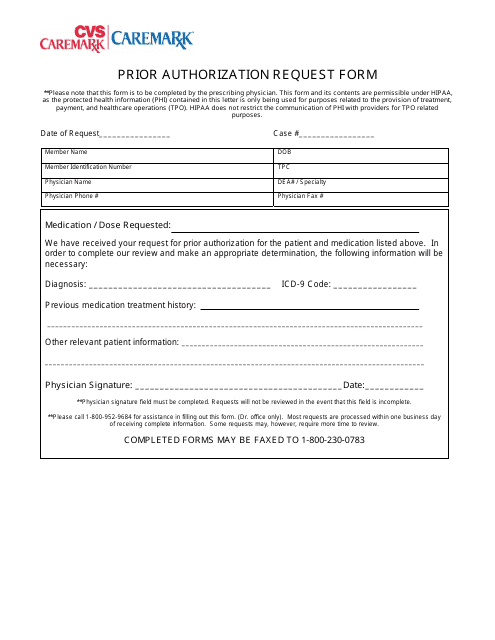
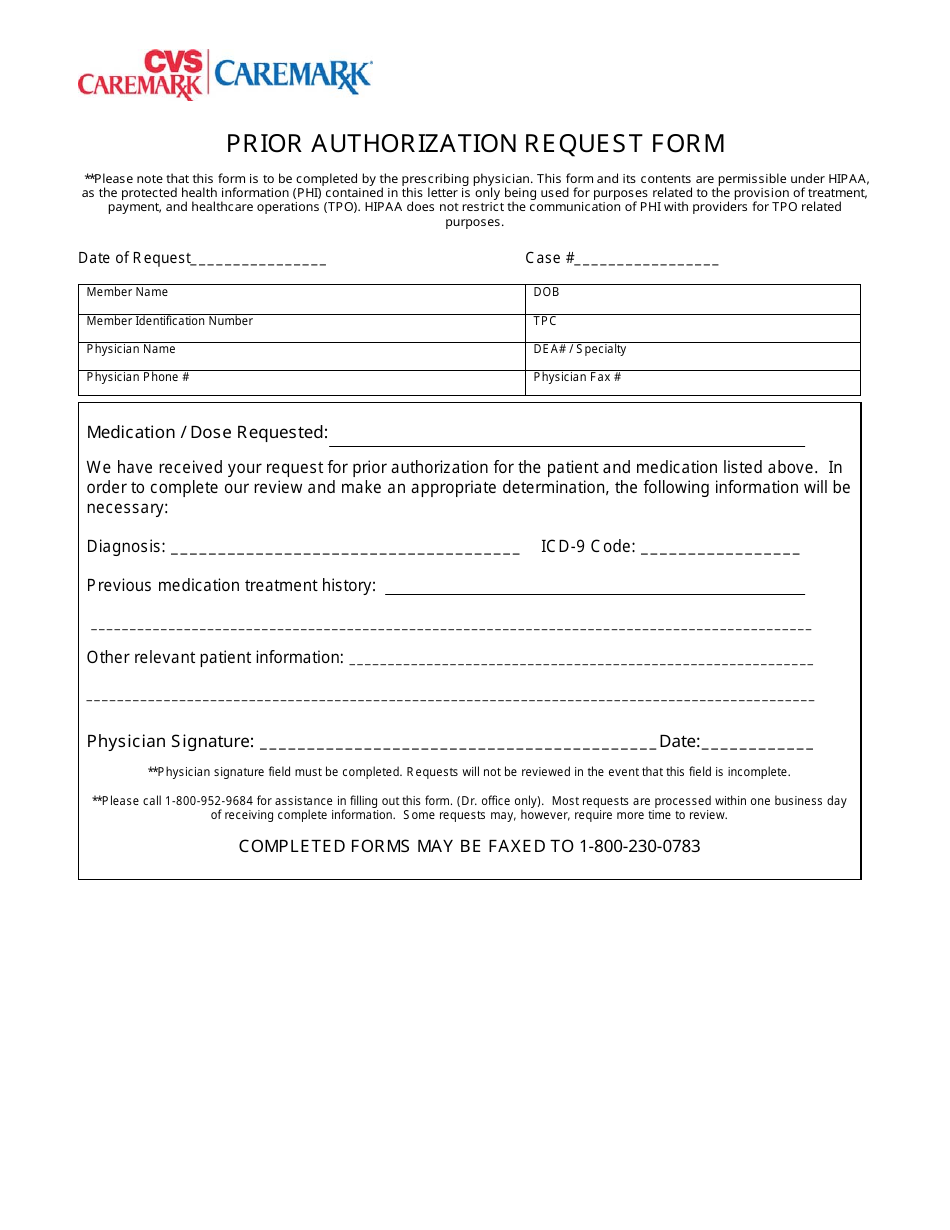
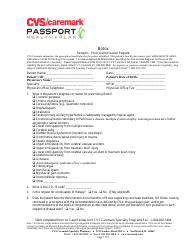
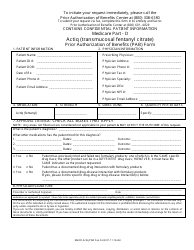
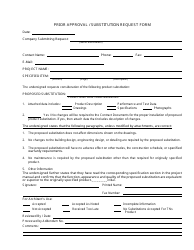
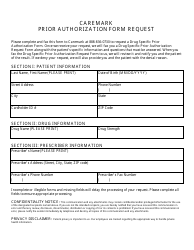
Prior Authorization Request Form - Cvs Caremark
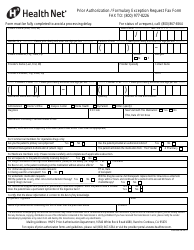
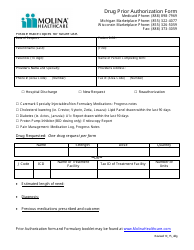
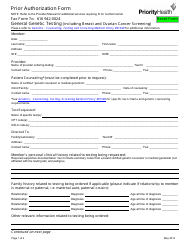
The Prior Authorization Request Form for CVS Caremark is used to request approval from your insurance provider to cover certain medications or treatments that may require prior authorization. It helps ensure that the prescribed medication or treatment meets the necessary criteria for coverage.
Yes, CVS Caremark would typically file the Prior Authorization Request form.
FAQ
Q: What is a Prior Authorization Request Form?
A: A Prior Authorization Request Form is a form used to request approval from CVS Caremark for a medication or treatment that may require additional review or documentation.
Q: When do I need to use a Prior Authorization Request Form?
A: You need to use a Prior Authorization Request Form when your medication or treatment requires prior authorization from CVS Caremark.
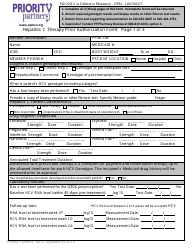
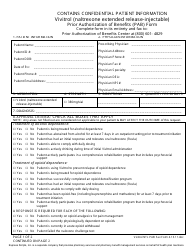
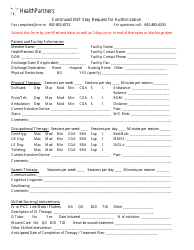
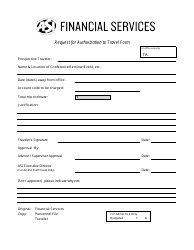
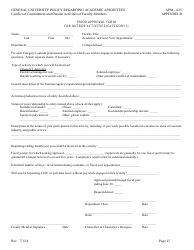
Q: What information is required on a Prior Authorization Request Form?
A: A Prior Authorization Request Form typically requires information such as the patient's personal information, healthcare provider's information, details of the medication or treatment, and supporting documentation.
Q: How long does it take for CVS Caremark to review a Prior Authorization Request?
A: The review process for a Prior Authorization Request can vary, but CVS Caremark typically responds within a certain timeframe, such as 72 hours.
Q: What happens after CVS Caremark reviews a Prior Authorization Request?
A: After reviewing a Prior Authorization Request, CVS Caremark will notify the patient and healthcare provider of their decision, which could be approval, denial, or a request for additional information.