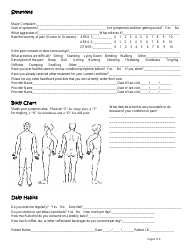
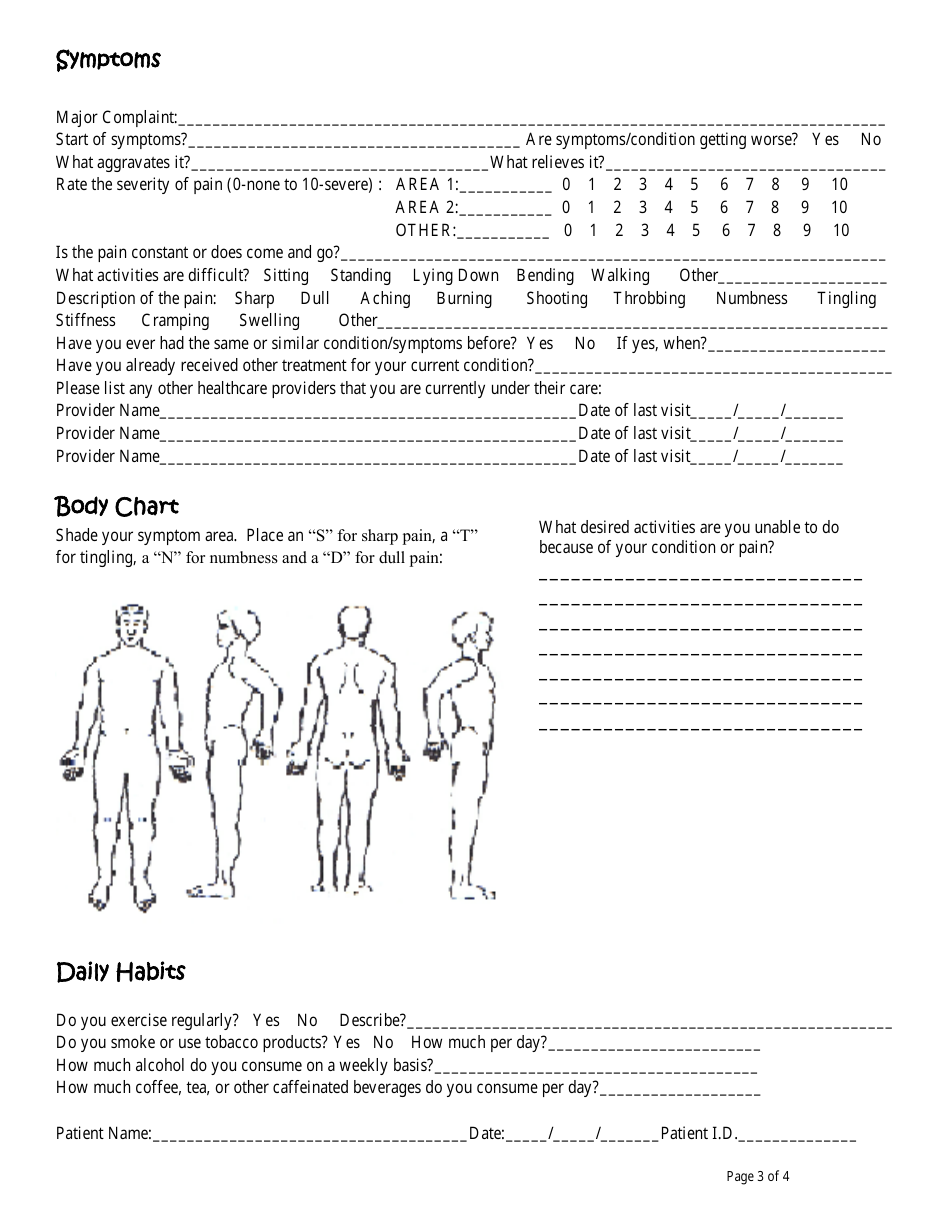
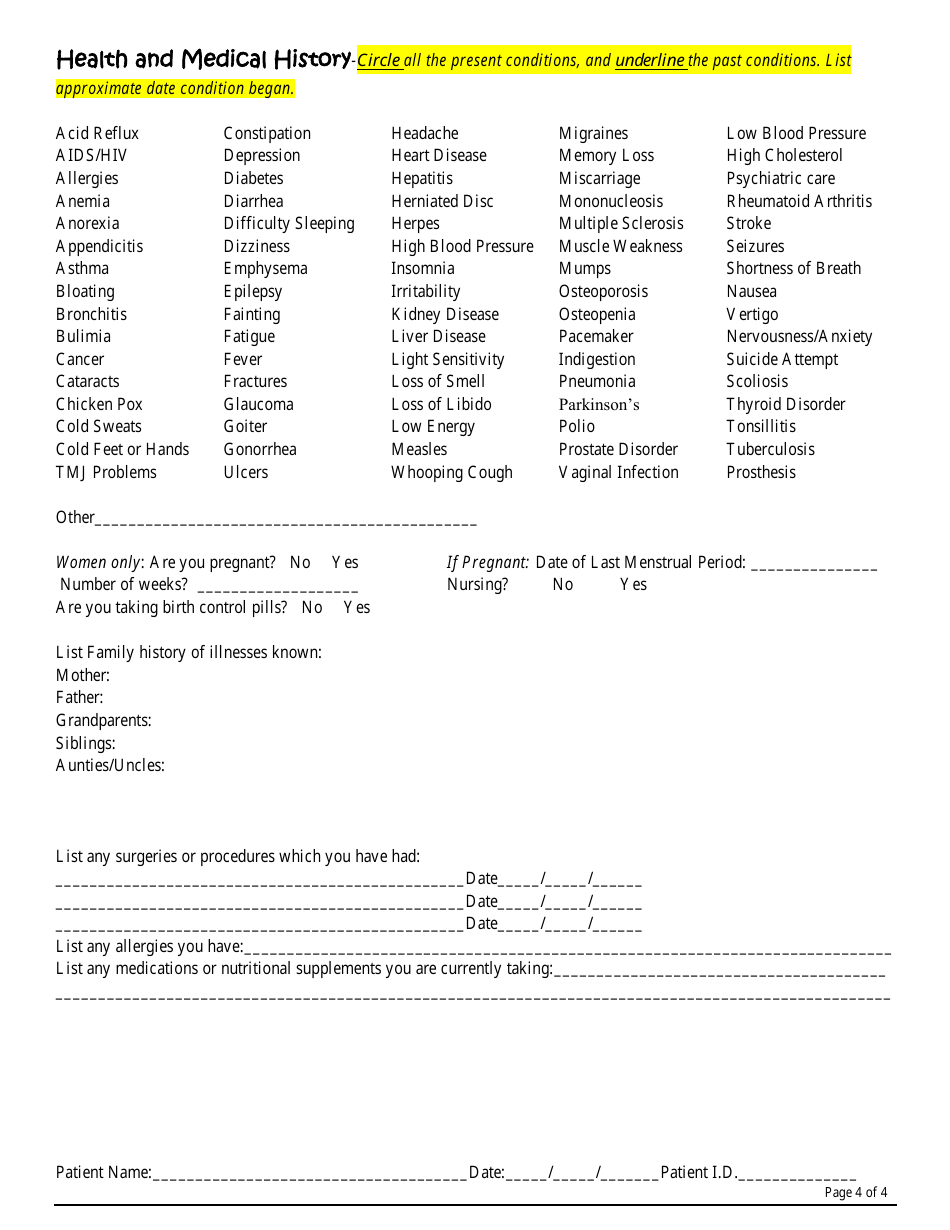
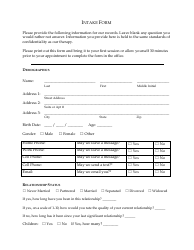
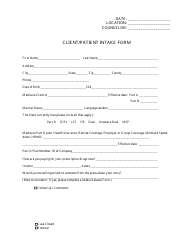
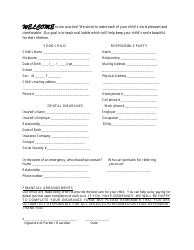
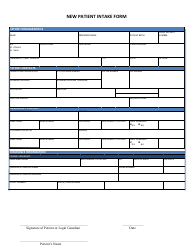
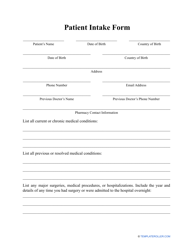
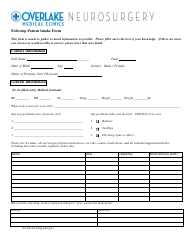
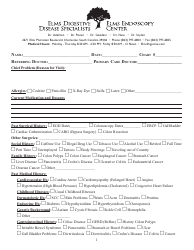
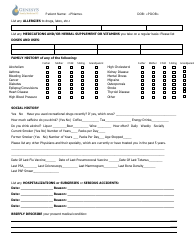
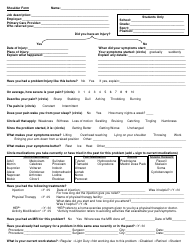
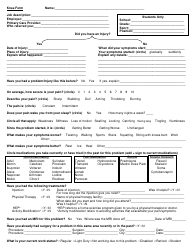
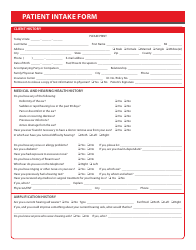
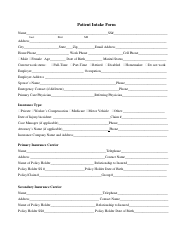
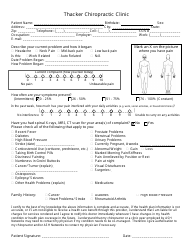
Patient Intake Form - With Daily Habits
A Patient Intake Form - With Daily Habits is used to collect information about a patient's medical history, current health status, and daily habits. It helps healthcare providers assess the patient's overall health and provide appropriate medical care.
The patient is responsible for filing the patient intake form with daily habits.
FAQ
Q: What is a patient intake form?
A: A patient intake form is a document used by healthcare providers to gather information about a patient's medical history, symptoms, and other relevant details.
Q: Why is a patient intake form important?
A: A patient intake form is important because it provides healthcare providers with valuable information to properly diagnose and treat patients.
Q: What should be included in a patient intake form?
A: A patient intake form should include personal information, medical history, current symptoms, allergies, medications, and any other relevant details about the patient's health.
Q: What are daily habits?
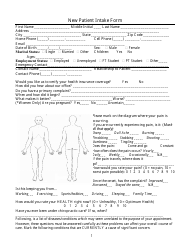
A: Daily habits refer to the activities and routines that a person engages in on a regular basis, such as eating, sleeping, exercise, smoking, and alcohol consumption.
Q: Why is it important to include daily habits in a patient intake form?
A: Including daily habits in a patient intake form helps healthcare providers assess lifestyle factors that may affect a patient's health and provide appropriate recommendations or interventions.
Q: What are examples of daily habits that should be included in a patient intake form?
A: Examples of daily habits that should be included in a patient intake form include dietary preferences, exercise frequency, smoking habits, alcohol consumption, and sleep patterns.
Q: How can daily habits impact a person's health?
A: Daily habits can have a significant impact on a person's health. For example, unhealthy eating habits or excessive alcohol consumption can increase the risk of developing certain diseases.
Q: Can daily habits be changed to improve health?
A: Yes, daily habits can be changed to improve health. Making positive changes to daily habits such as eating a balanced diet, exercising regularly, and avoiding harmful substances can have a beneficial effect on overall health.