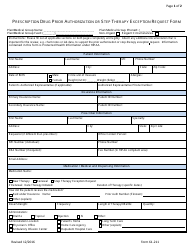
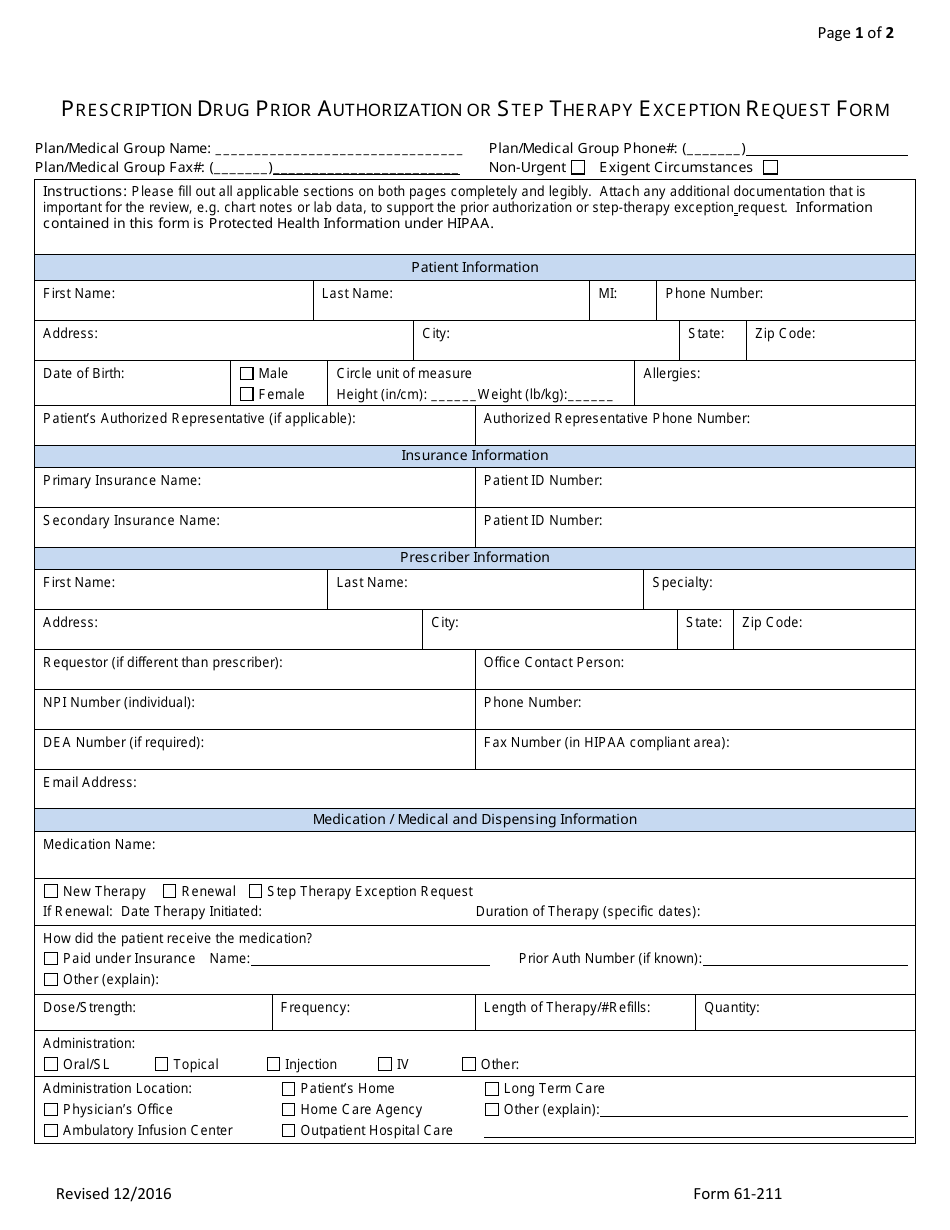
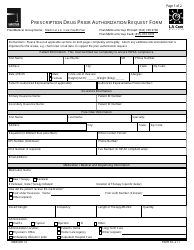
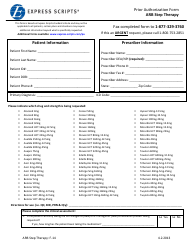
Form 61-211 Prescription Drug Prior Authorization or Step Therapy Exception Request Form - Express Scripts
Form 61-211 Prescription Drug Prior Authorization or Step Therapy Exception Request Form - Express Scripts is used to request prior authorization or an exception to step therapy for prescription drugs. It helps ensure that the appropriate drugs are prescribed and covered by insurance.
The Form 61-211 Prescription Drug Prior Authorization or Step Therapy Exception Request Form for Express Scripts is typically filled out by patients or their healthcare providers.
FAQ
Q: What is the Form 61-211?
A: Form 61-211 is the Prescription Drug Prior Authorization or Step Therapy Exception Request Form.
Q: Who is Express Scripts?
A: Express Scripts is a pharmacy benefits management organization that administers prescription drug programs.
Q: What is the purpose of Form 61-211?
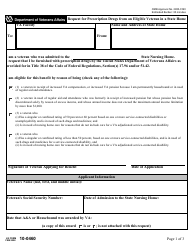
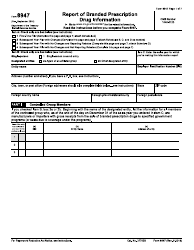
A: The purpose of Form 61-211 is to request prior authorization for a prescription drug or to request an exception to step therapy requirements.
Q: What is prior authorization?
A: Prior authorization is a process where a healthcare provider obtains approval from the insurance company before prescribing certain medications.
Q: What is step therapy?
A: Step therapy is a process where patients must try less expensive or alternative medications before being approved for more expensive drugs.