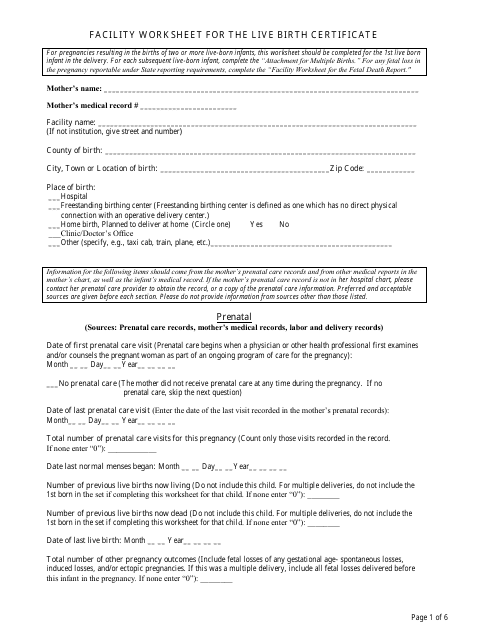
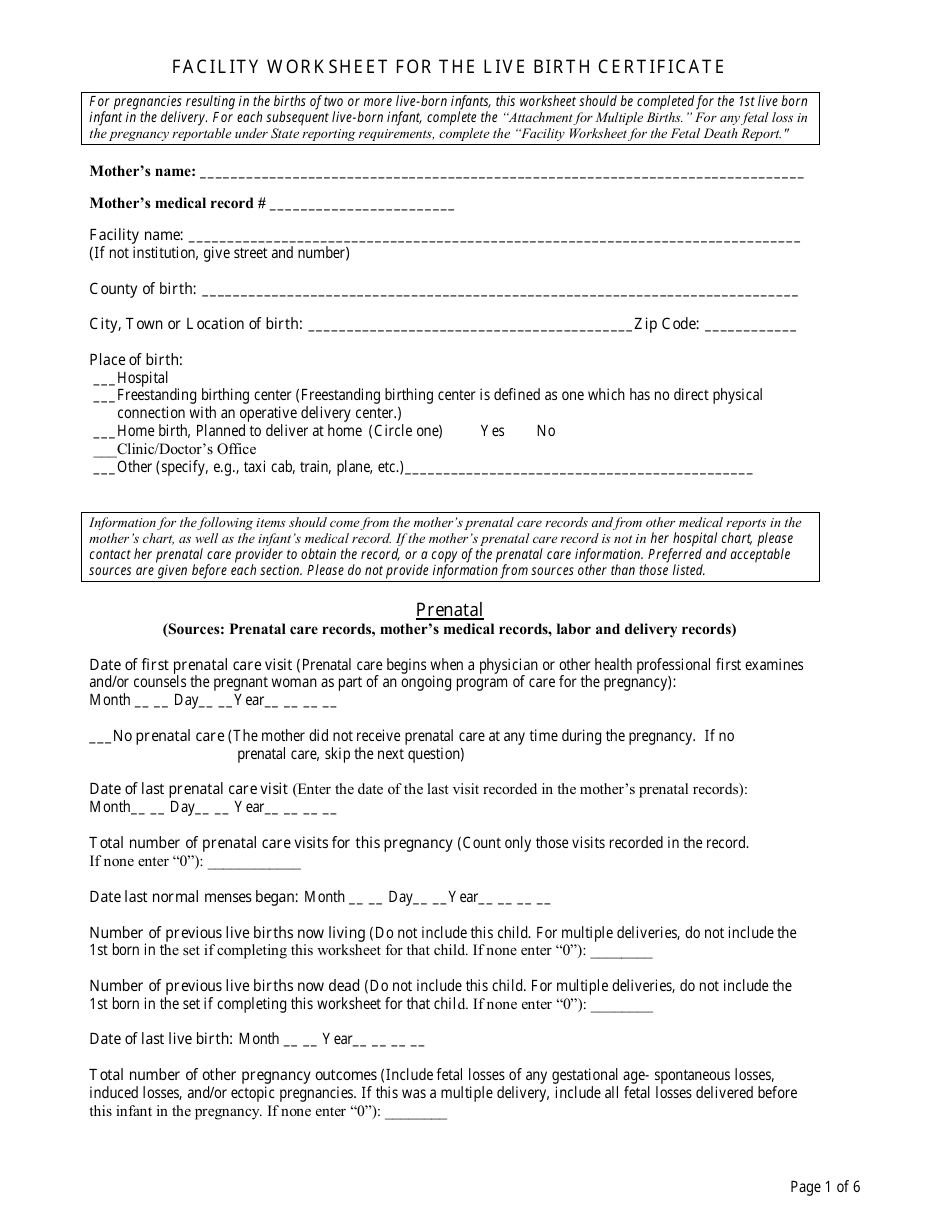
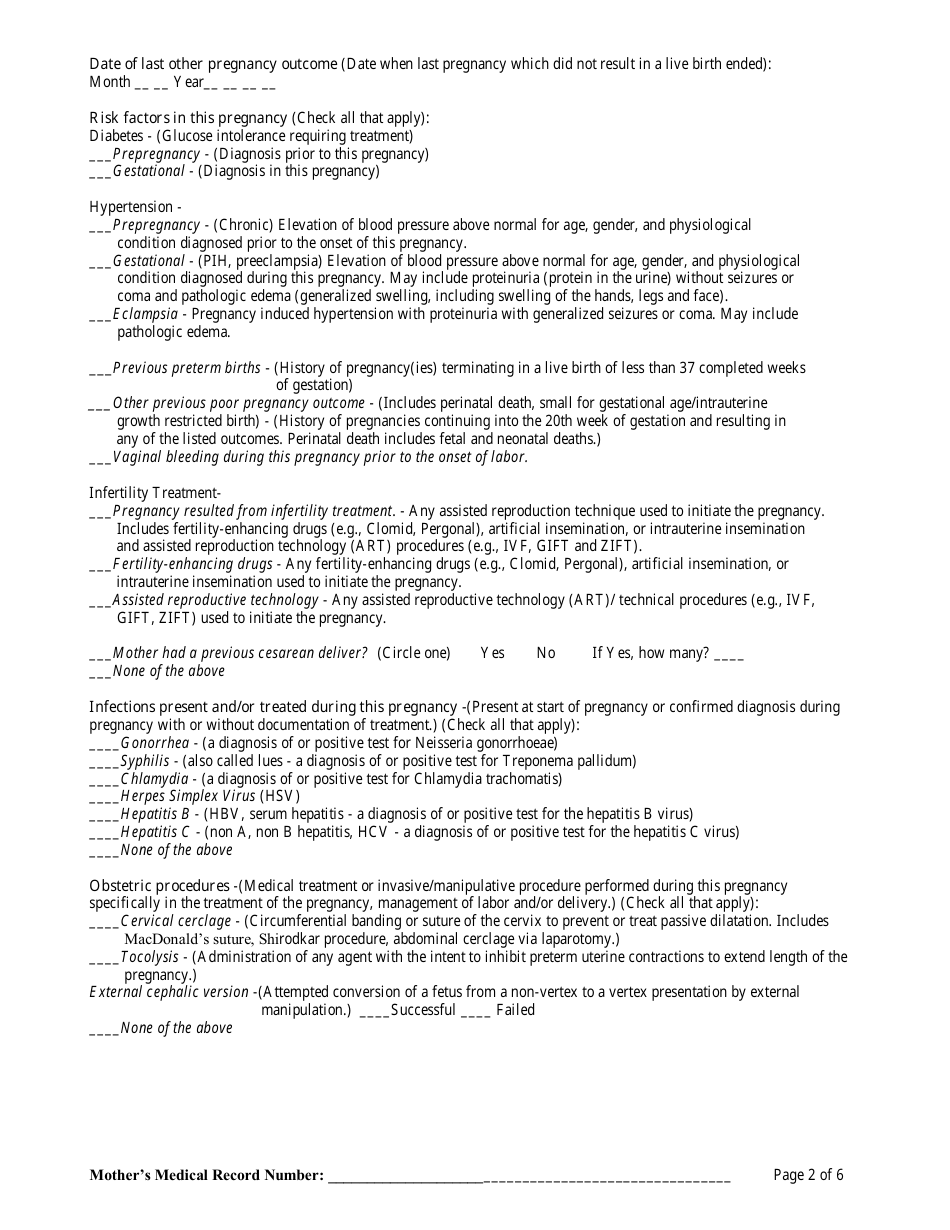
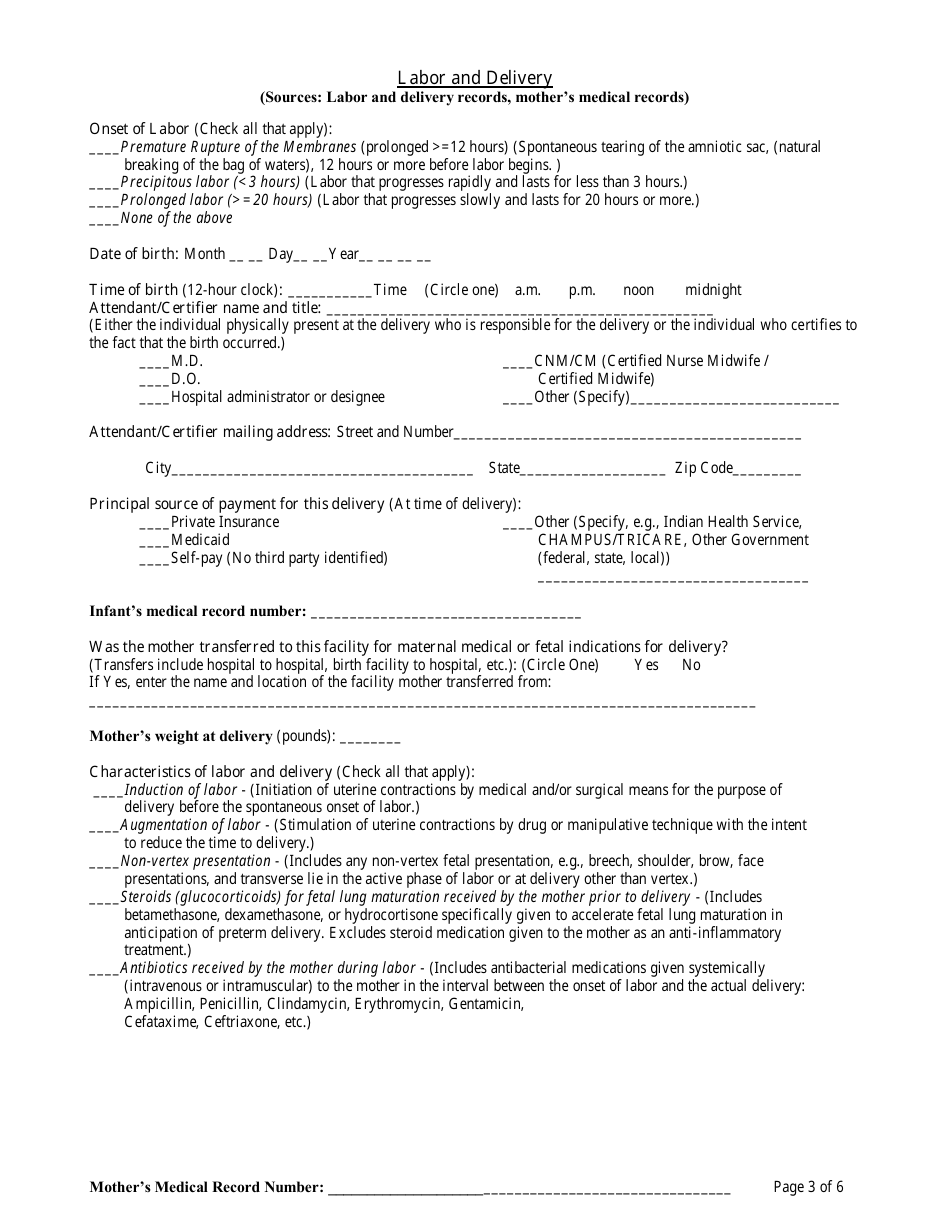
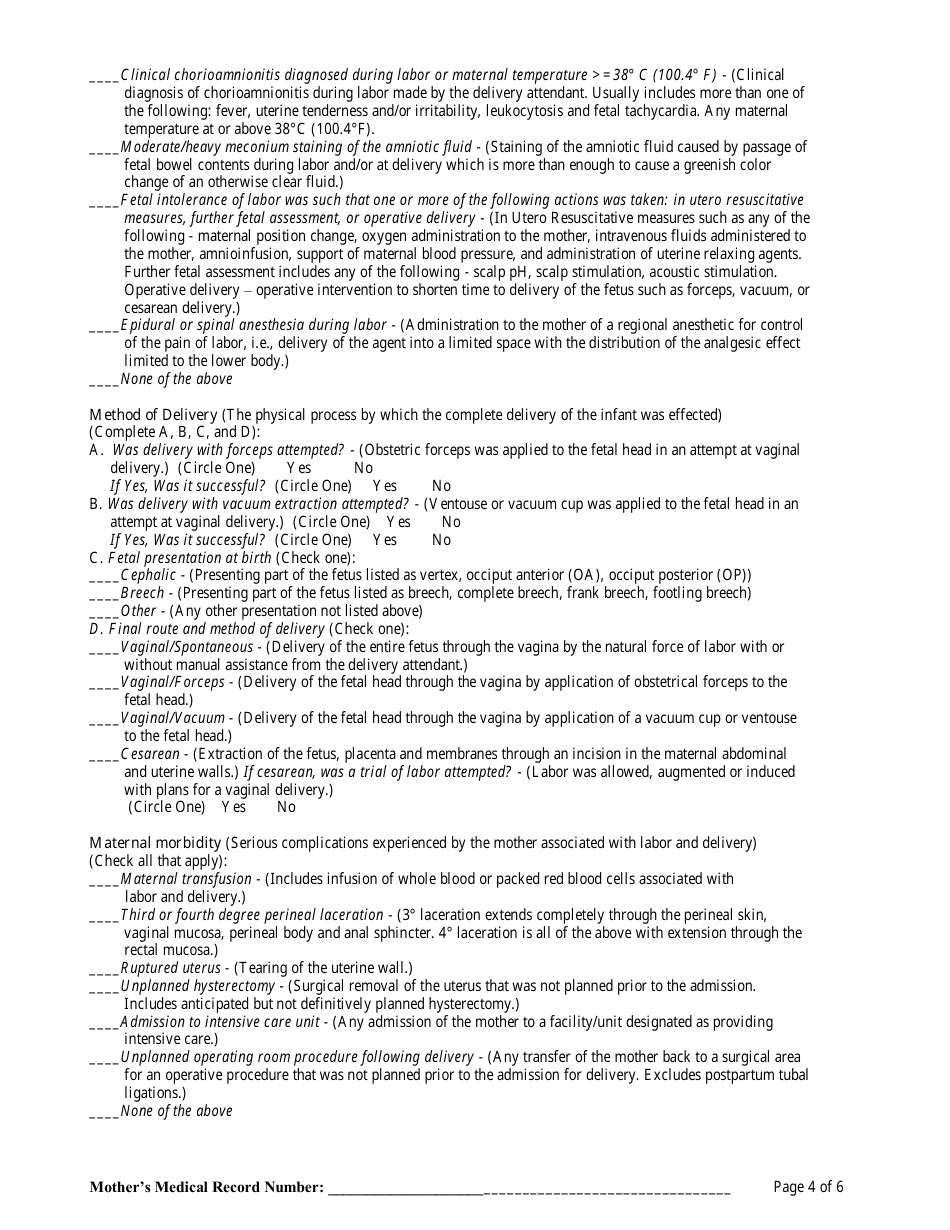
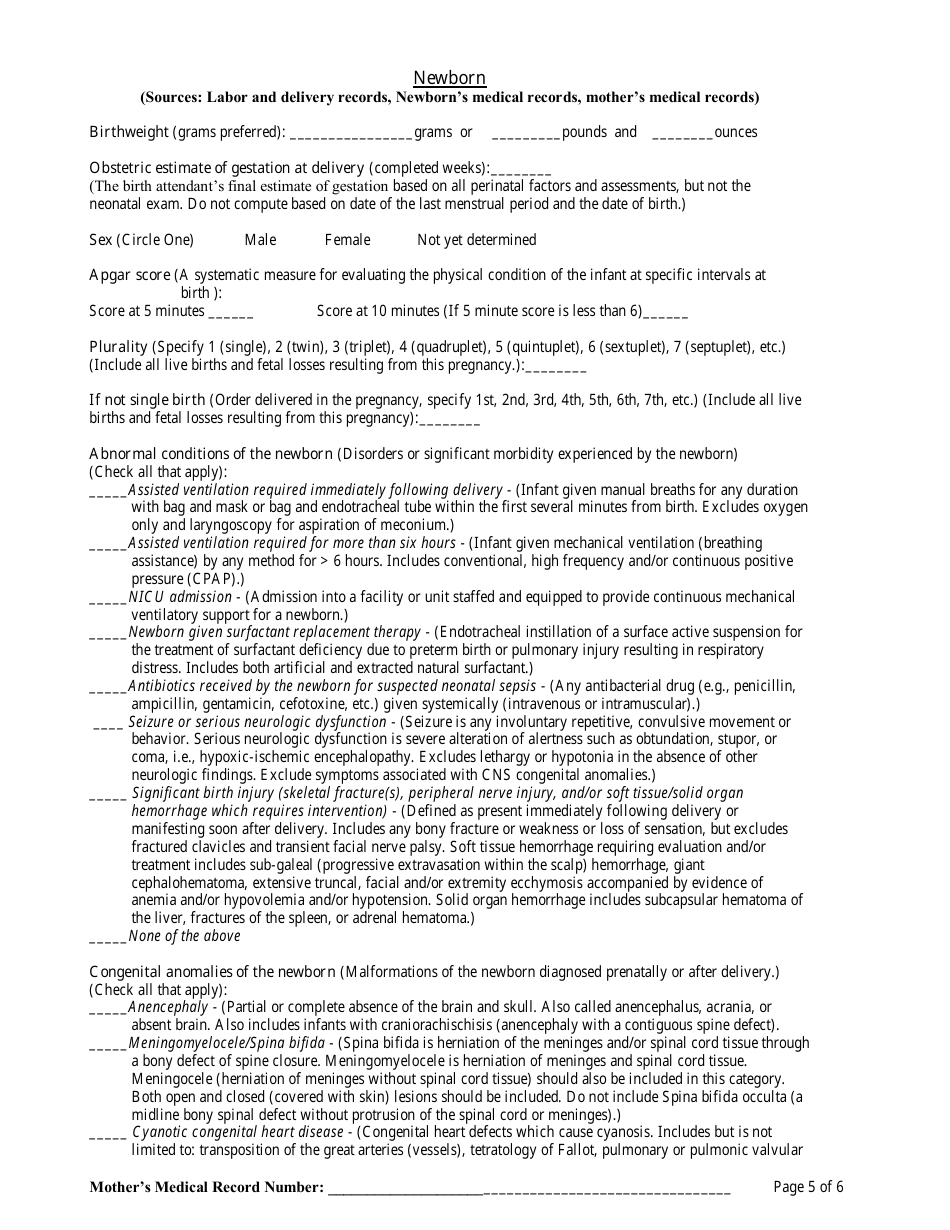
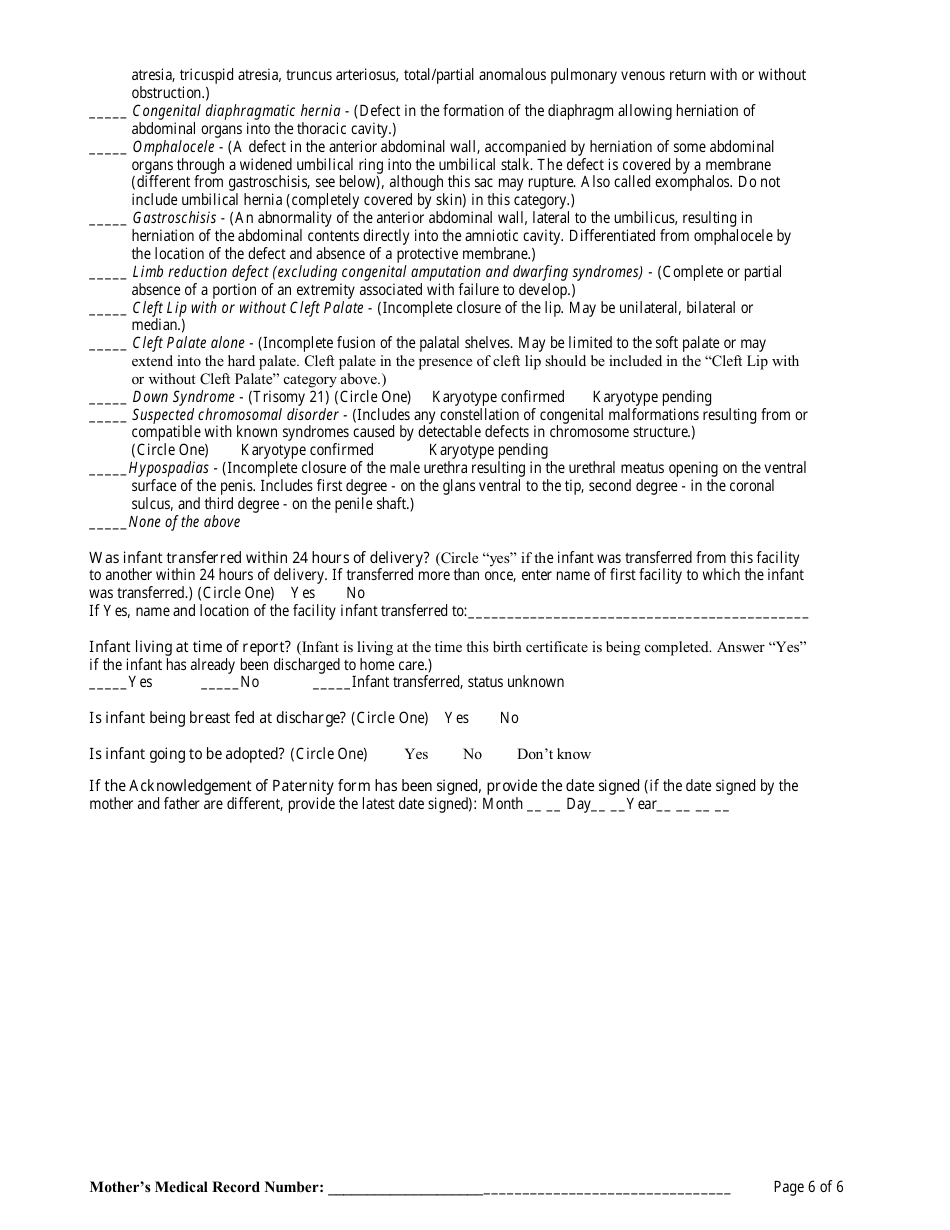
Facility Worksheet for the Live Birth Certificate
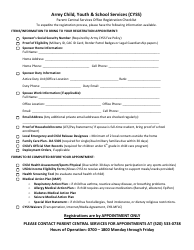
The Facility Worksheet for the Live Birth Certificate is used to document information about the facility where the birth took place. It includes details such as the facility name, address, and type.
The facility where the live birth occurs typically files the facility worksheet for the live birth certificate.
FAQ
Q: What is a Live Birth Certificate?
A: A Live Birth Certificate is an official document that records the birth of a child.
Q: How can I obtain a Live Birth Certificate?
A: You can obtain a Live Birth Certificate by contacting the Vital Records office in the state where the child was born.
Q: What information is typically included in a Live Birth Certificate?
A: A Live Birth Certificate typically includes the child's full name, date and place of birth, parents' names, and registration number.
Q: Why do I need a Live Birth Certificate?
A: A Live Birth Certificate is often required as proof of citizenship, for enrolling in school, obtaining a passport, and other legal purposes.
Q: Can I get a Live Birth Certificate for myself?
A: No, a Live Birth Certificate is only issued for newborn babies.
Q: Is there a fee for obtaining a Live Birth Certificate?
A: Yes, there is usually a fee associated with obtaining a Live Birth Certificate.
Q: How long does it take to receive a Live Birth Certificate?
A: The processing time for a Live Birth Certificate varies by state, but it typically takes a few weeks.
Q: What should I do if I notice an error on my Live Birth Certificate?
A: If you notice an error on your Live Birth Certificate, you should contact the Vital Records office and request a correction.
Q: Can I use a photocopy of my Live Birth Certificate?
A: In most cases, a photocopy of a Live Birth Certificate is not considered valid. You should obtain an official certified copy.