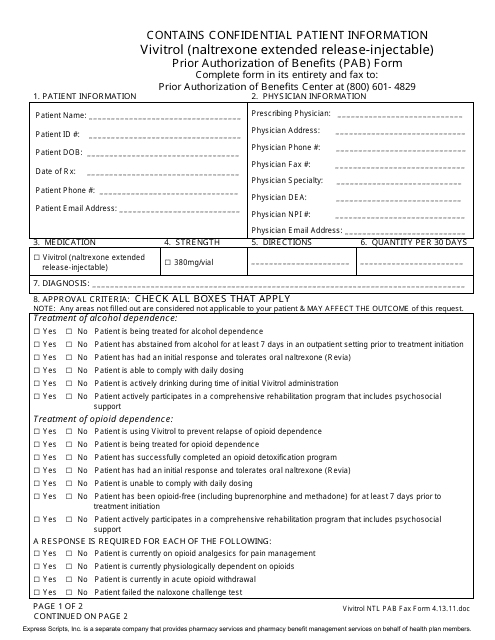
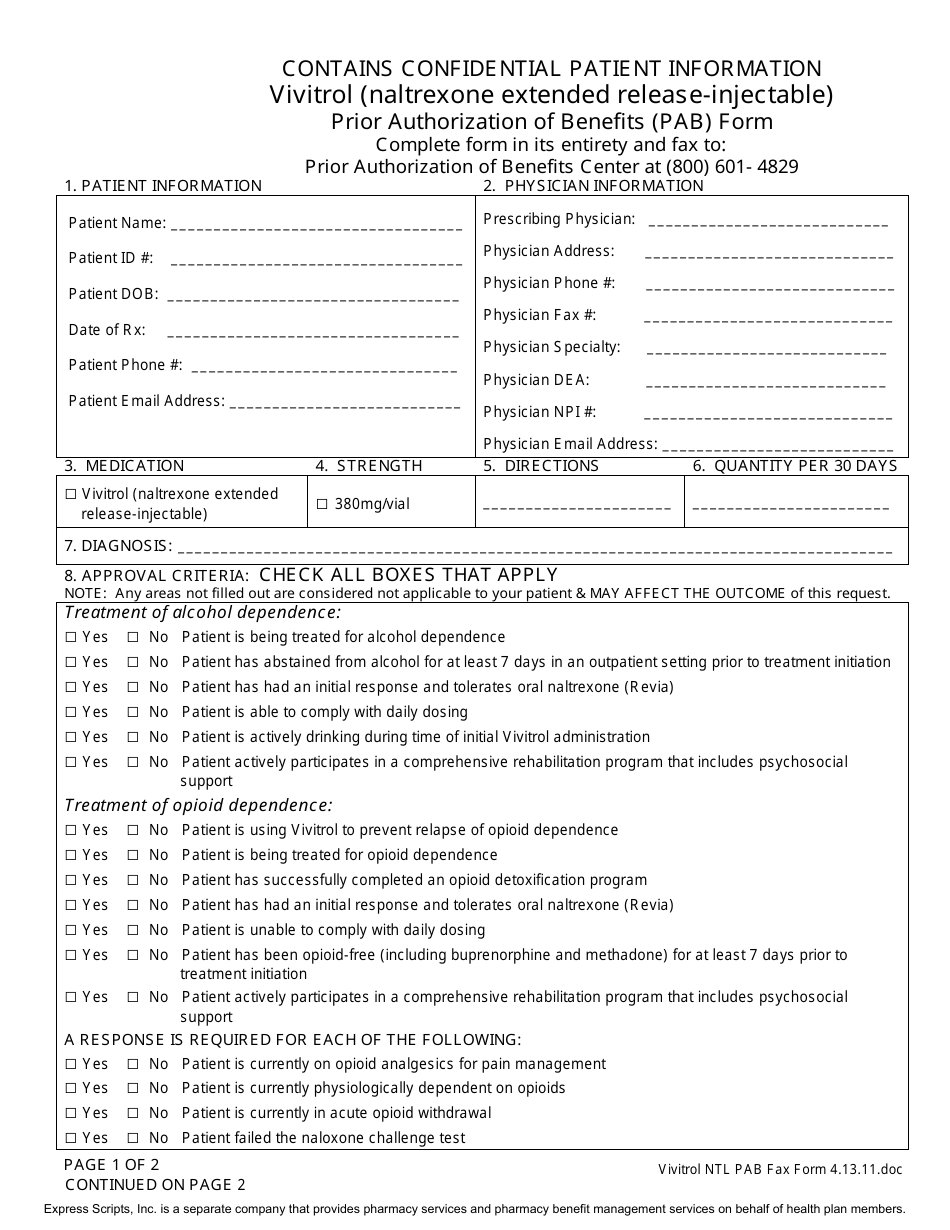
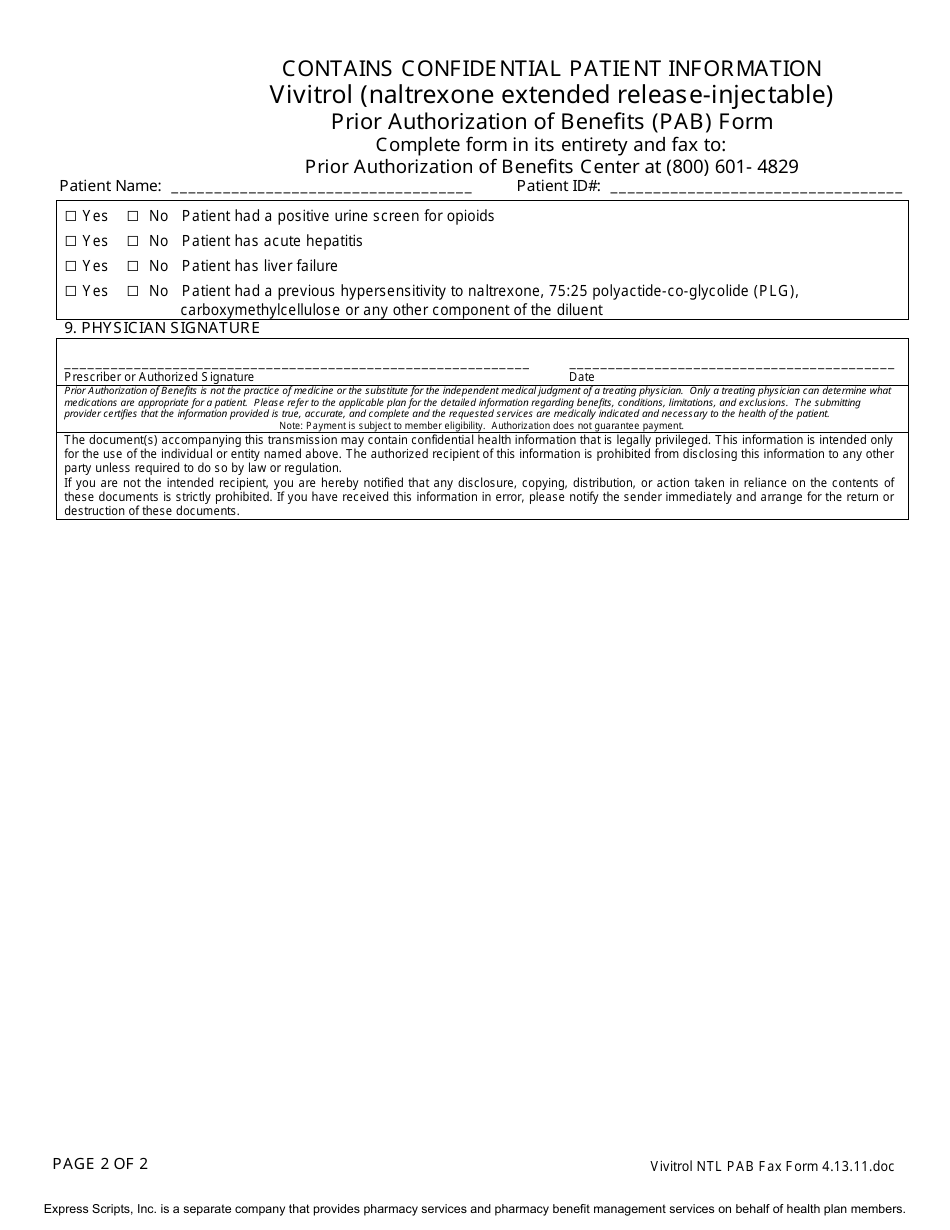
Vivitrol (Naltrexone Extended Release-Injectable) Prior Authorization of Benefits (Pab) Form - Express Scripts
Vivitrol, or Naltrexone Extended Release-Injectable, is a medication used for the treatment of alcohol or opioid dependence. The Prior Authorization of Benefits (PAB) form is used by Express Scripts to determine if a patient's insurance plan covers the cost of Vivitrol.
FAQ
Q: What is Vivitrol?
A: Vivitrol is a medication that contains the active ingredient Naltrexone and is used to treat alcohol or opioid dependence.
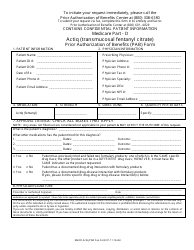
Q: What is a Prior Authorization of Benefits (PAB) form?
A: A Prior Authorization of Benefits (PAB) form is a document that needs to be filled out and submitted to Express Scripts for approval before coverage for Vivitrol can be authorized.
Q: What is Naltrexone Extended Release-Injectable?
A: Naltrexone Extended Release-Injectable is the generic name for Vivitrol, which is a long-acting injectable form of the medication Naltrexone.
Q: What is the purpose of a Prior Authorization?
A: A Prior Authorization is required by your insurance company to ensure that the medication, in this case Vivitrol, is medically necessary and meets their coverage criteria before they will approve and cover its cost.
Q: How do I complete the Vivitrol Prior Authorization of Benefits (PAB) form?
A: The Vivitrol Prior Authorization of Benefits (PAB) form requires you to provide personal and medical information, along with details about your prescribing healthcare provider and the reasons why you need Vivitrol.
Q: Why do I need to submit a Prior Authorization of Benefits (PAB) form to Express Scripts?
A: Express Scripts requires a Prior Authorization of Benefits (PAB) form to determine if you meet the necessary criteria for their coverage of Vivitrol.
Q: Who should I contact if I have questions about the Vivitrol Prior Authorization of Benefits (PAB) form?
A: If you have any questions about the Vivitrol Prior Authorization of Benefits (PAB) form, you should contact Express Scripts customer service for assistance.
Q: How long does it take to get a Prior Authorization approved?
A: The time it takes to get a Prior Authorization approved can vary, but it typically takes a few days to a week for a decision to be made.
Q: What happens if my Prior Authorization for Vivitrol is denied?
A: If your Prior Authorization for Vivitrol is denied, you may need to work with your healthcare provider and your insurance company to explore other options for coverage or appeal the decision.