Coverage Determination Templates
Are you looking for information about coverage determinations and the process to request one? Look no further than our comprehensive collection of documents and forms related to coverage determinations.
Also known as coverage determination forms, these important documents play a crucial role in determining whether specific medical services, treatments, or prescription drugs will be covered by your healthcare provider or insurance plan. Our collection includes a variety of useful resources to help you navigate the coverage determination process.
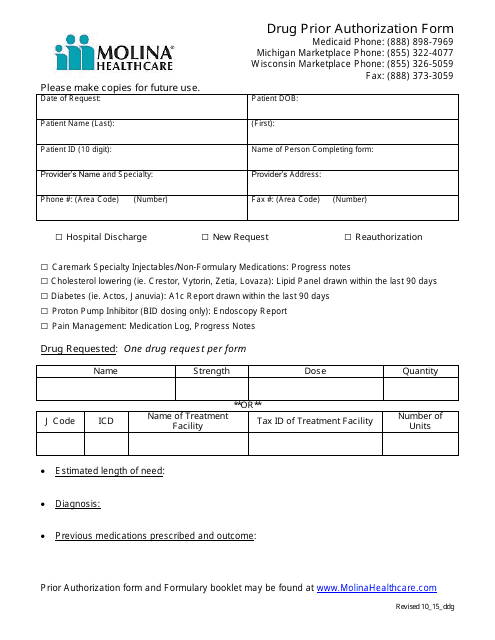
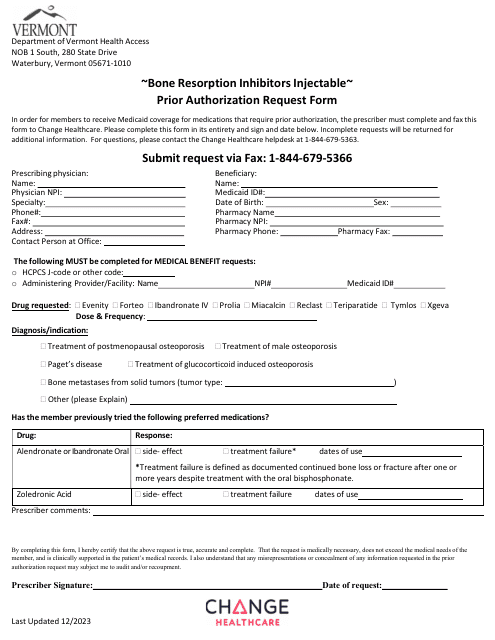
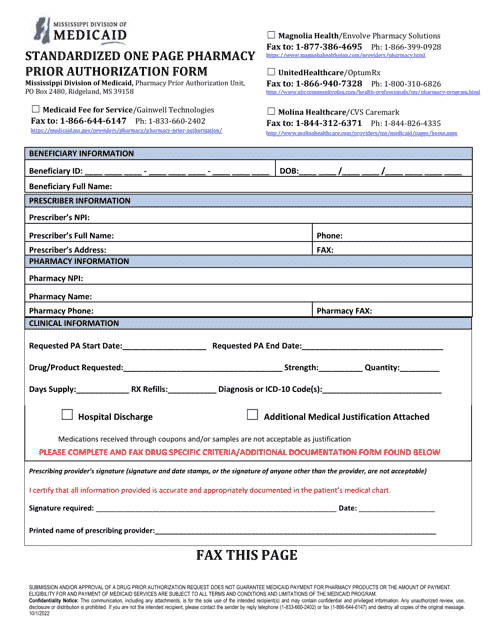
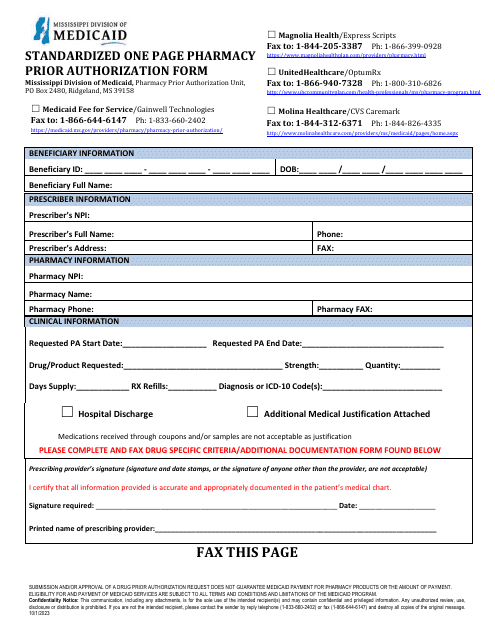
If you're in need of a drug prior authorization, we have a specific form designed to facilitate this process. This form allows you to request coverage for a specific medication and provides all the necessary information for your healthcare provider to evaluate the request.
In addition to the drug prior authorization form, we have an extensive list of documents that can guide you through the coverage determination process. From request forms to detailed instructions, our collection provides you with everything you need to make a strong case for coverage.
Whether you're facing a prior authorization requirement for opioids or brand name multi-source medications in Mississippi, we have the prior authorization packets that contain all the required documentation for these specific situations.
Don't let the complexity of coverage determinations overwhelm you. Our collection of documents and forms is here to simplify the process and ensure you have the best chance of receiving the coverage you need. Trust our comprehensive resource library to provide you with the information and tools necessary to navigate coverage determinations effectively.
Documents:
10
This form is used for requesting prior authorization for drugs through Molina Healthcare.
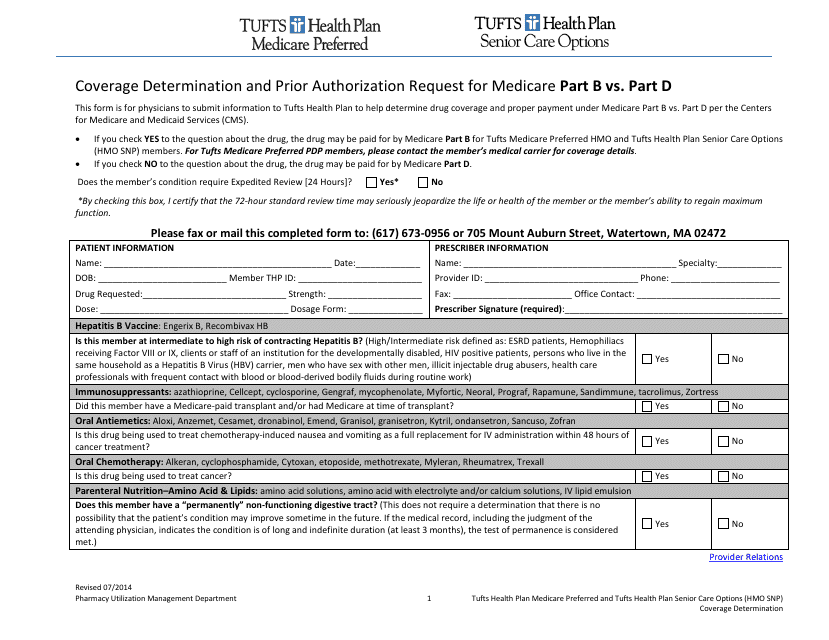
This Form is used for submitting a coverage determination request or prior authorization request for Medicare Part B or Part D benefits under Tufts insurance.
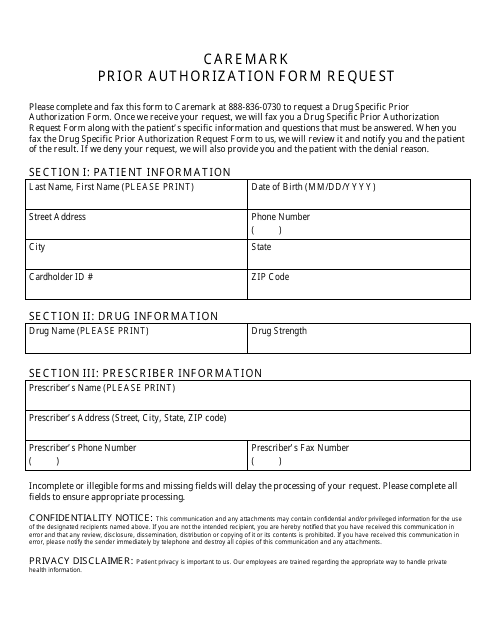
This Form is used for requesting prior authorization for medications through Cvs Caremark.
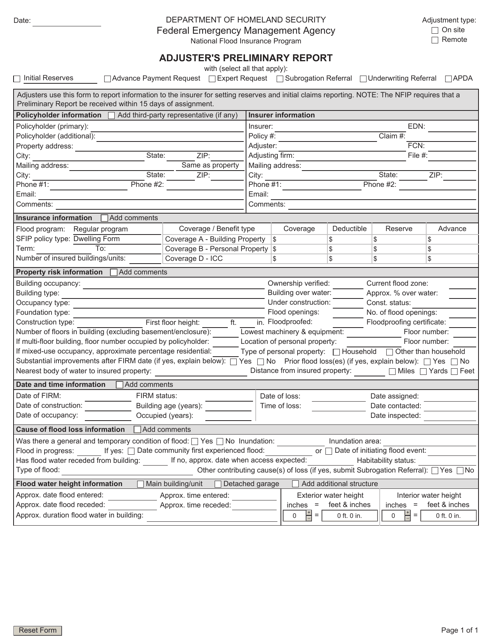
This document is used by insurance adjusters to provide an initial assessment and report on the damage and value of a claim. It helps determine the next steps for the claims process.
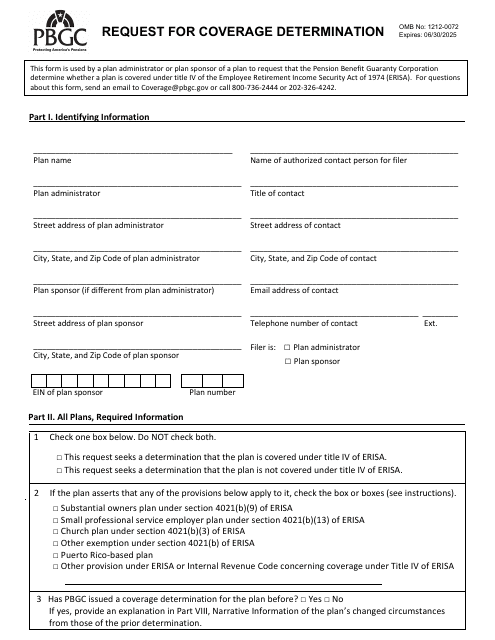
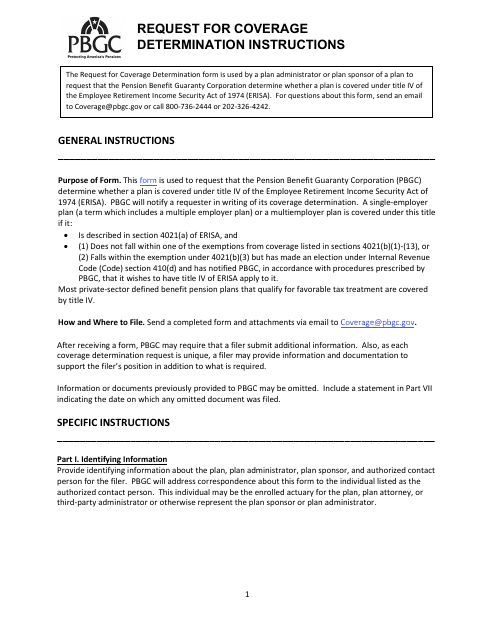
This document is used to request a determination of coverage for an insurance claim or benefit. It typically involves submitting information and evidence to support the request and may be required by the insurance company before they make a decision on coverage.
This document provides instructions on how to request a coverage determination.
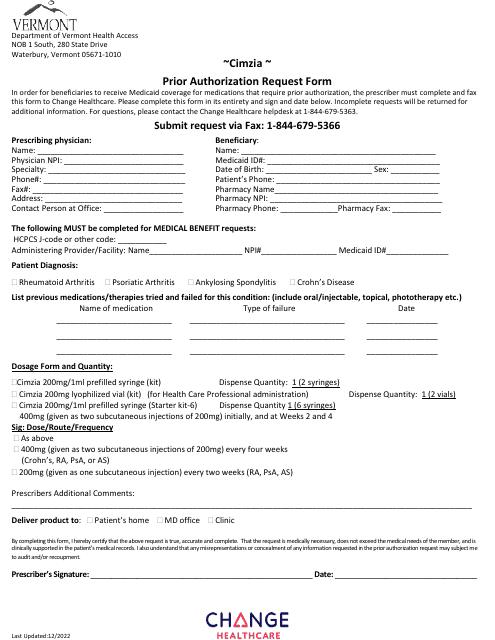
This Form is used for submitting a prior authorization request for Cimzia medication in the state of Vermont.
This document is used for obtaining prior authorization for opioids in the state of Mississippi. It includes the necessary paperwork and information required to request approval for the use of these medications.