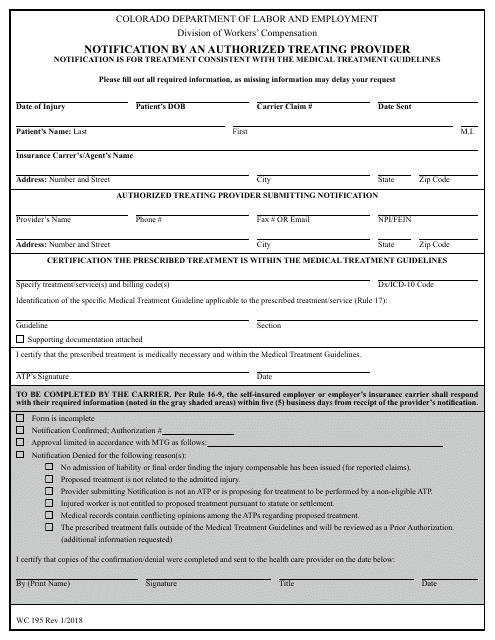
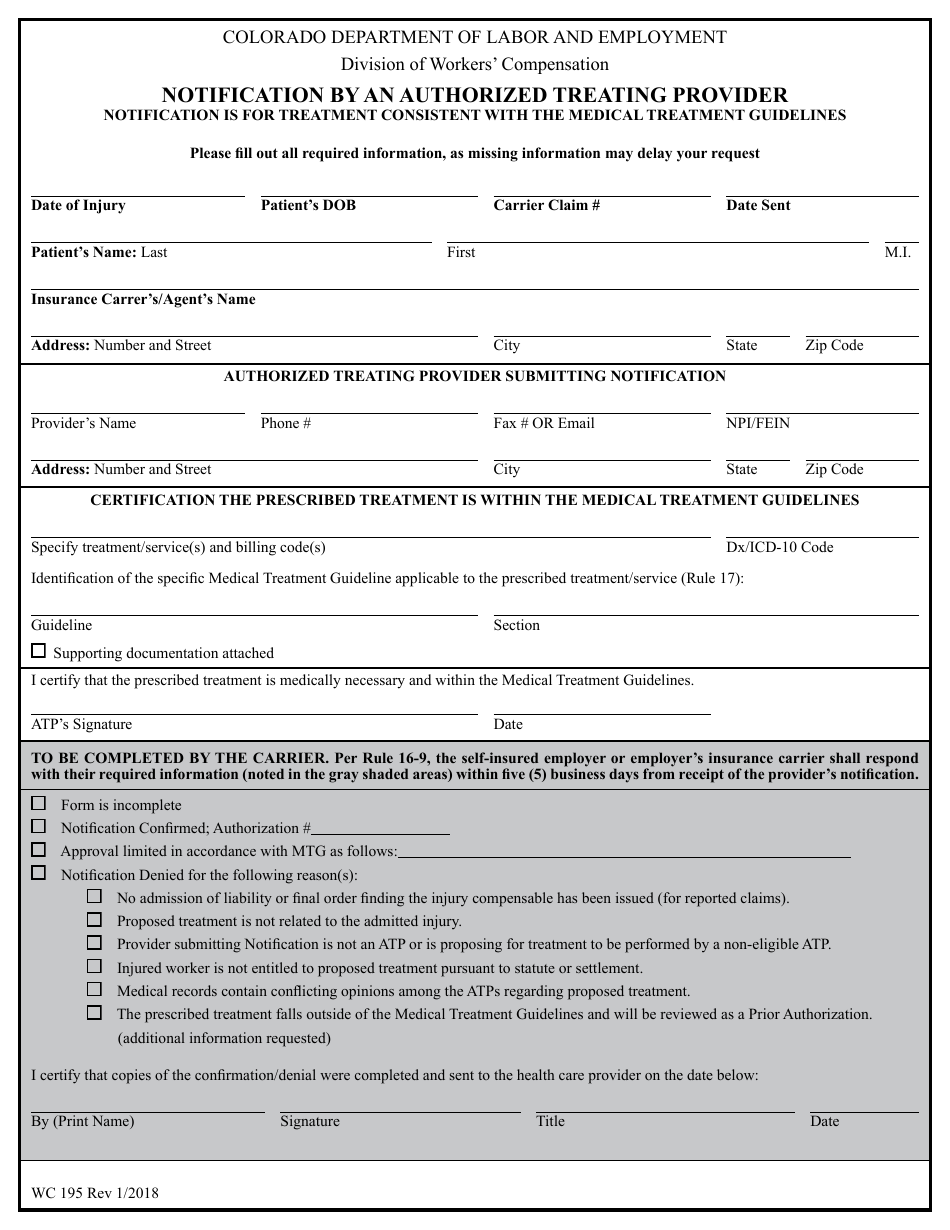
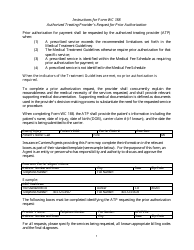
Form WC195 Notification by an Authorized Treating Provider - Colorado
What Is Form WC195?
This is a legal form that was released by the Colorado Department of Labor and Employment - a government authority operating within Colorado. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is a WC195 Notification by an Authorized Treating Provider?
A: A WC195 Notification by an Authorized Treating Provider is a form used in Colorado to notify the employer and insurance company about an injured worker's treatment.
Q: Who fills out the WC195 form?
A: The Authorized Treating Provider fills out the WC195 form.
Q: What information is included in the WC195 form?
A: The WC195 form includes information such as the injured worker's name, address, date of injury, and a description of the treatment being provided.
Q: How is the WC195 form submitted?
A: The WC195 form can be submitted electronically or by mail to the employer and insurance company.
Q: Why is the WC195 form important?
A: The WC195 form is important because it ensures that the employer and insurance company are notified about the injured worker's treatment, which can affect benefits and coverage.
Form Details:
- Released on January 1, 2018;
- The latest edition provided by the Colorado Department of Labor and Employment;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form WC195 by clicking the link below or browse more documents and templates provided by the Colorado Department of Labor and Employment.