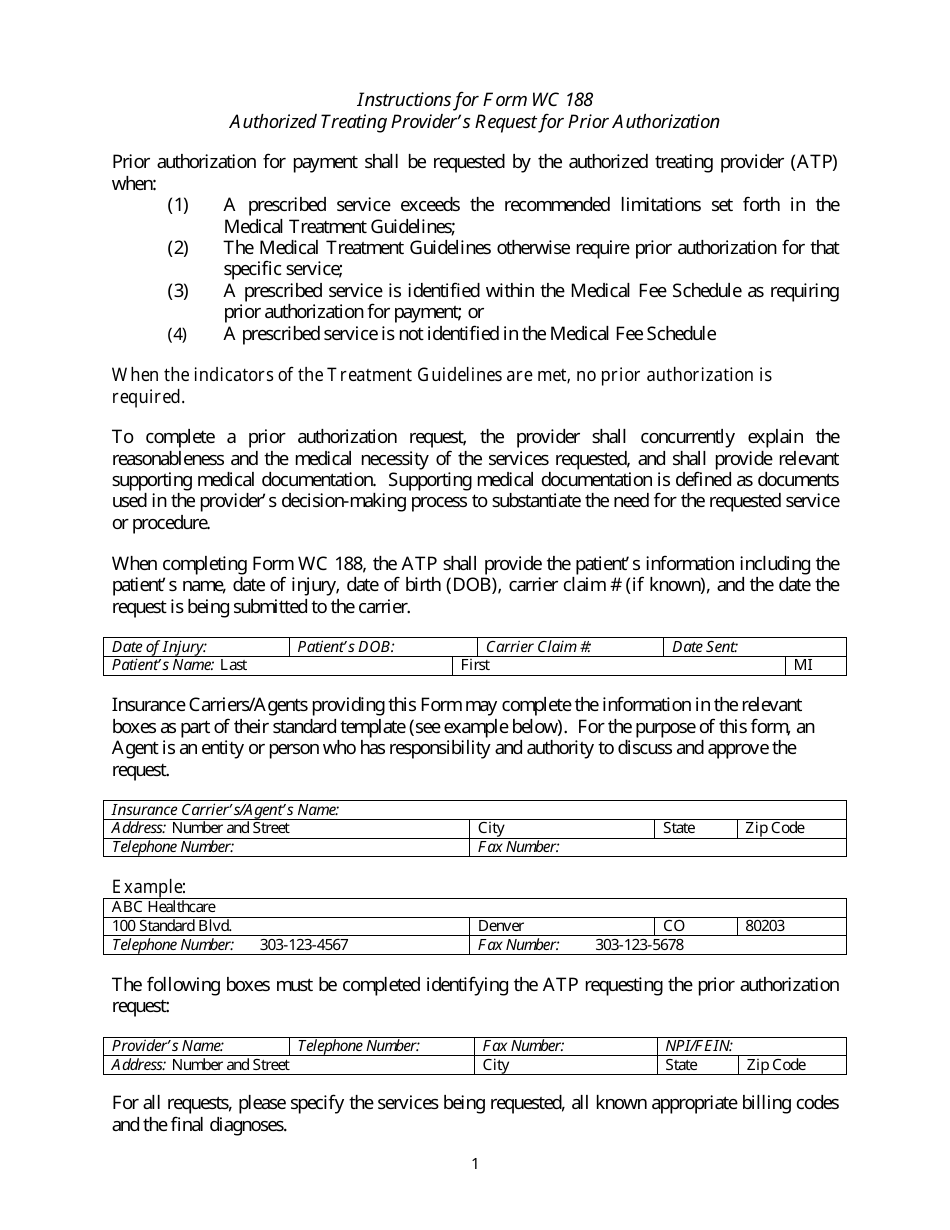
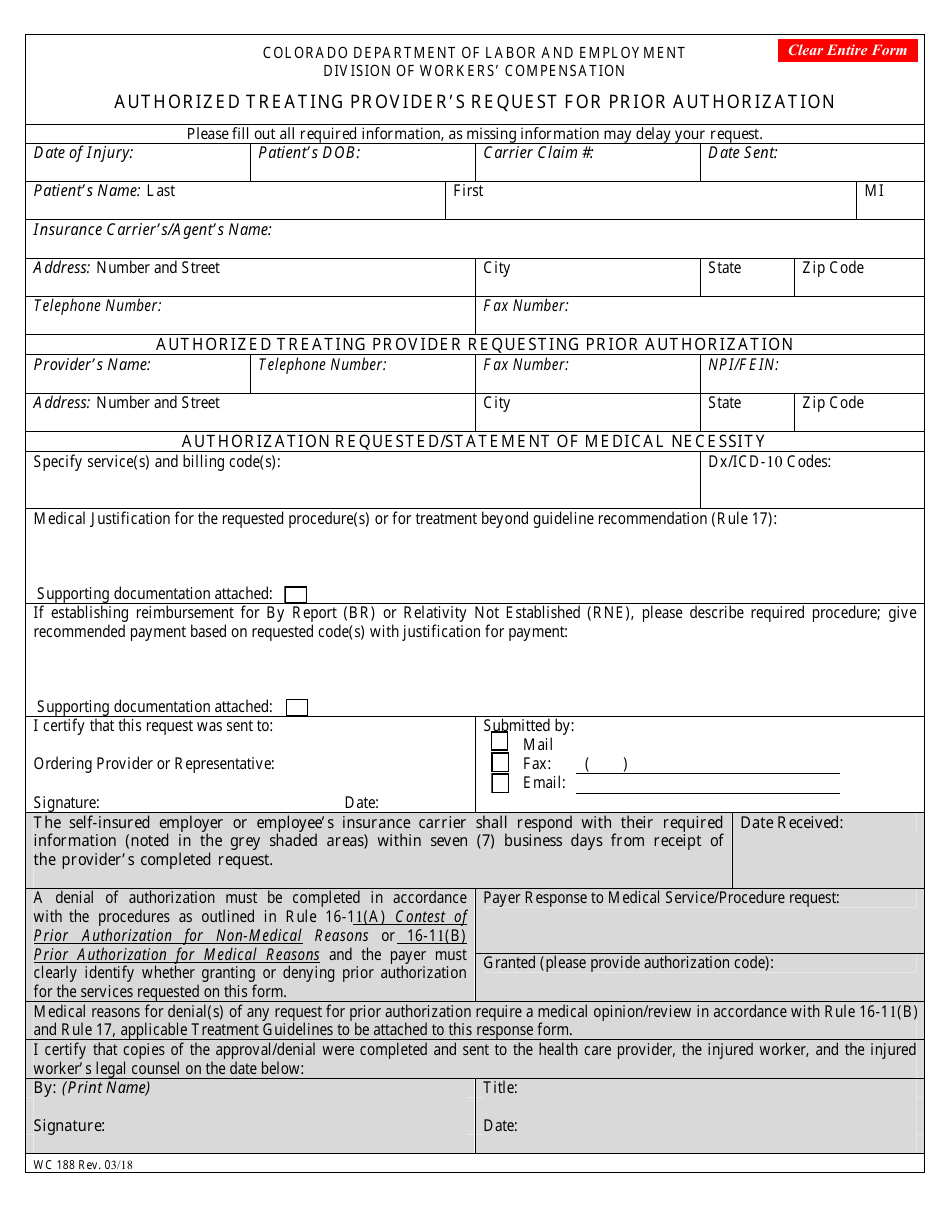
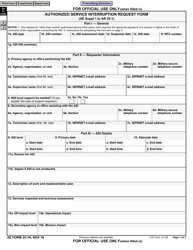
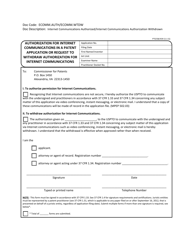
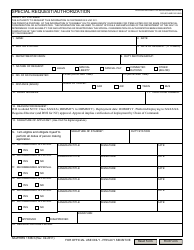
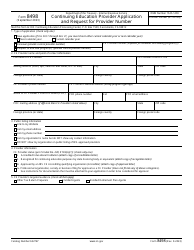
Form WC188 Authorized Treating Provider's Request for Prior Authorization - Colorado
What Is Form WC188?
This is a legal form that was released by the Colorado Department of Labor and Employment - a government authority operating within Colorado. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
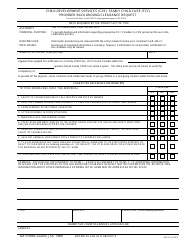
Q: What is WC188 form?
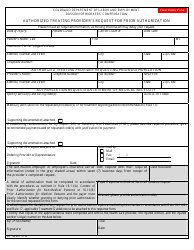
A: WC188 is a form used in Colorado for authorized treating provider's request for prior authorization in workers' compensation cases.
Q: Who can use WC188 form?
A: Authorized treating providers can use WC188 form to request prior authorization.
Q: What is the purpose of WC188 form?
A: The purpose of WC188 form is to obtain prior authorization for medical treatment or services in workers' compensation cases.
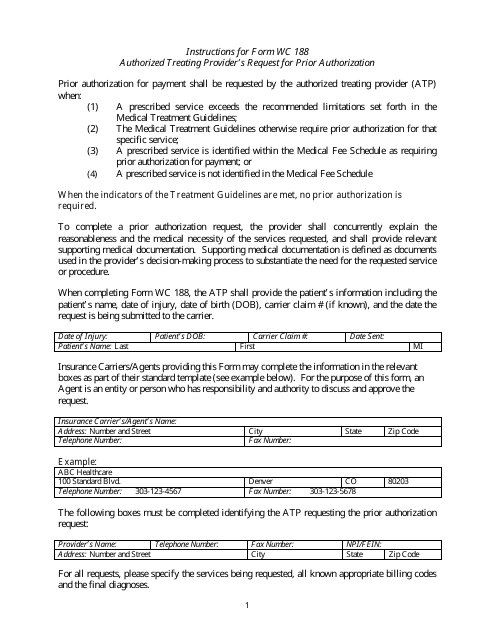
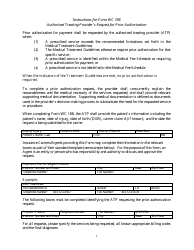
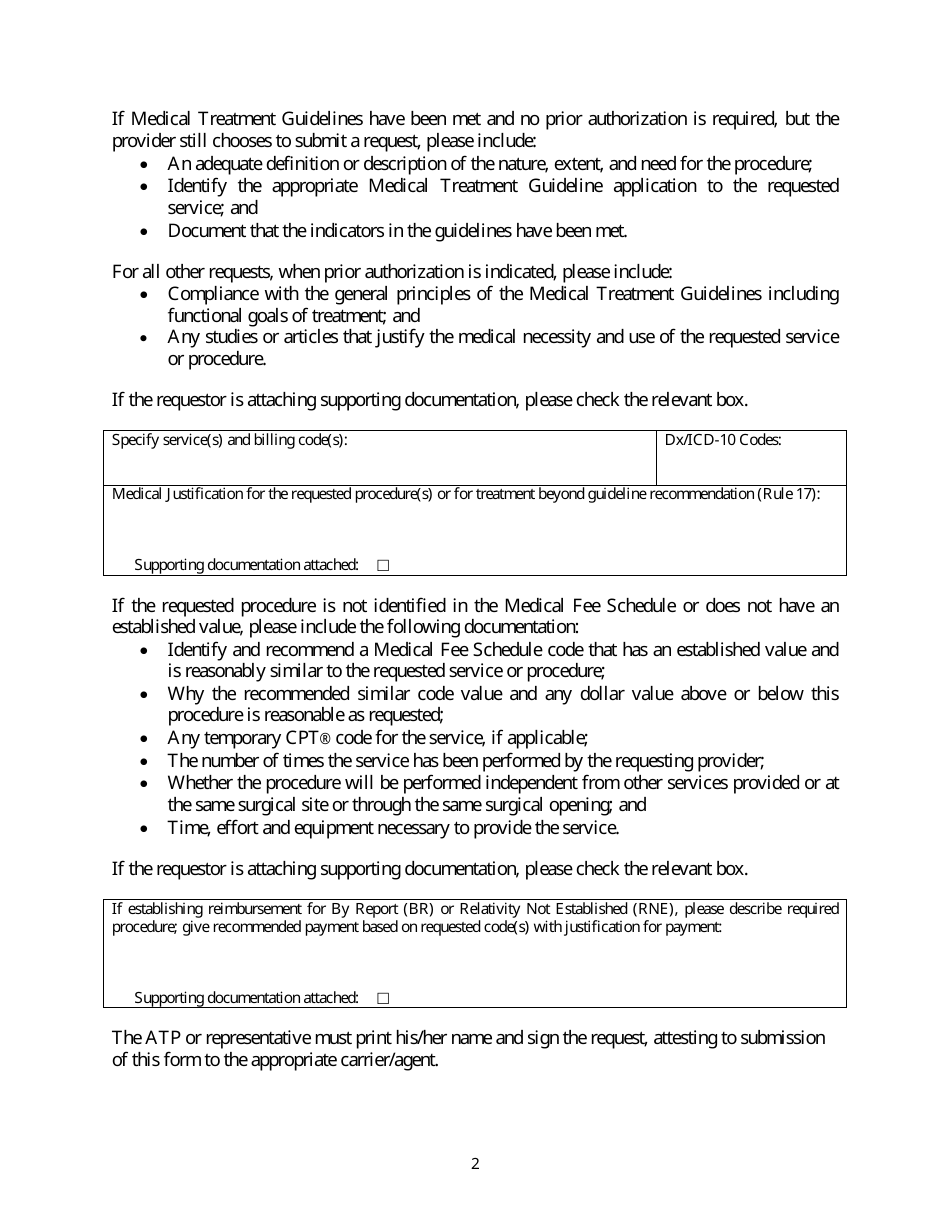
Q: What information is required on the WC188 form?
A: The WC188 form requires information about the injured worker, the requested treatment or service, and supporting documentation.
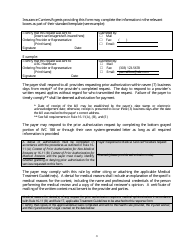
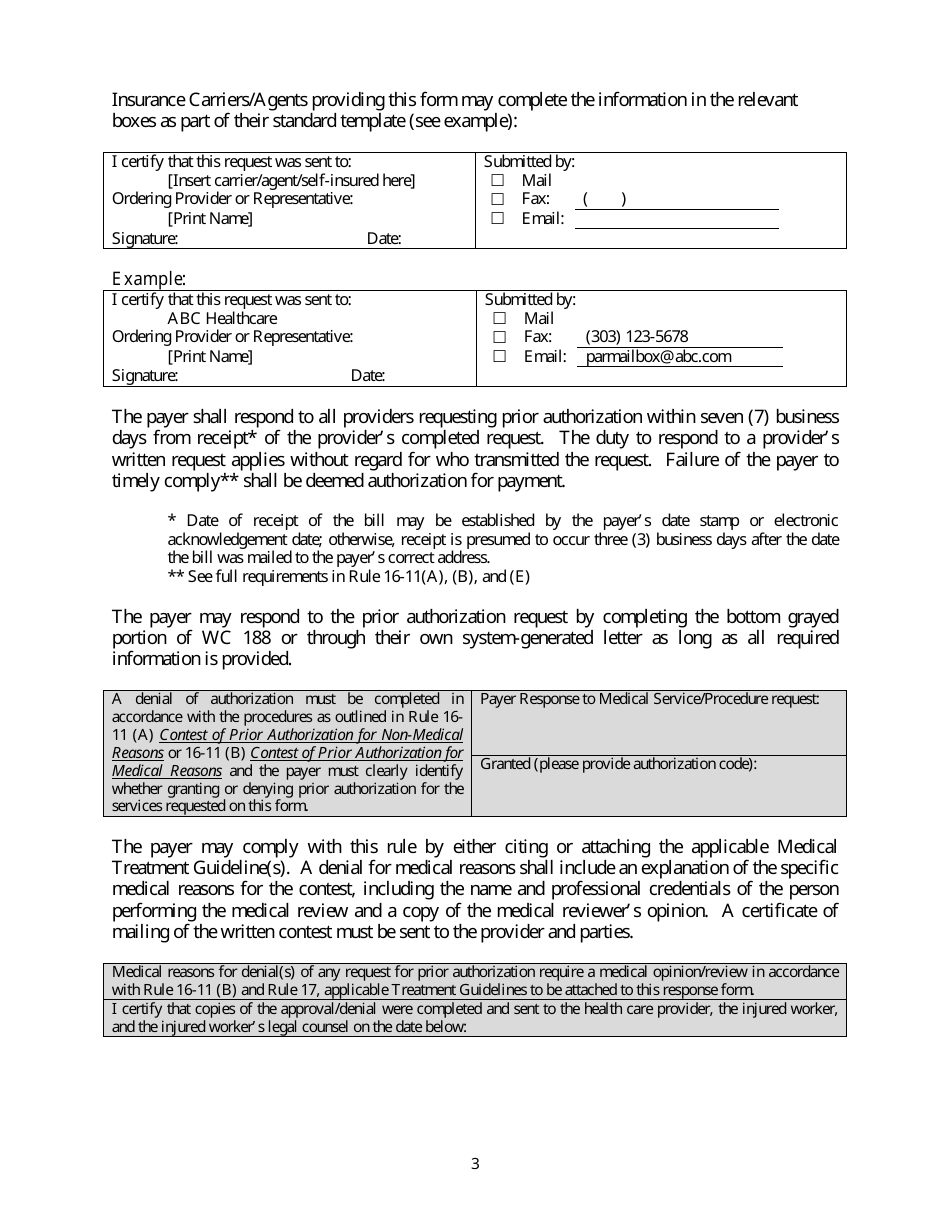
Q: How long does it take to get a response to a WC188 form?
A: The response time for a WC188 form can vary, but the Colorado Workers' Compensation rules specify that a response should be provided within 7 business days.
Form Details:
- Released on March 1, 2018;
- The latest edition provided by the Colorado Department of Labor and Employment;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form WC188 by clicking the link below or browse more documents and templates provided by the Colorado Department of Labor and Employment.