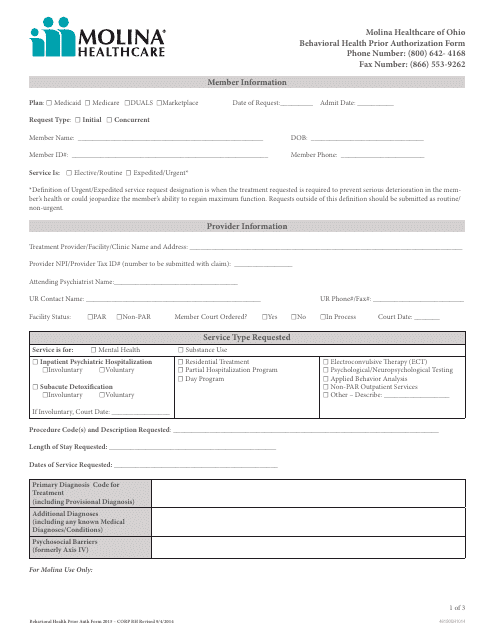
This Form is used for obtaining prior authorization for behavioral health services from Molina Healthcare in Ohio.
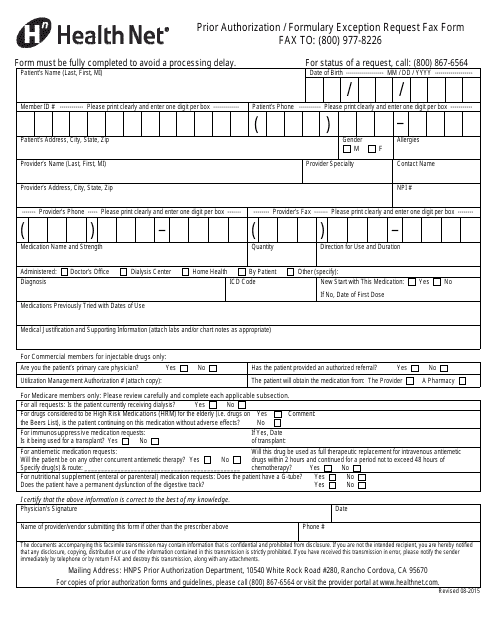
This form is used for requesting prior authorization or formulary exception from Health Net through fax.
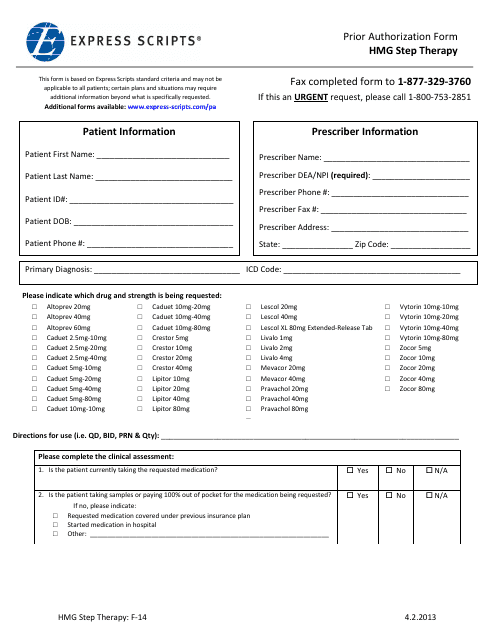
This form is used for requesting prior authorization for HMG step therapy through Express Scripts.
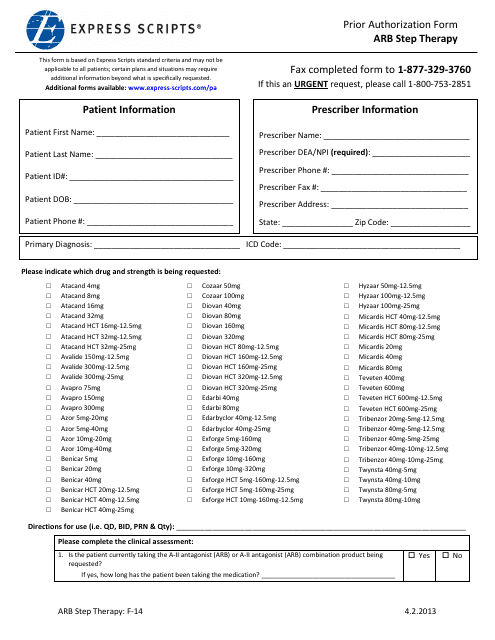
This form is used for obtaining prior authorization for step therapy through Express Scripts. Step therapy is a cost-saving measure that requires patients to try lower-cost medications before progressing to more expensive options.
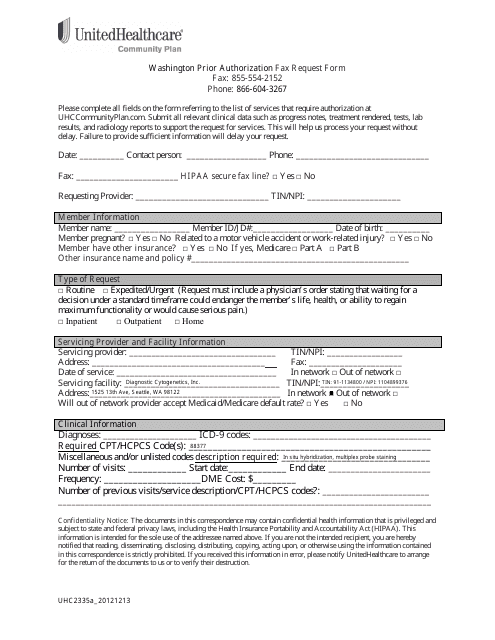
This Form is used for requesting prior authorization for healthcare services from UnitedHealthcare in Washington.
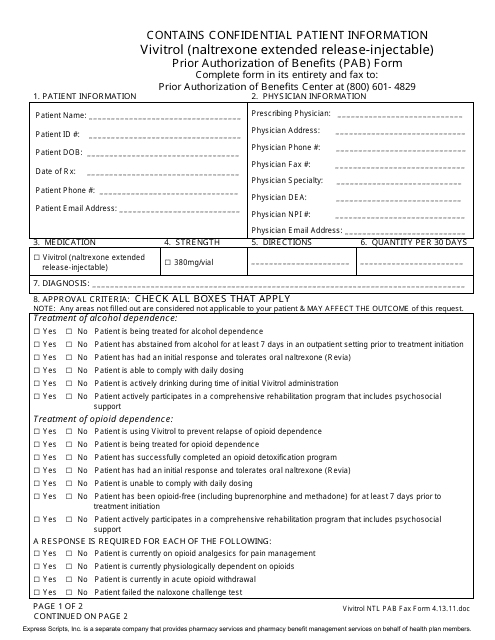
This Form is used for requesting prior authorization of benefits for Vivitrol, a medication for alcohol and opioid dependence. It is an extended-release injectable form of naltrexone.
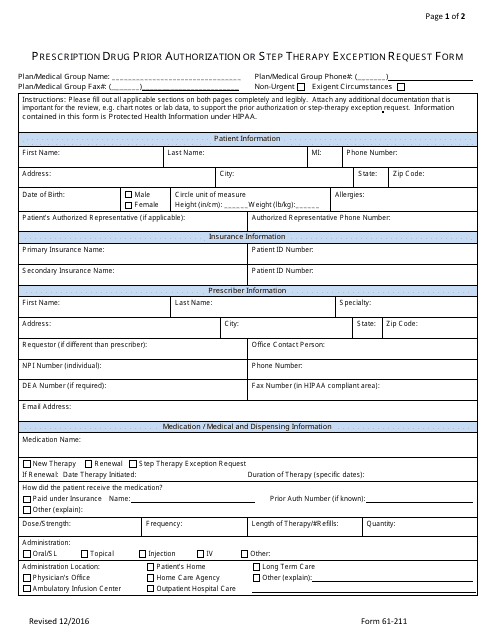
This form is used for requesting prior authorization or step therapy exception for prescription drugs through Express Scripts.
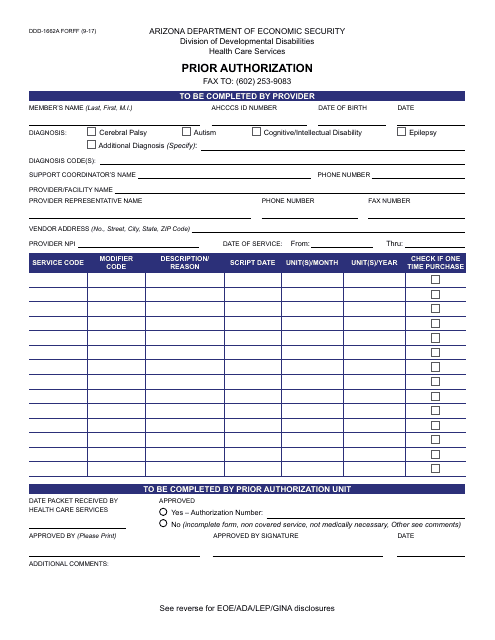
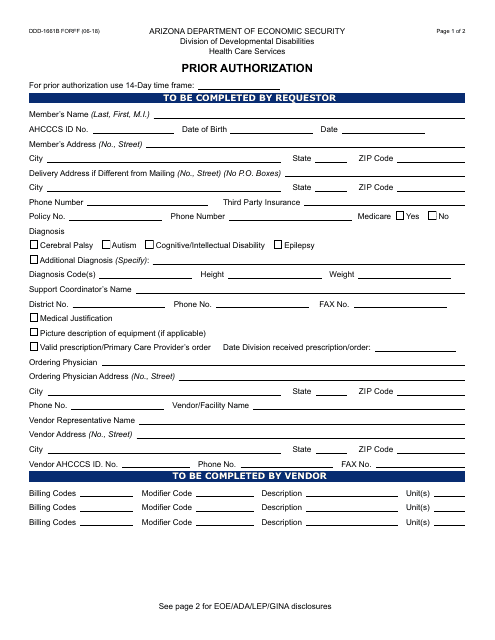
This form is used for prior authorization in Arizona. It is specifically designed for the FORFF (Family Orthodontic Redetermination/Financial Agreement) program.
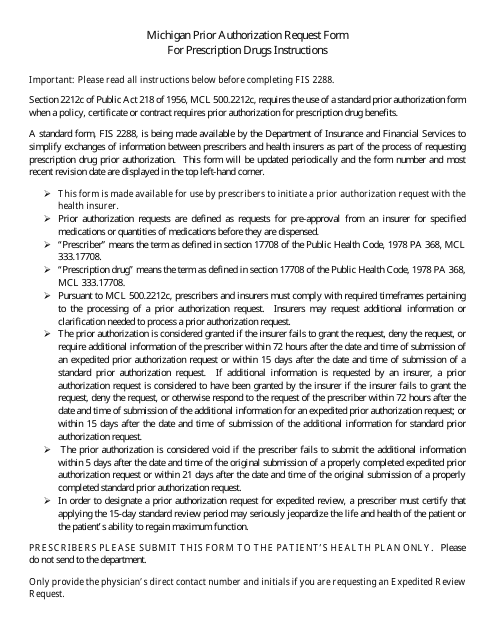
This form is used for submitting a prior authorization request for prescription drugs in the state of Michigan.
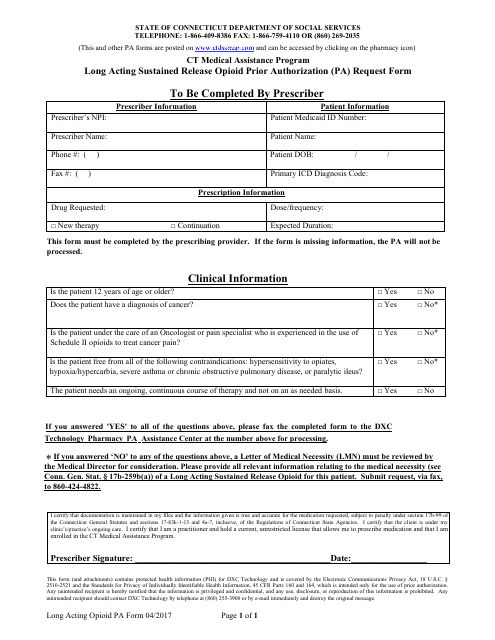
This Form is used for authorizing the use of long-acting sustained release opioids under the Connecticut Medical Assistance Program.
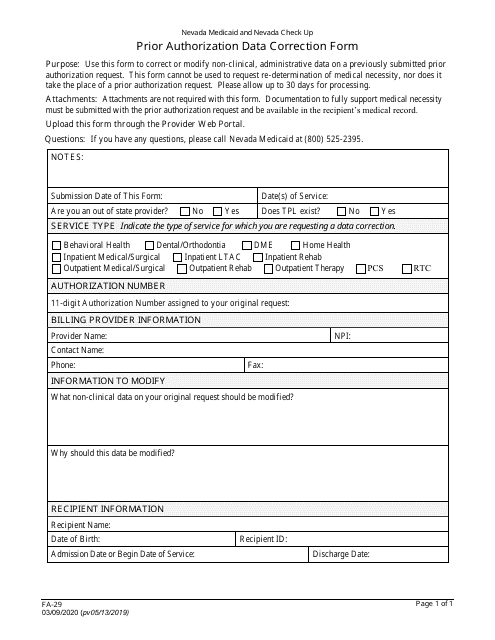
This form is used for obtaining prior authorization in Arizona for certain medical services or treatments. It helps ensure that the service or treatment is covered by the insurance provider before it is performed.
This document is a guide that provides information on Medicare Special Needs Plans (SNPs). It explains what SNPs are and the benefits they offer for individuals with specific health needs. It also highlights the eligibility criteria and enrollment process for SNPs.
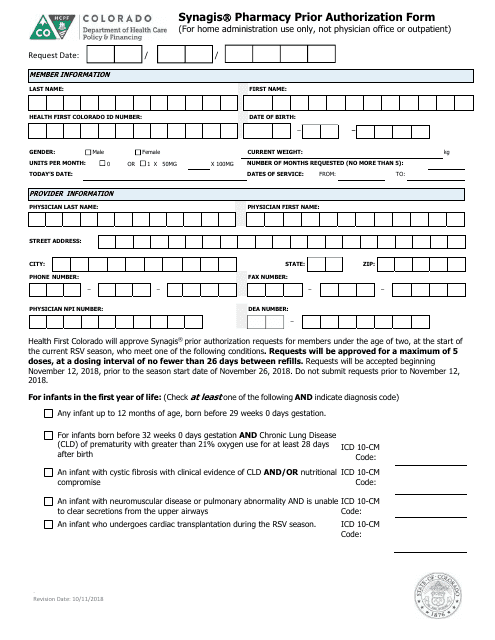
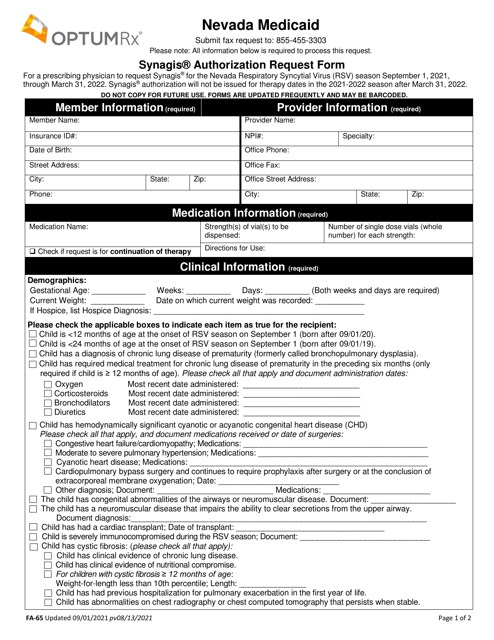
This Form is used for obtaining prior authorization from the pharmacy for Synagis medication in Colorado.
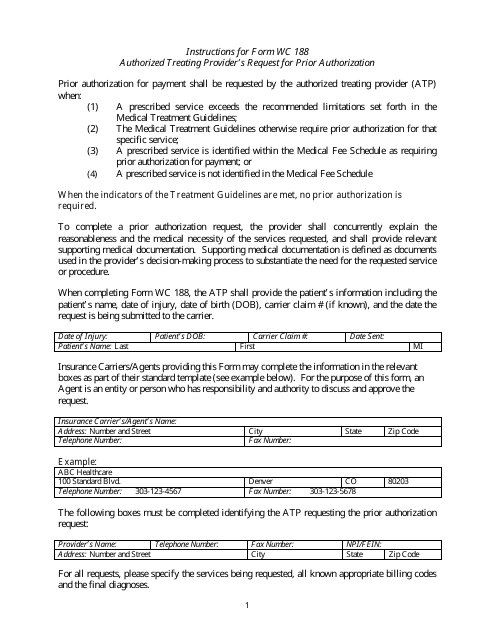
This form is used for authorized treating providers in Colorado to request prior authorization for medical treatment.
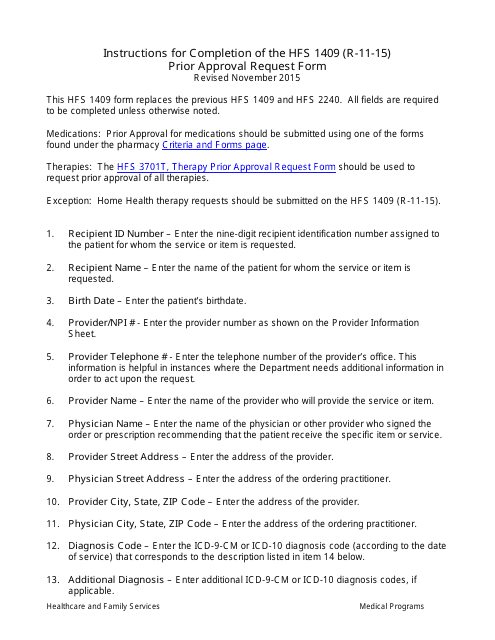
This Form is used for requesting prior approval in Illinois. It provides instructions for completing the Form HFS1409.
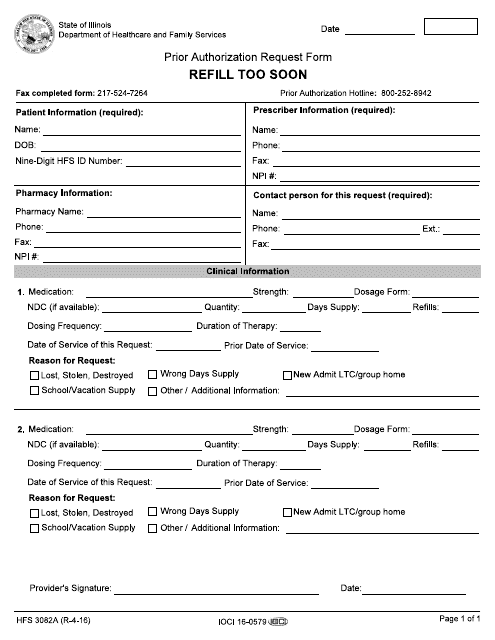
This form is used for requesting prior authorization to refill a prescription too soon in the state of Illinois.
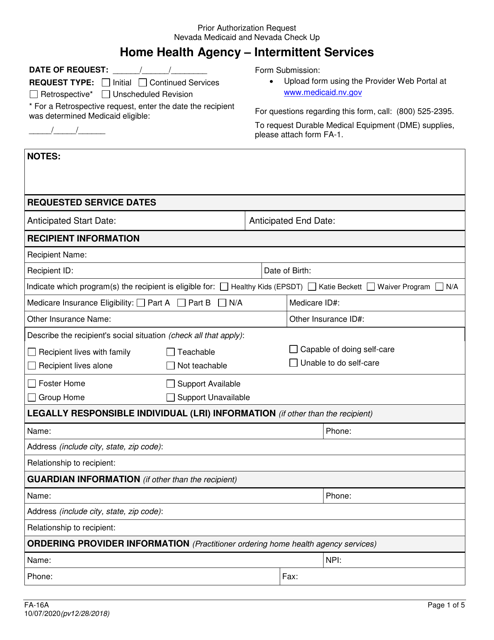
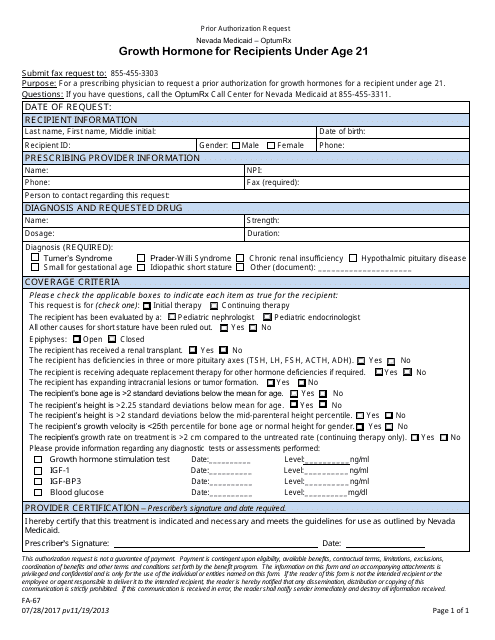
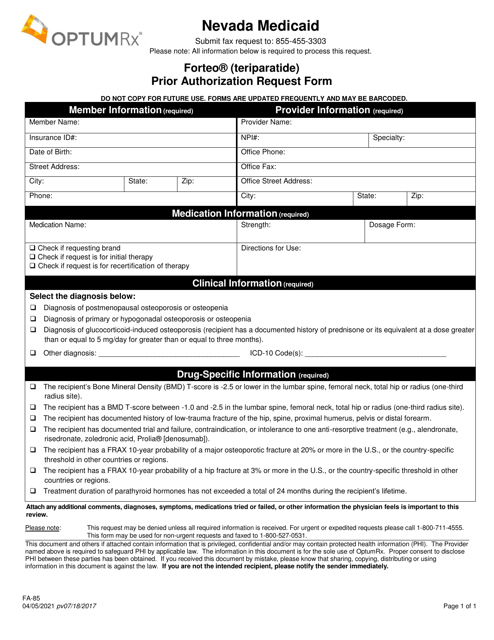
This Form is used for requesting prior authorization for growth hormone treatment for recipients under the age of 21 in Nevada.
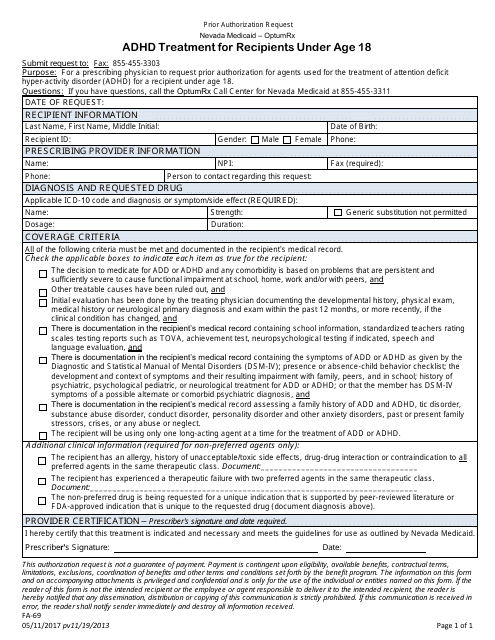
This form is used for requesting prior authorization for ADHD treatment for recipients under the age of 18 in Nevada.
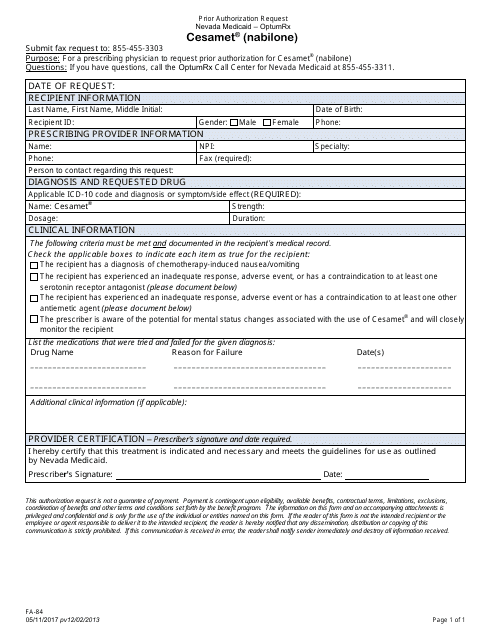
This Form is used for requesting prior authorization for the medication Cesamet (Nabilone) in the state of Nevada.
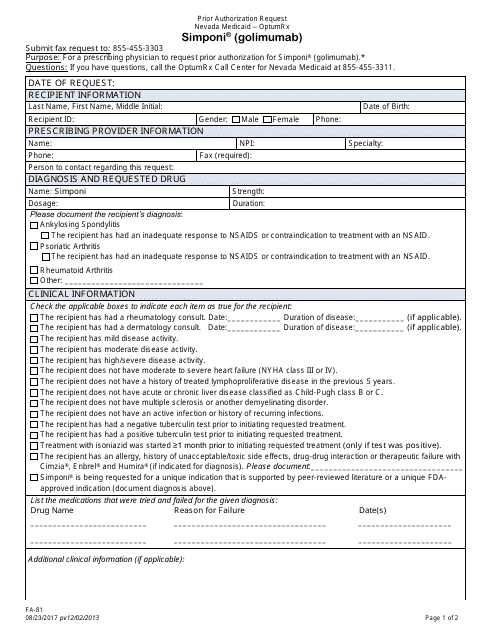
This form is used for submitting a prior authorization request for Simponi (Golimumab) medication in Nevada.