Cvs Caremark Prior Authorization Form Templates
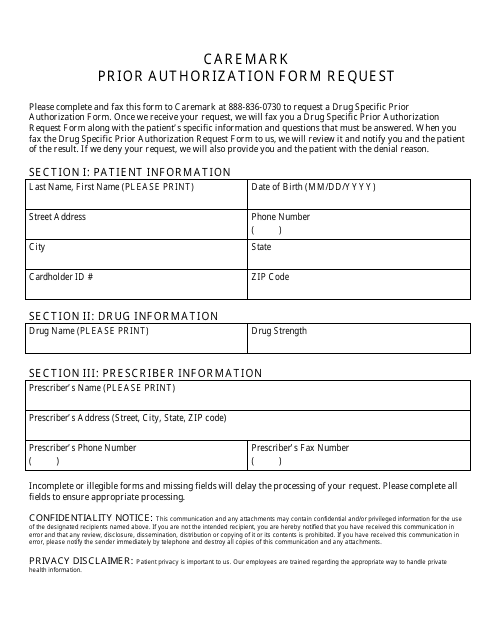
The CVS Caremark Prior Authorization Form is used to request approval from CVS Caremark, a pharmacy benefits manager, for the coverage of certain medications. Prior authorization is typically required for specific medications that may have limitations or require additional clinical information before they can be covered by insurance. This form helps to gather necessary information and documentation to support the request for coverage.
Documents:
1
This Form is used for requesting prior authorization for medications through Cvs Caremark.