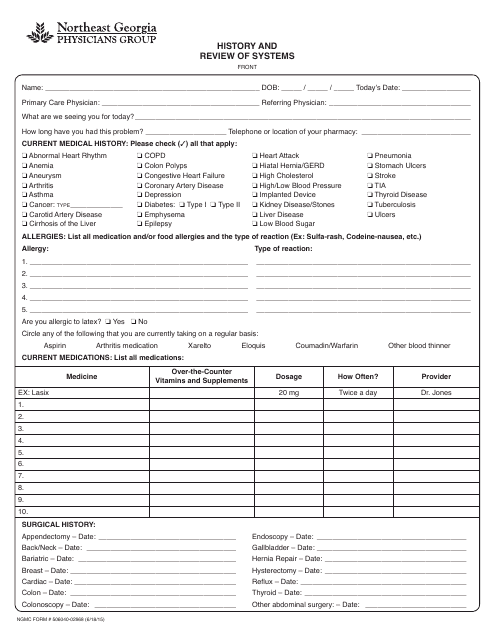
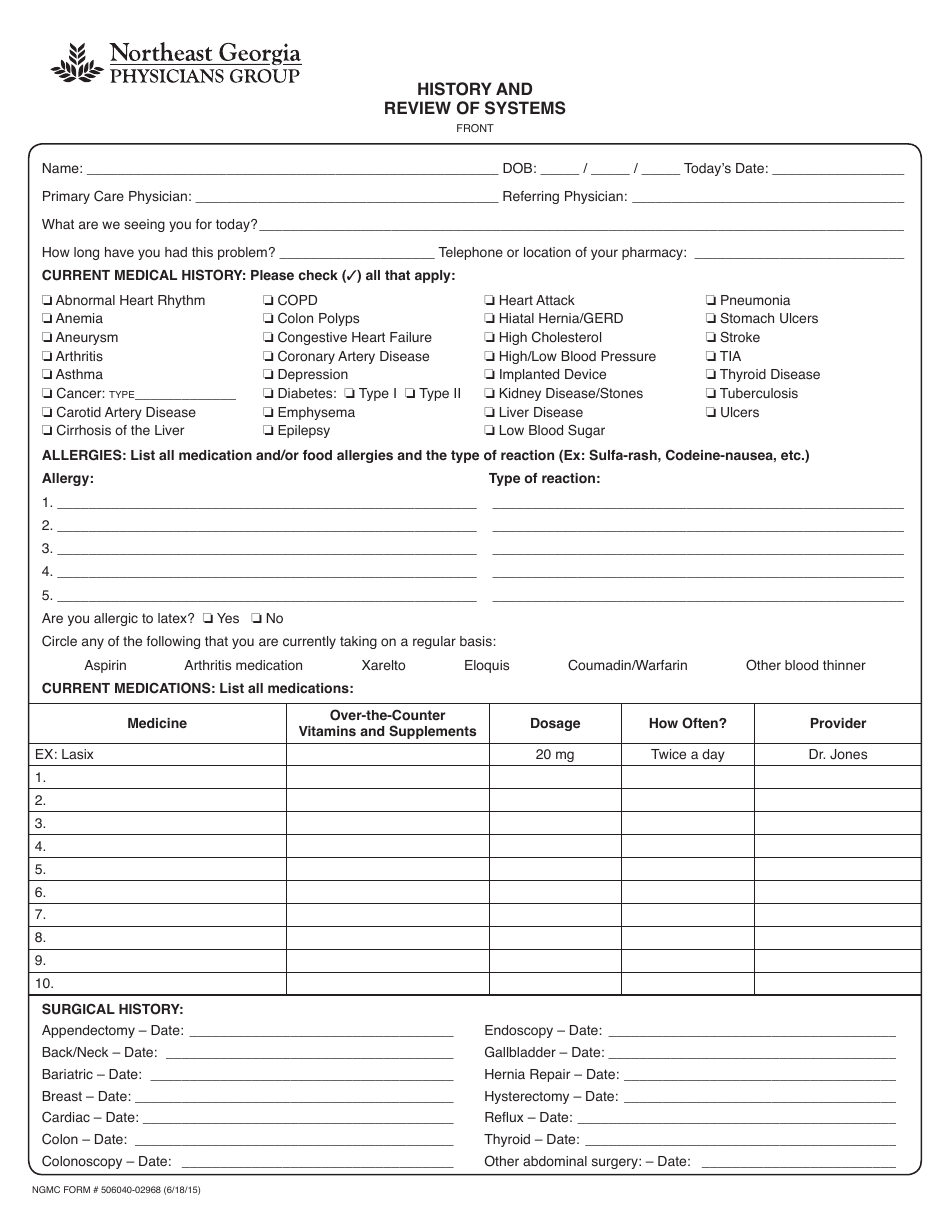
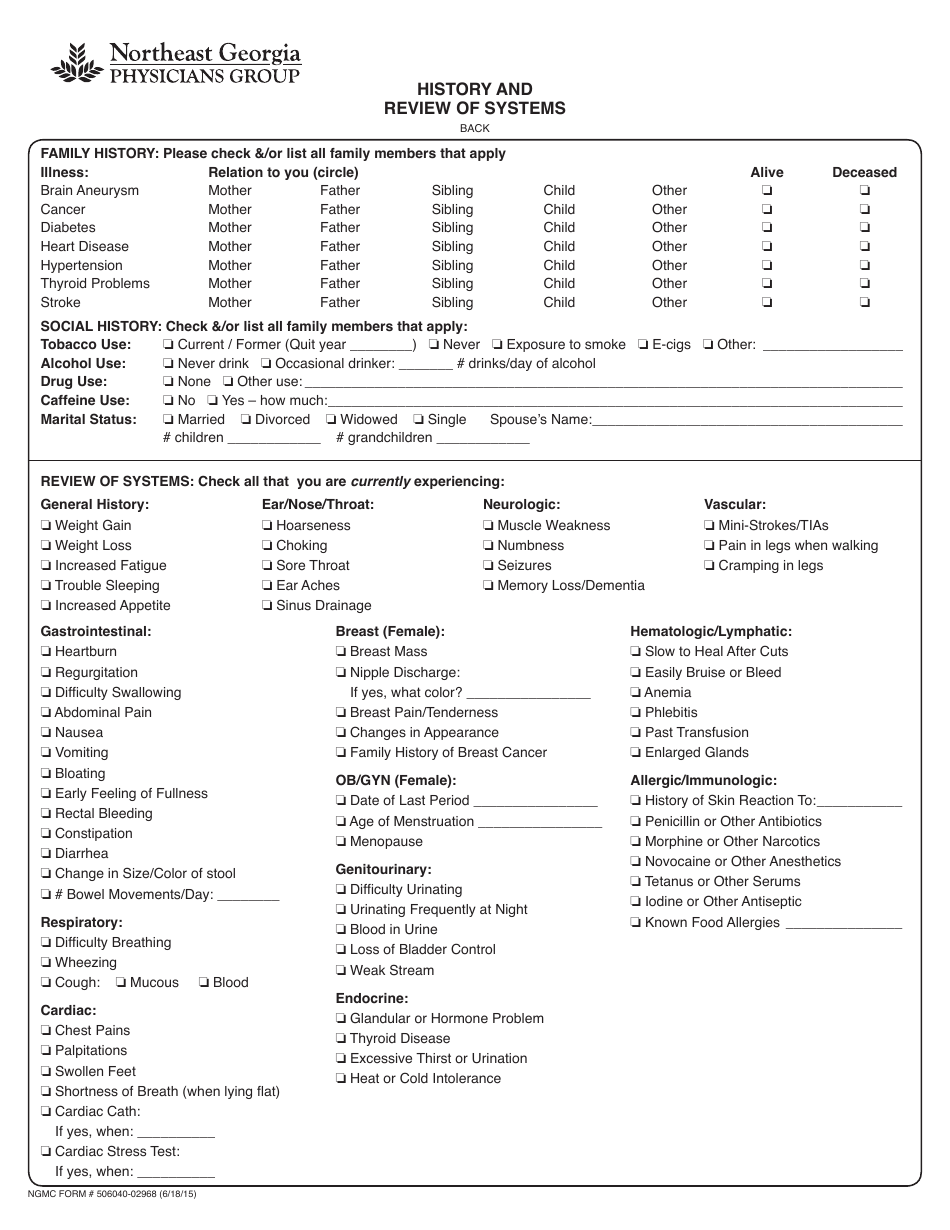
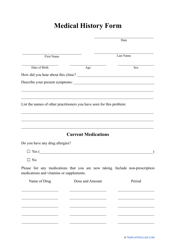
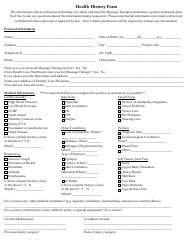
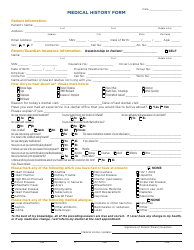
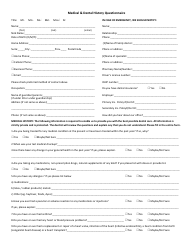
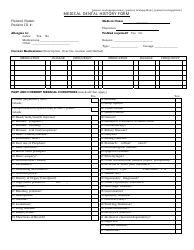
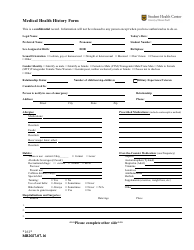
Medical History and Review of Systems Form - Northeast Georgia Physicians Group
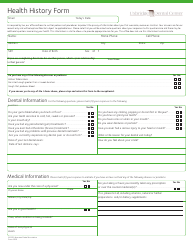
The Medical History and Review of Systems Form from Northeast Georgia Physicians Group is used to gather information about a patient's medical history, current health status, and any symptoms or concerns they may have. It helps healthcare providers in assessing a patient's overall health and identifying any potential health issues or conditions.
FAQ
Q: What is a medical history and review of systems form?
A: A medical history and review of systems form is a document used by healthcare providers to gather information about a patient's past medical conditions and current symptoms.
Q: Why do healthcare providers use a medical history and review of systems form?
A: Healthcare providers use this form to obtain a comprehensive understanding of a patient's medical history, current health status, and potential risk factors.
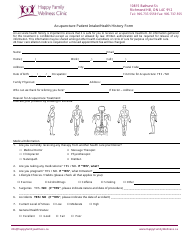
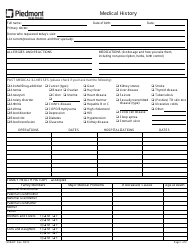
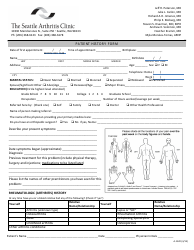
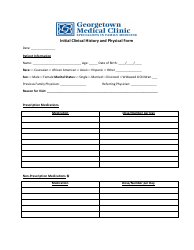
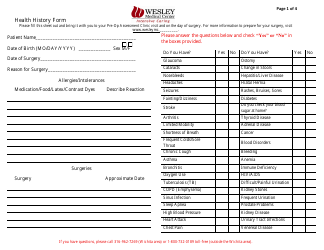
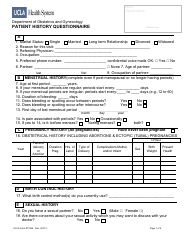
Q: What information is typically included in a medical history and review of systems form?
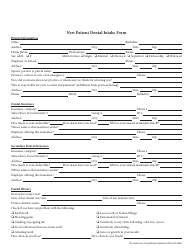
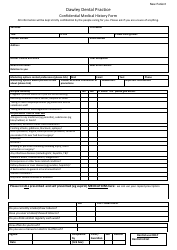
A: The form usually includes sections for personal and family medical history, current medications, allergies, past surgeries, and an overview of the patient's various body systems.
Q: Why is it important for patients to complete a medical history and review of systems form accurately and thoroughly?
A: Completing the form accurately and thoroughly helps healthcare providers make more informed decisions about diagnosis, treatment, and preventative care.
Q: How can patients obtain a copy of their medical history and review of systems form?
A: Patients can request a copy of their completed form from their healthcare provider's office or ask for electronic access, if available.
Q: Is the information provided on a medical history and review of systems form confidential?
A: Yes, healthcare providers have a legal and ethical duty to protect patient confidentiality, and the information provided on the form is kept confidential.
Q: Can patients update their medical history and review of systems form in the future?
A: Yes, patients should inform their healthcare provider of any changes to their medical history or current health status during subsequent visits, so the form can be updated accordingly.