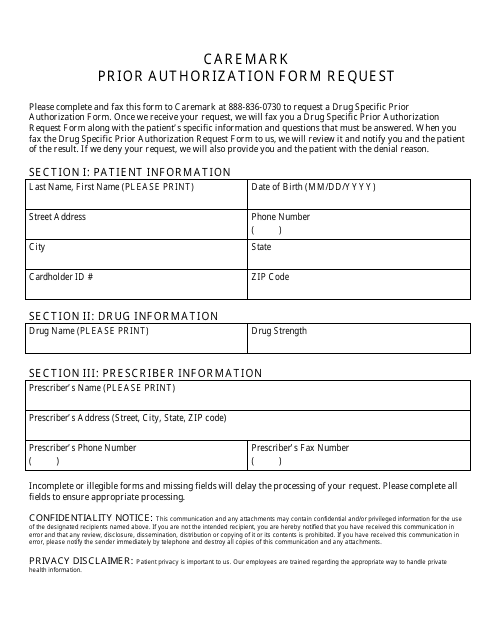
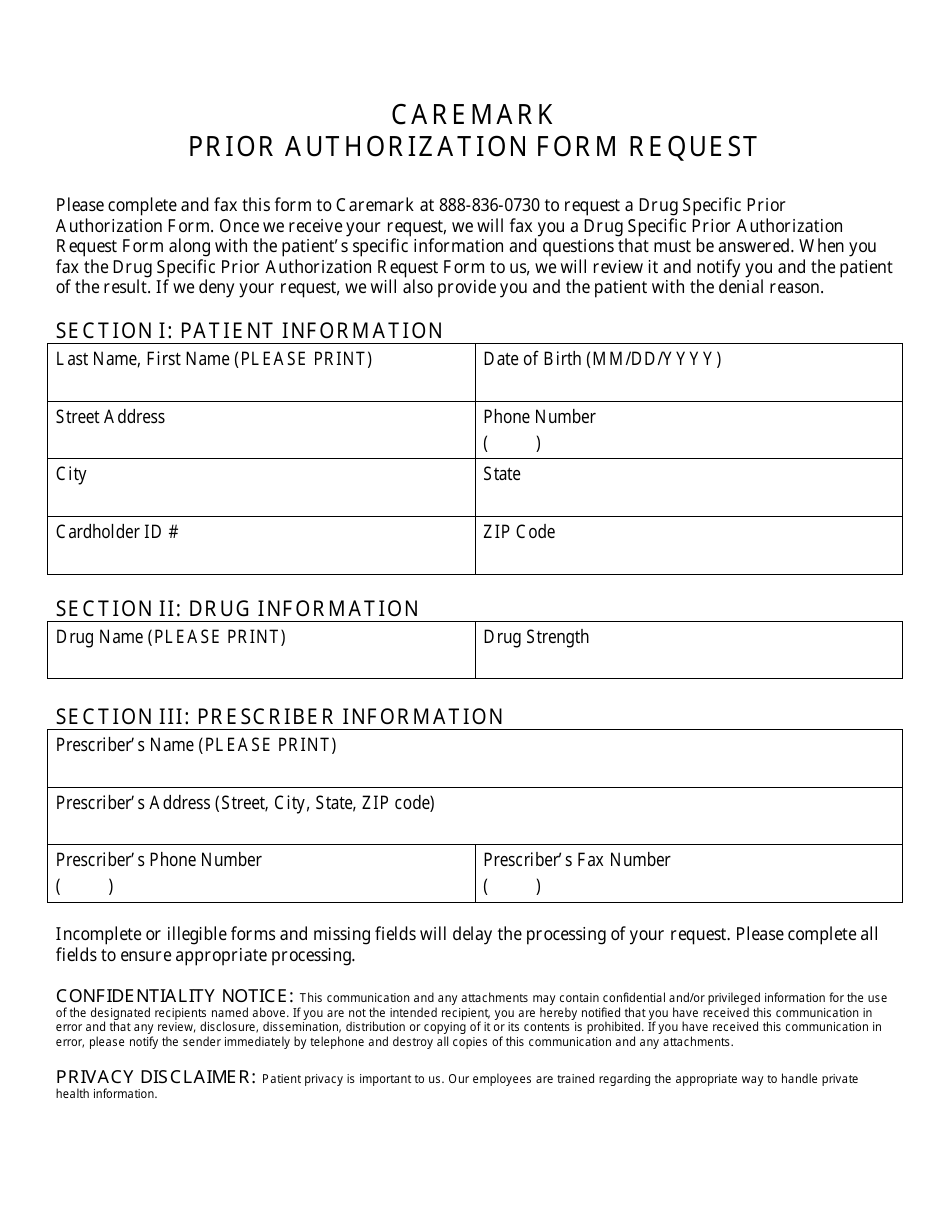
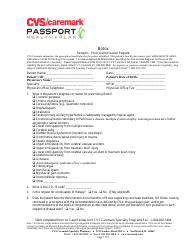
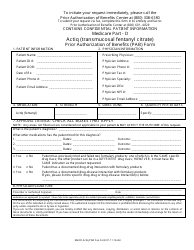
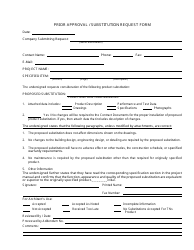
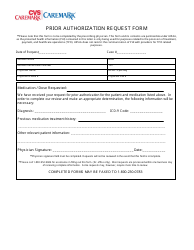
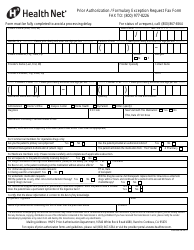
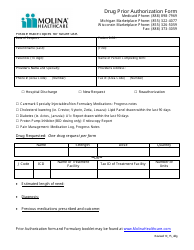
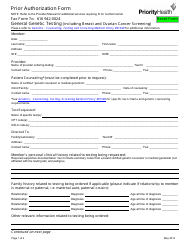
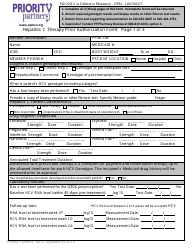
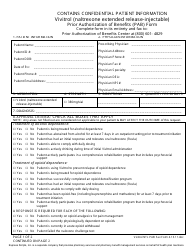
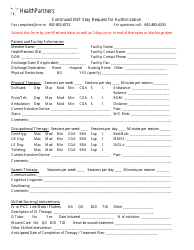
Prior Authorization Form Request - Cvs Caremark
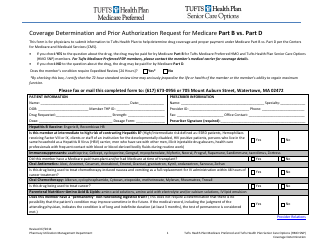
The Prior Authorization Form Request - CVS Caremark is used to request approval from the insurance company for certain prescription medications or treatments. It's a process to ensure that the medication or treatment is medically necessary and covered by the insurance plan.
Typically, it is the healthcare provider or the prescribing doctor who files the prior authorization form request with CVS Caremark.
FAQ
Q: What is a Prior Authorization Form?
A: A Prior Authorization Form is a document that is required for certain prescriptions to be covered by insurance.
Q: Why do I need a Prior Authorization Form?
A: You need a Prior Authorization Form for prescriptions that require prior approval from your insurance company before they will cover the cost.
Q: How do I obtain a Prior Authorization Form?
A: You can obtain a Prior Authorization Form from your doctor or pharmacy.
Q: What information is needed on a Prior Authorization Form?
A: A Prior Authorization Form typically requires information such as your personal details, the medication being prescribed, and supporting medical documentation.
Q: How long does it take to process a Prior Authorization Form?
A: The processing time for a Prior Authorization Form can vary, but it generally takes a few business days.
Q: What happens if my Prior Authorization Form is denied?
A: If your Prior Authorization Form is denied, you may need to discuss alternative medication options with your doctor or appeal the decision with your insurance company.
Q: Do I need a Prior Authorization Form for all medications?
A: Not all medications require a Prior Authorization Form. It depends on your insurance coverage and the specific medication being prescribed.
Q: Can my doctor request a Prior Authorization Form on my behalf?
A: Yes, your doctor can request a Prior Authorization Form on your behalf and submit it to your insurance company or pharmacy.
Q: Is a Prior Authorization Form the same as a prescription?
A: No, a Prior Authorization Form is a separate document that is required in addition to a prescription in order for the medication to be covered by insurance.