Prior Authorization Request Form Templates
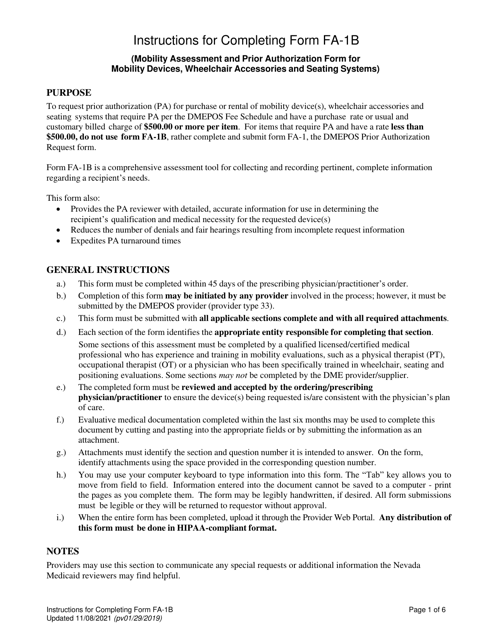
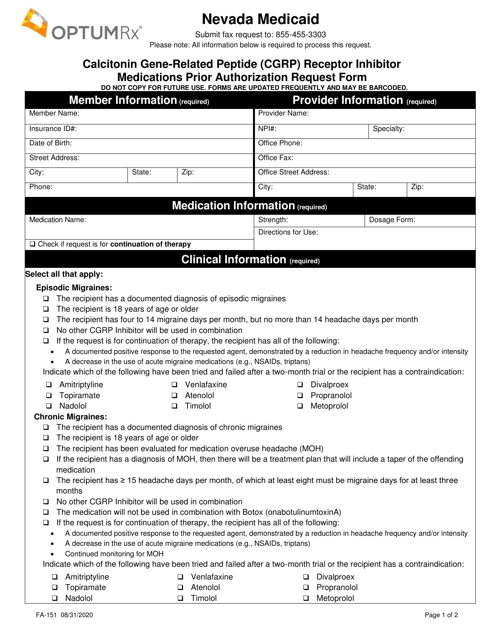
Prior Authorization Request Forms are used to request approval from a healthcare insurance provider for coverage of a specific medication or medical service. It is typically required when a medication or service is not included in the insurance plan's formulary or when certain criteria need to be met before coverage is granted. The form is used to provide detailed information about the patient, the prescribed medication or service, and the justification for the request.
Documents:
132
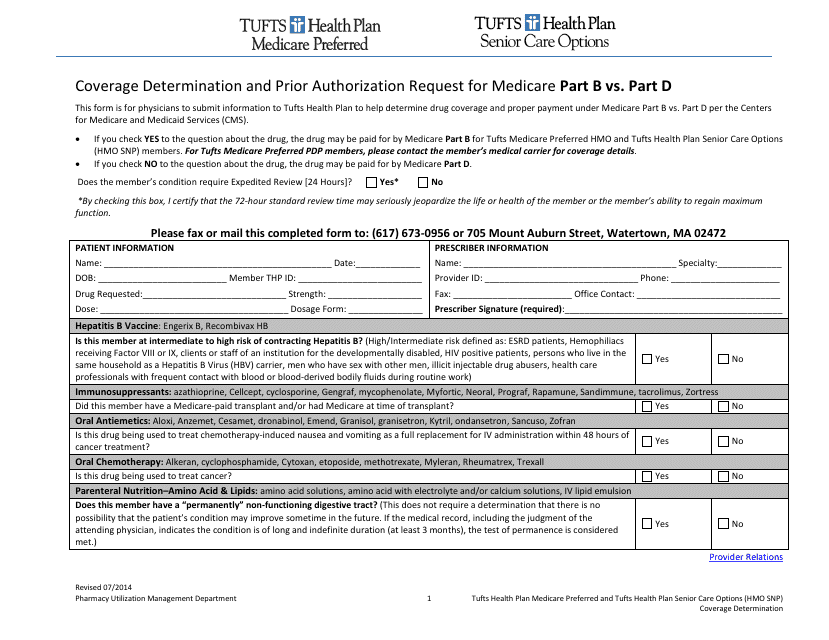
This Form is used for submitting a coverage determination request or prior authorization request for Medicare Part B or Part D benefits under Tufts insurance.
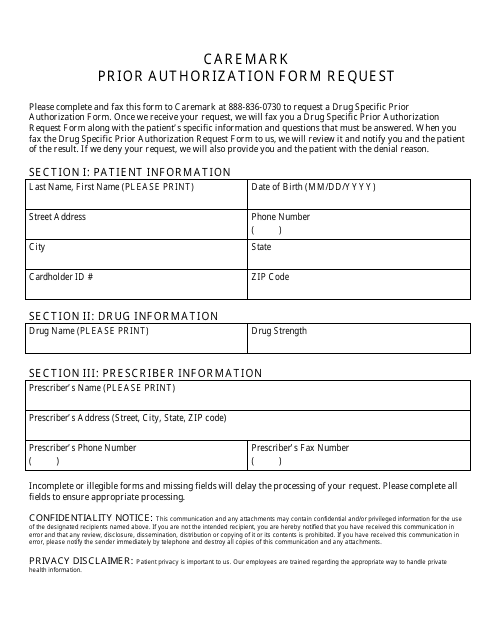
This Form is used for requesting prior authorization for medications through Cvs Caremark.
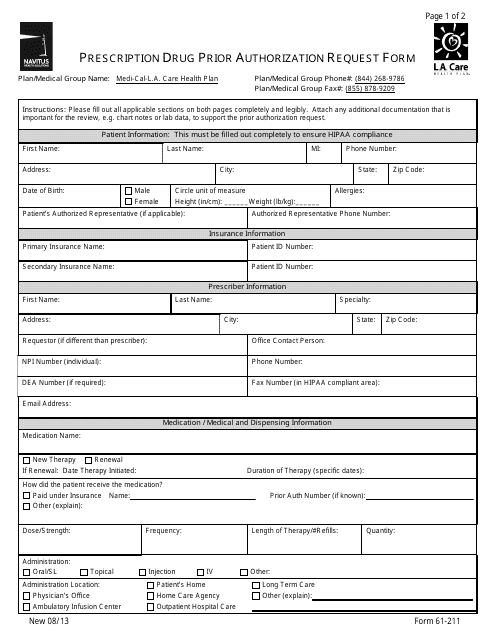
This form is used for requesting prior authorization for prescription drugs from L.A. Care Health Plan.
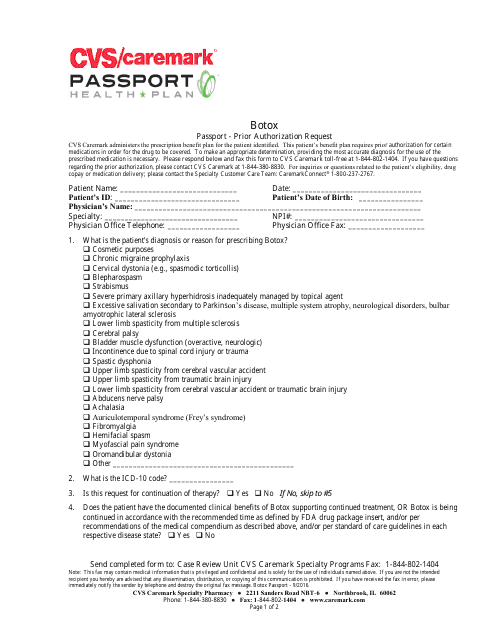
This form is used for requesting prior authorization for Botox treatment through CVS Caremark.
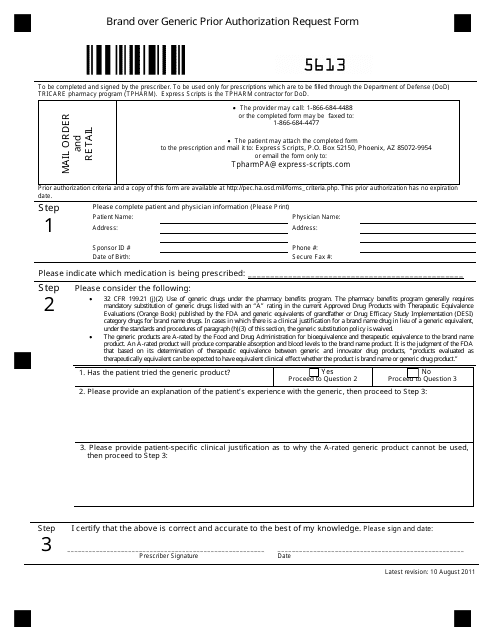
This document is used for requesting prior authorization for brand-name medications instead of generic alternatives.
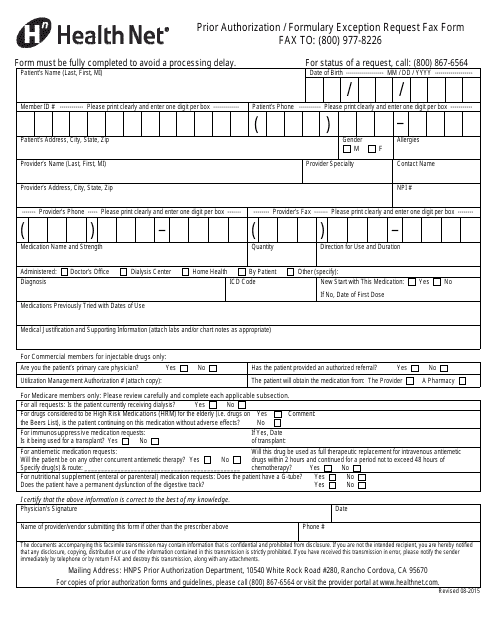
This form is used for requesting prior authorization or formulary exception from Health Net through fax.
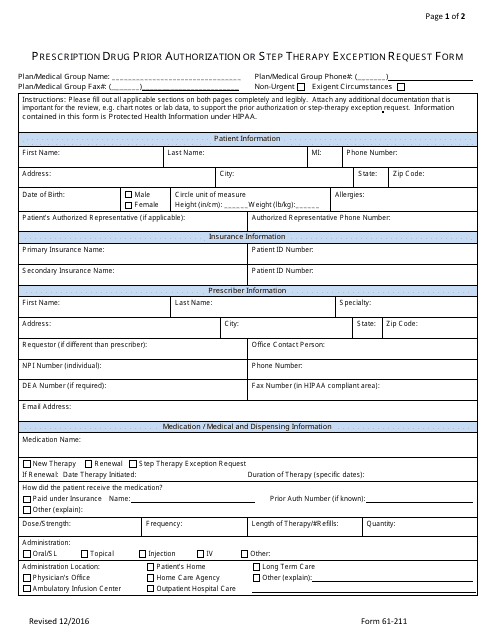
This form is used for requesting prior authorization or step therapy exception for prescription drugs through Express Scripts.
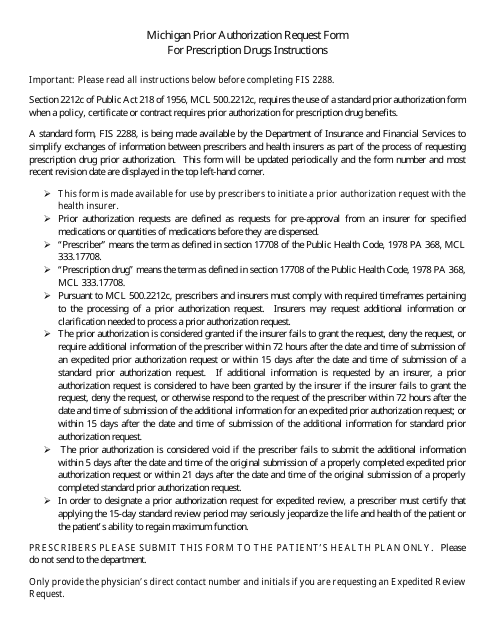
This form is used for submitting a prior authorization request for prescription drugs in the state of Michigan.
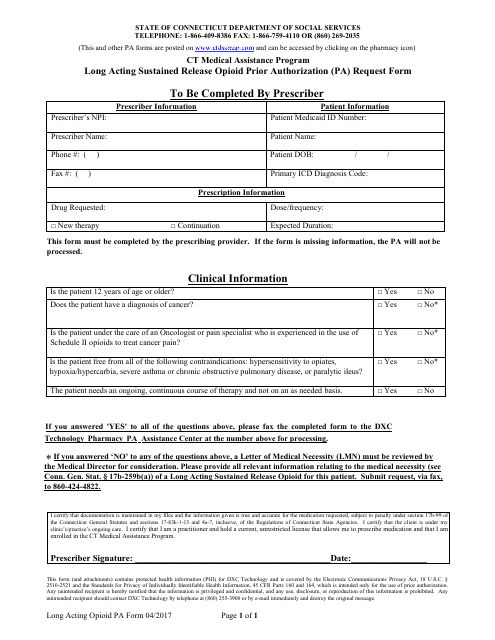
This Form is used for authorizing the use of long-acting sustained release opioids under the Connecticut Medical Assistance Program.
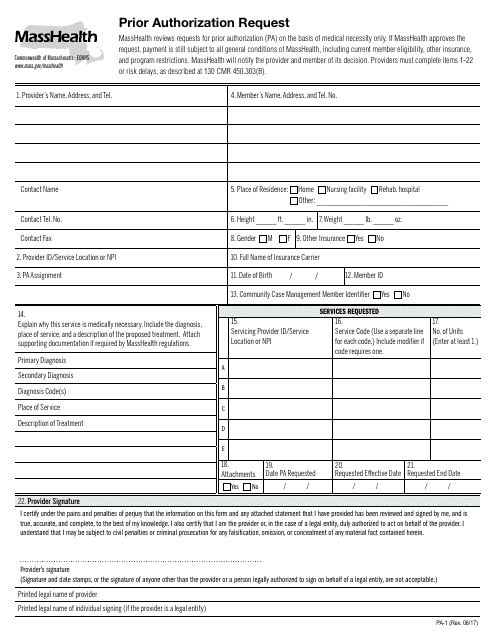
This form is used for requesting prior authorization in Massachusetts.
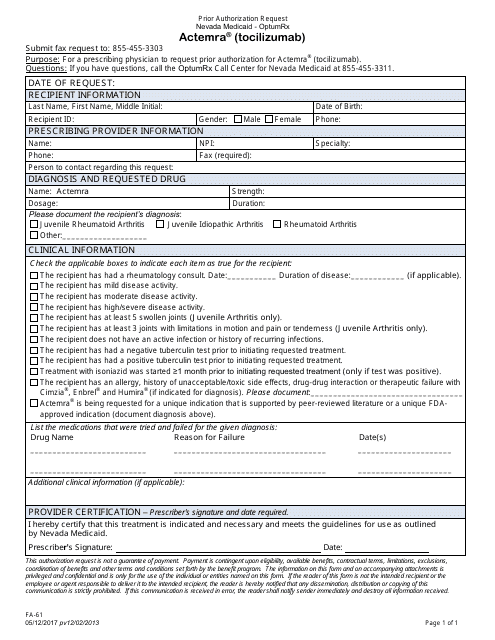
This Form is used for requesting prior authorization for the medication Actemra (Tocilizumab) in the state of Nevada.
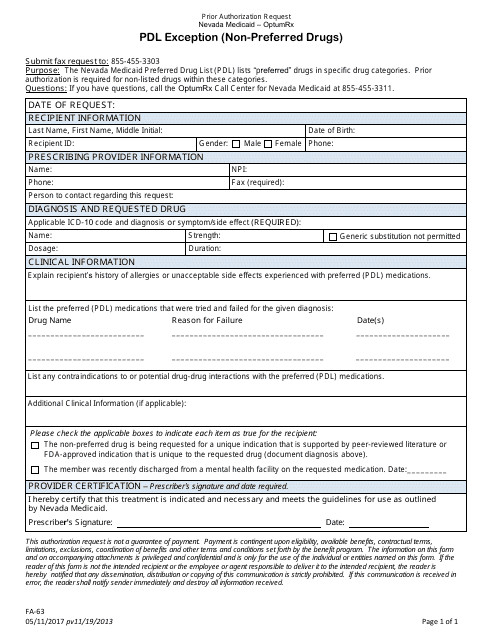
This form is used for requesting prior authorization for non-preferred drugs in Nevada.
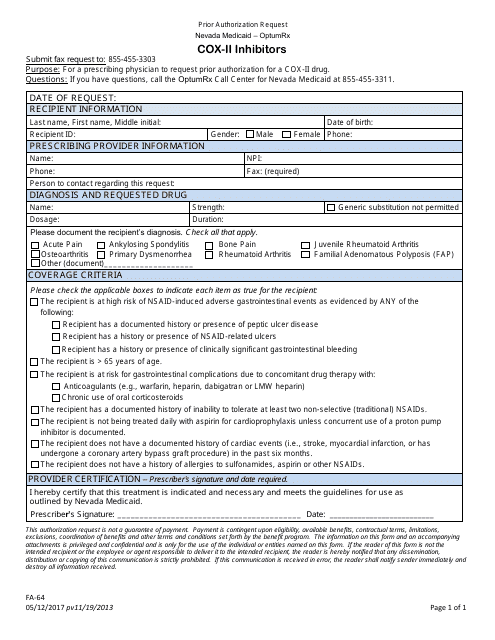
This Form is used for requesting prior authorization for Cox-II inhibitors in the state of Nevada.
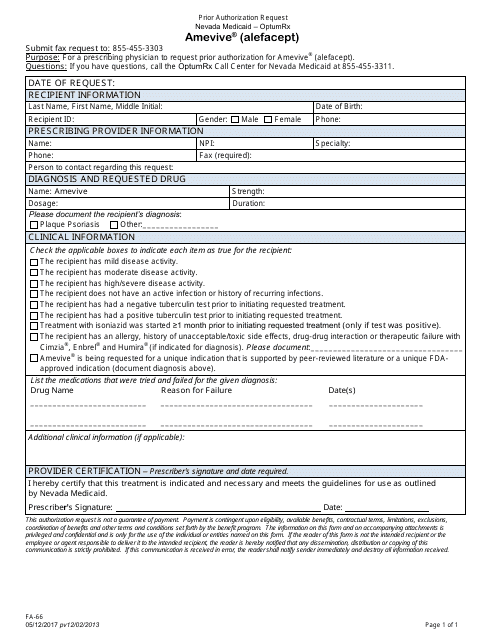
This Form is used for requesting prior authorization for the medication Amevive (Alefacept) in the state of Nevada.
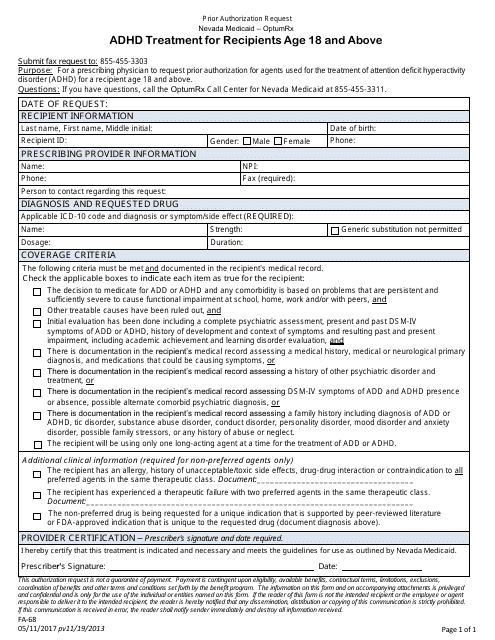
This form is used for requesting prior authorization for ADHD treatment for recipients aged 18 and above in Nevada.
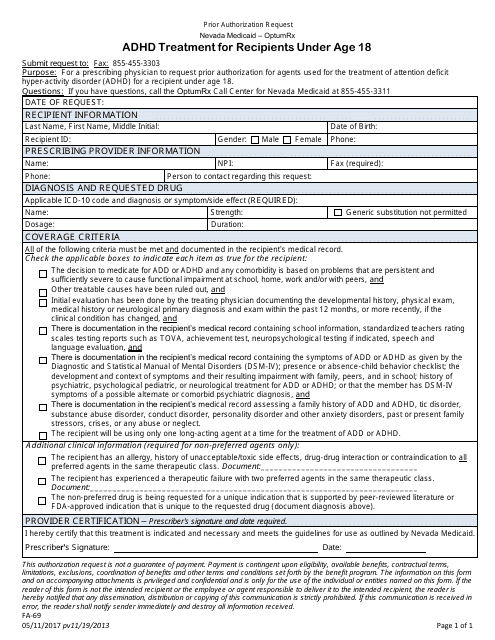
This form is used for requesting prior authorization for ADHD treatment for recipients under the age of 18 in Nevada.
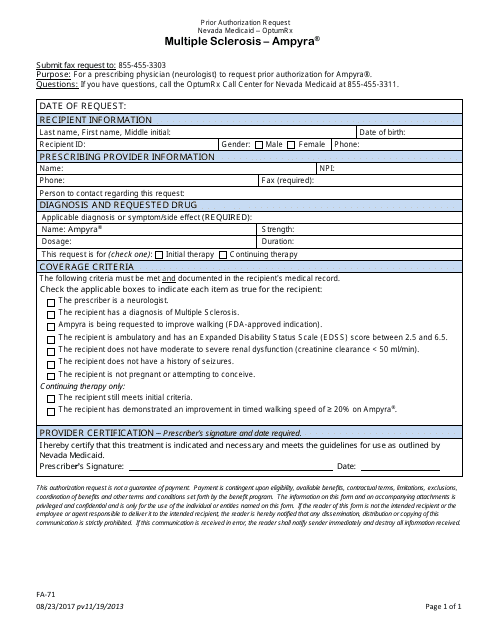
This Form is used for requesting prior authorization for the medication Ampyra in Nevada for individuals with Multiple Sclerosis.
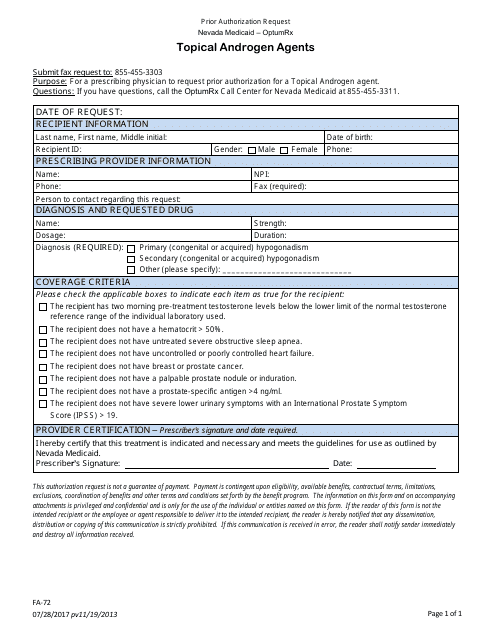
This form is used for requesting prior authorization for the use of topical androgen agents in the state of Nevada.
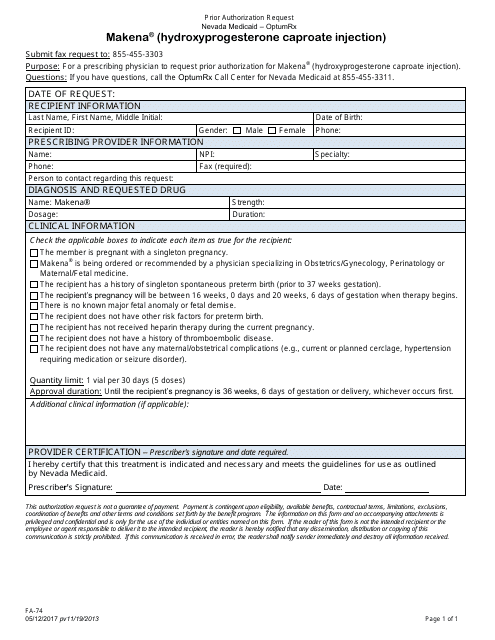
This Form is used for requesting prior authorization for Makena (Hydroxyprogesterone Caproate Injection) in Nevada.
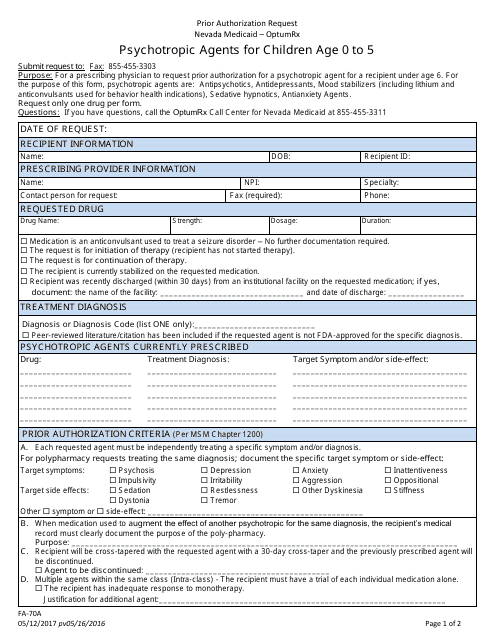
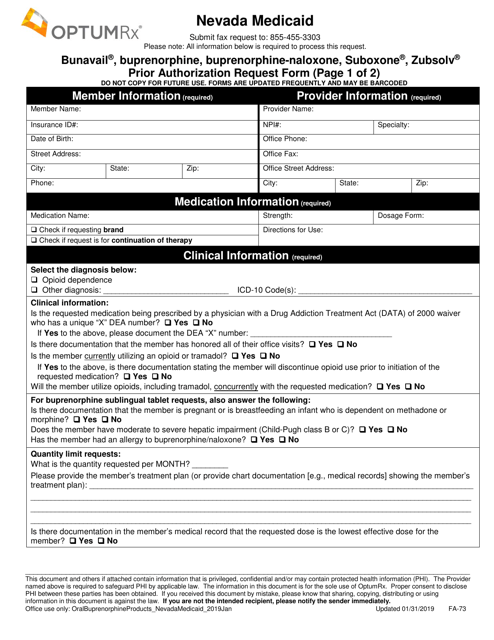
This Form is used for requesting prior authorization for psychotropic agents for children aged 0 to 5 in Nevada.
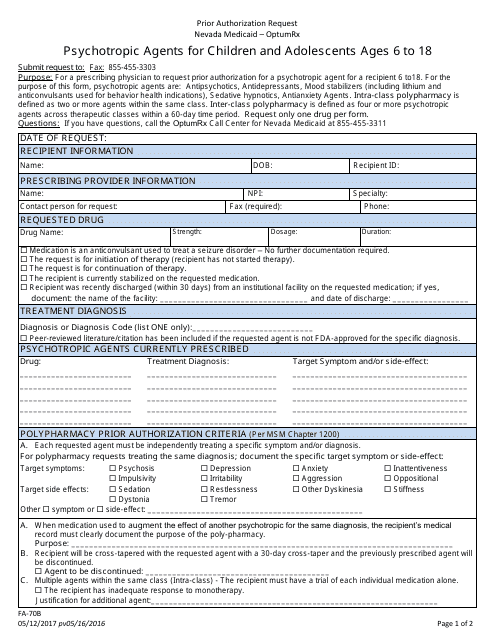
This Form is used for requesting prior authorization for psychotropic agents for children and adolescents between the ages of 6 to 18 in Nevada.
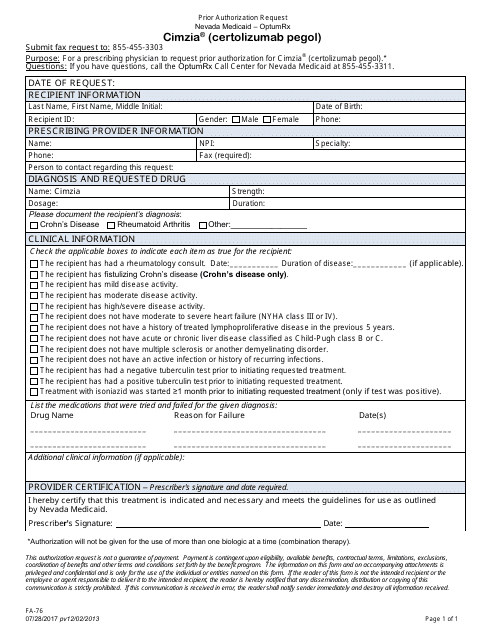
This Form is used for requesting prior authorization for the medication Cimzia (Certolizumab Pegol) in the state of Nevada.
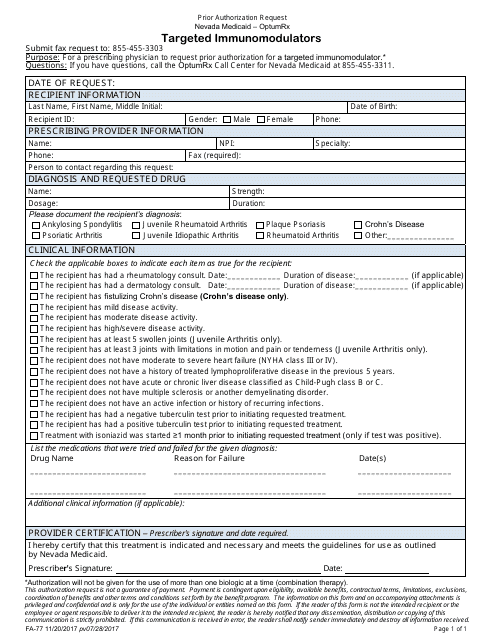
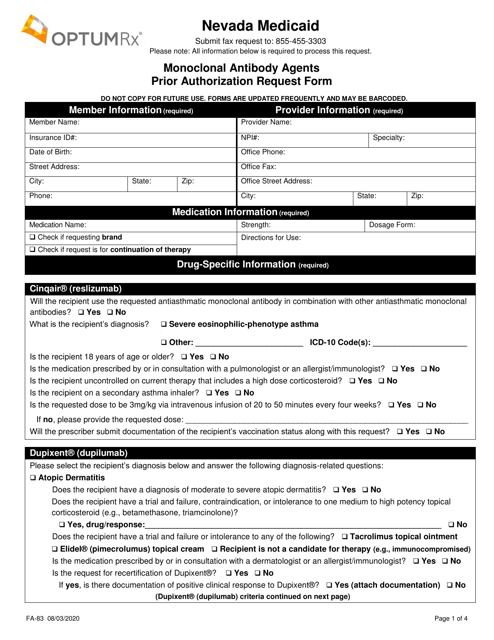
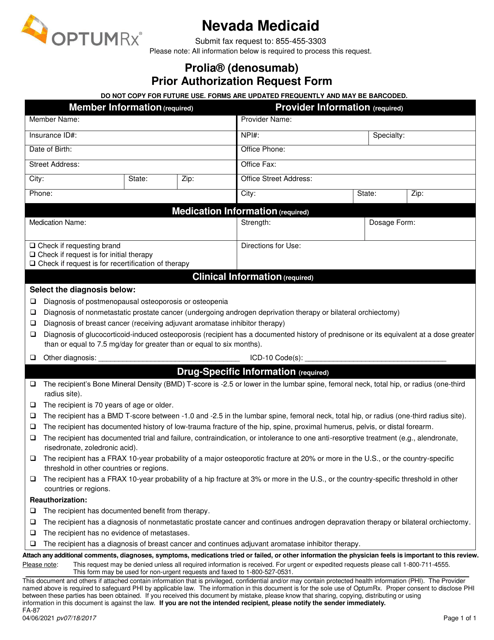
This Form is used for requesting prior authorization for targeted immunomodulators in Nevada. It helps ensure that the use of these medications is appropriate and meets necessary criteria.
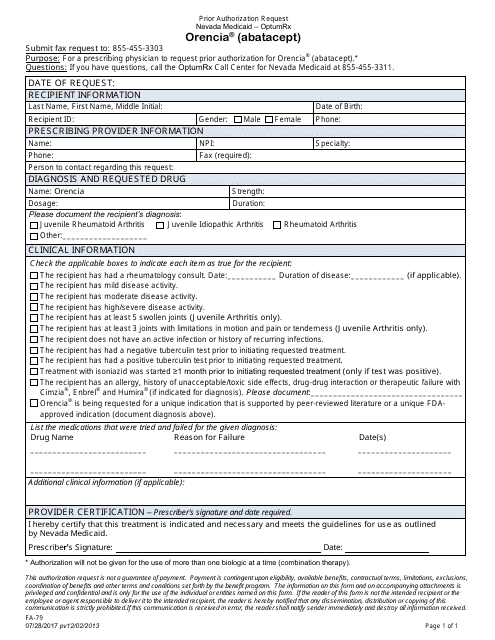
This form is used for submitting a prior authorization request for the medication Orencia (abatacept) in the state of Nevada.
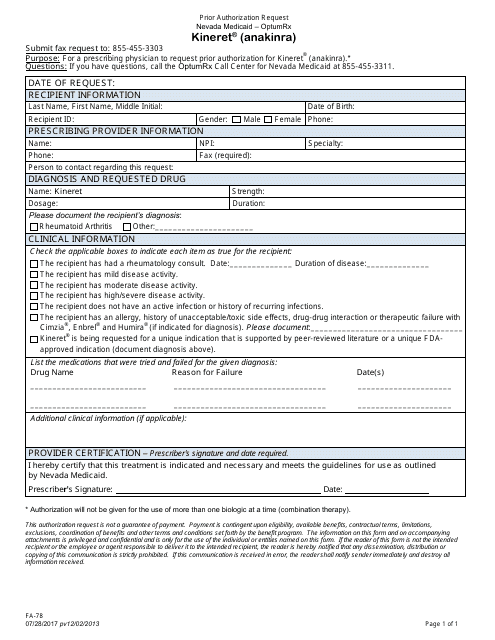
This form is used for submitting a prior authorization request for the medication Kineret (Anakinra) in the state of Nevada.
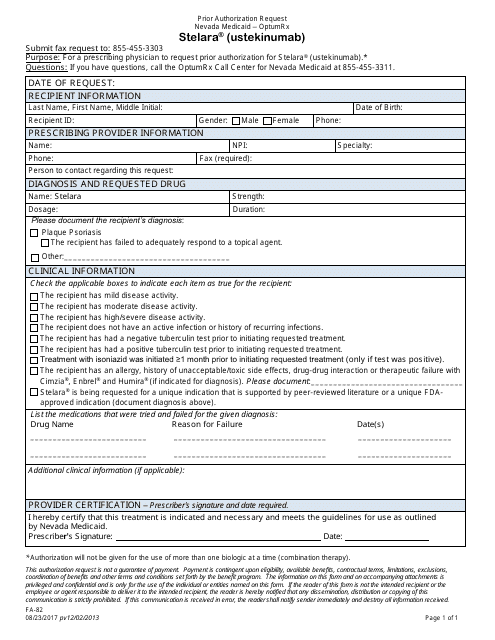
This form is used for submitting a prior authorization request for the medication Stelara (Ustekinumab) in the state of Nevada.
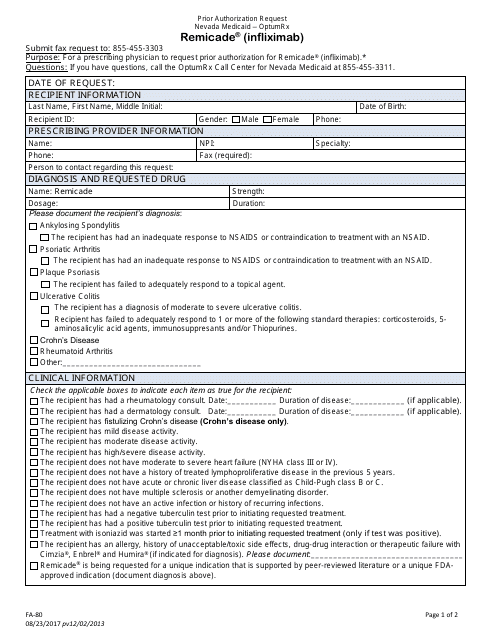
This form is used for requesting prior authorization for the medication Remicade (Infliximab) in the state of Nevada.
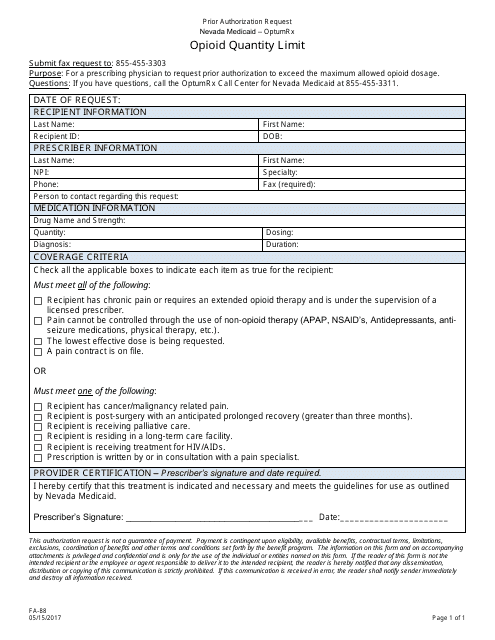
This Form is used for requesting prior authorization for an opioid quantity limit in the state of Nevada.
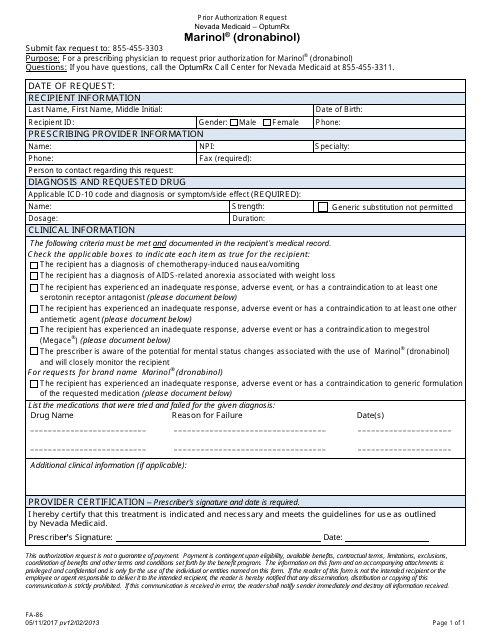
This Form is used for submitting a prior authorization request for Marinol (Dronabinol) medication in Nevada.
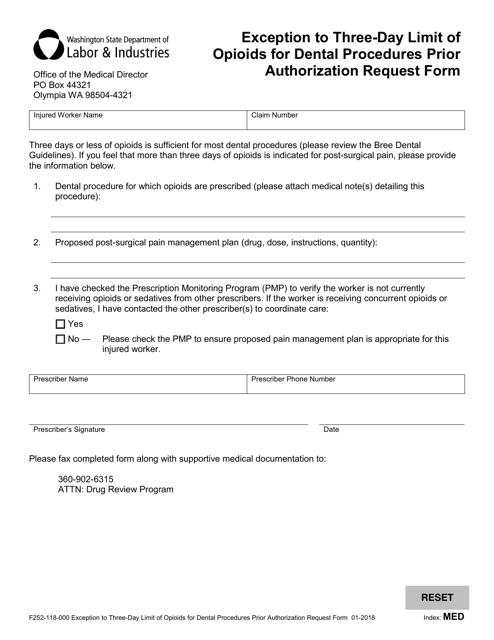
This form is used for requesting prior authorization to exceed the three-day limit of opioids for dental procedures in the state of Washington.
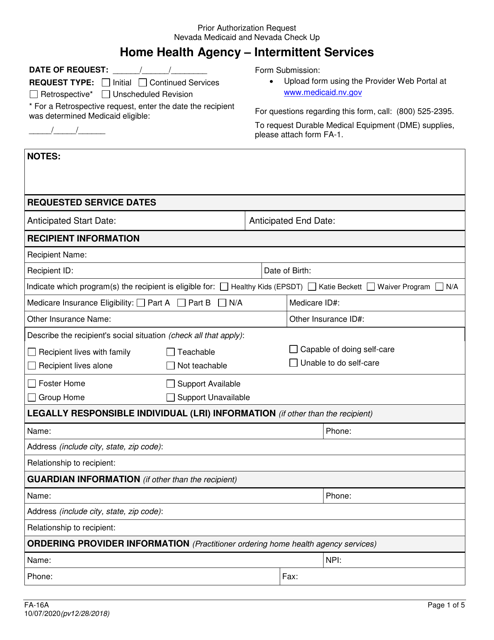
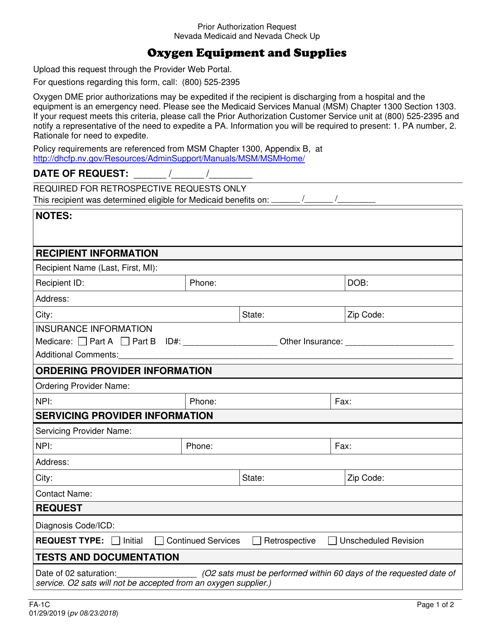
This form is used for requesting prior authorization for oxygen equipment and supplies in Nevada.