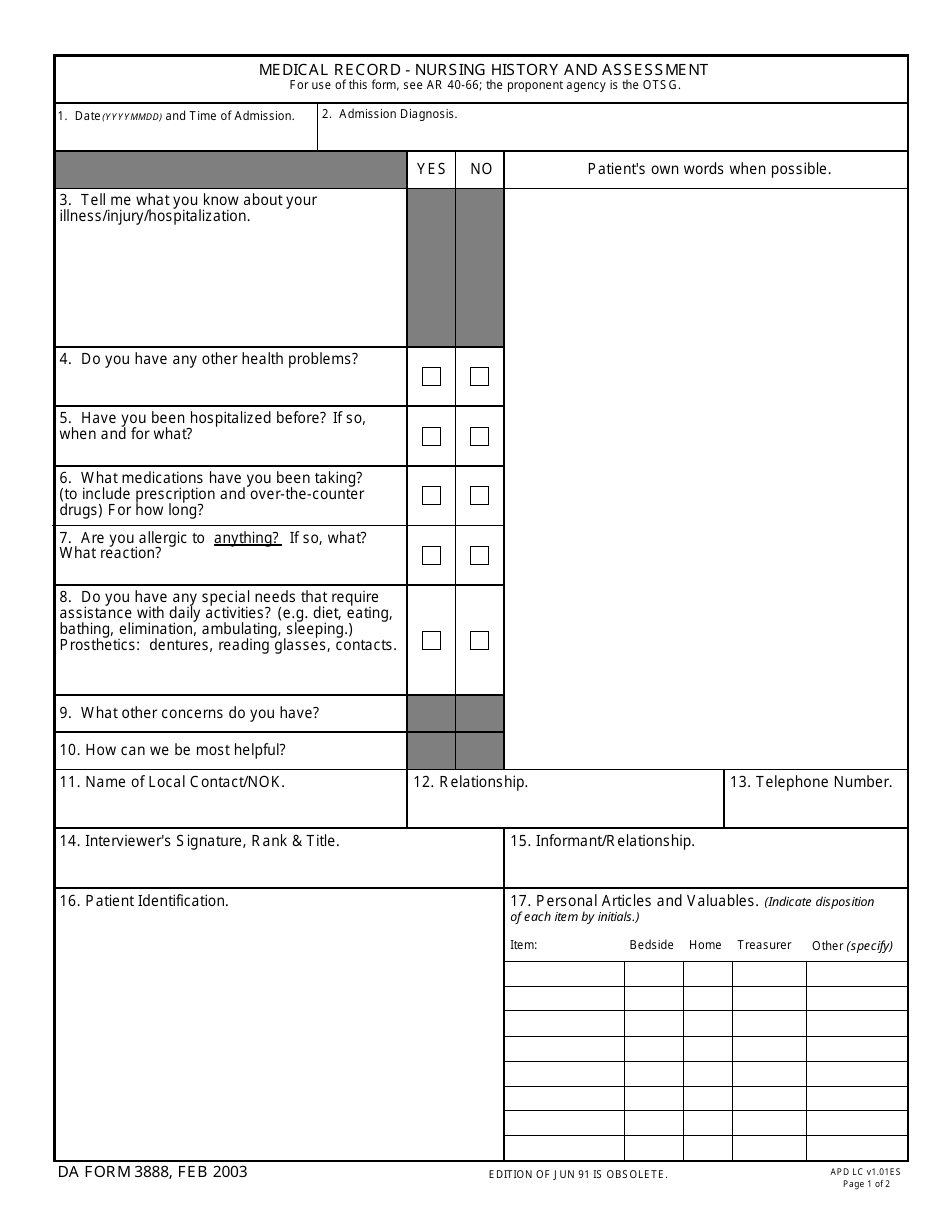
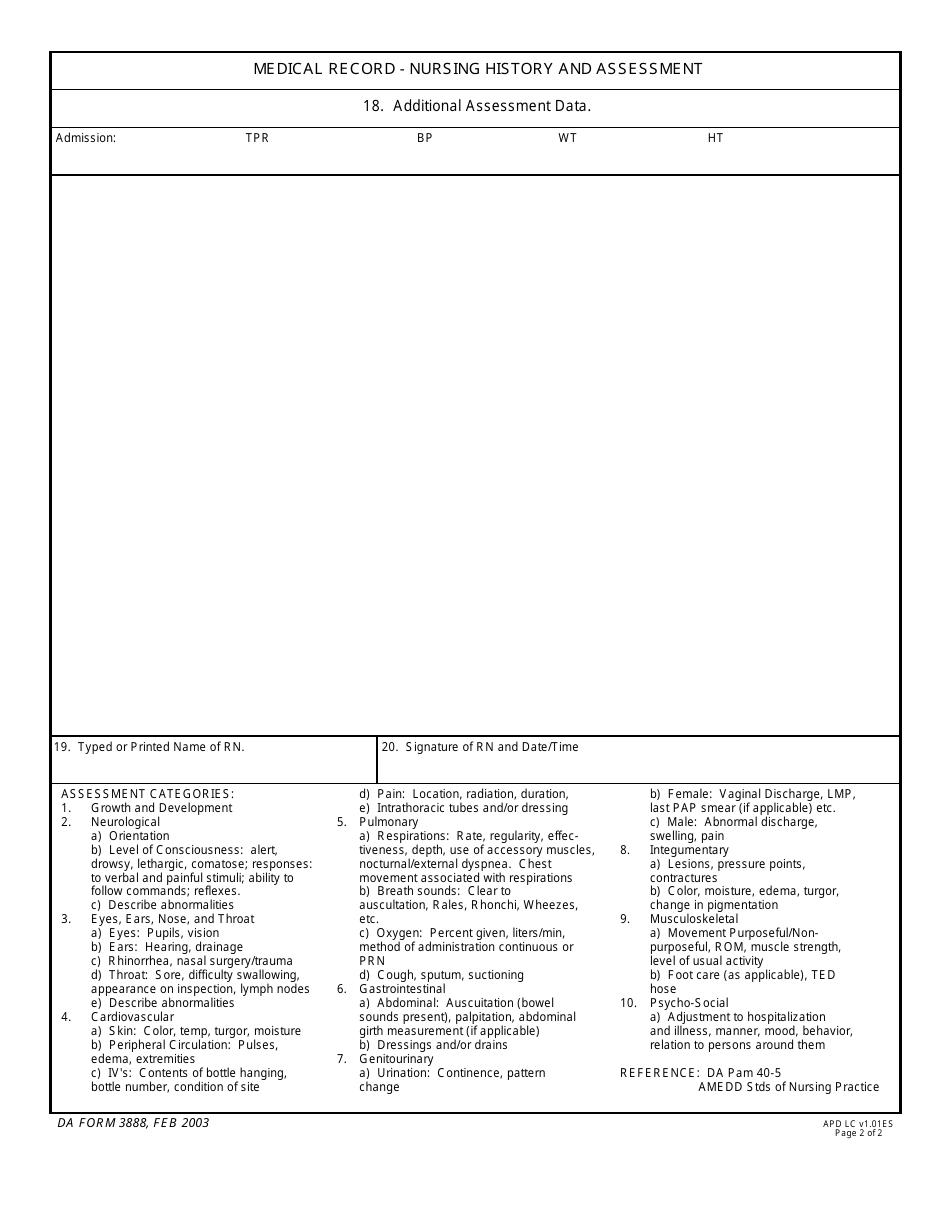
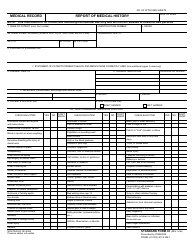
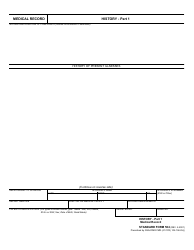
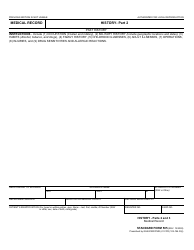
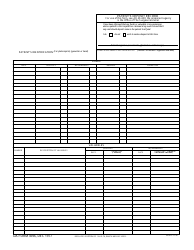
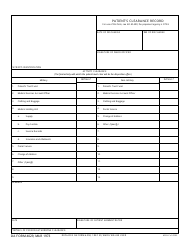
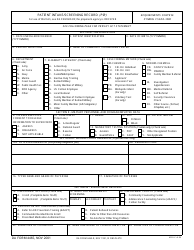
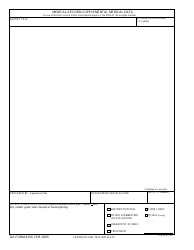
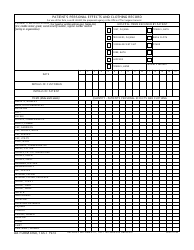
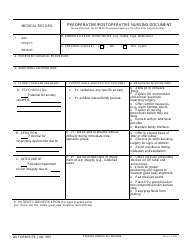
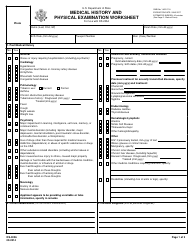
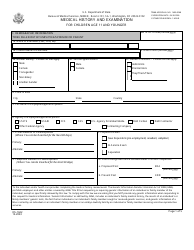
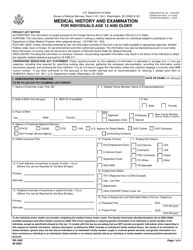
DA Form 3888 Medical Record - Nursing History and Assessment
What Is DA Form 3888?
This is a military form that was released by the U.S. Department of the Army (DA) on February 1, 2003. The form, often mistakenly referred to as the DD Form 3888, is a military form used by and within the U.S. Army. As of today, no separate instructions for the form are provided by the DA.
FAQ
Q: What is the DA Form 3888?
A: The DA Form 3888 is a medical record form specifically used for nursing history and assessment.
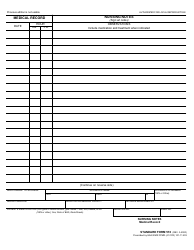
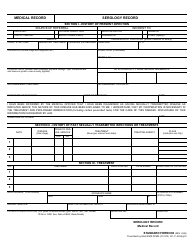
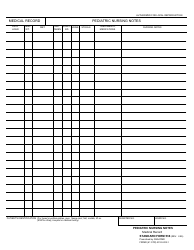
Q: What does the DA Form 3888 include?
A: The DA Form 3888 includes information such as patient's demographic details, medical history, nursing assessments, and interventions.
Q: Who uses the DA Form 3888?
A: The DA Form 3888 is mainly used by healthcare professionals, specifically nurses, to document a patient's nursing history and assessment.
Q: Why is the DA Form 3888 important?
A: The DA Form 3888 is important as it helps healthcare providers maintain a comprehensive record of a patient's nursing history and assessment, which can aid in providing appropriate and effective care.
Form Details:
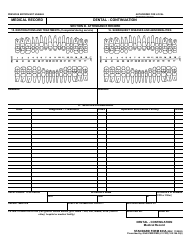
- A 2-page document available for download in PDF;
- The latest version available from the Army Publishing Directorate;
- Editable, free, and easy to use;
- Fill out the form in our online filing application.
Download an up-to-date fillable DA Form 3888 down below in PDF format or browse hundreds of other DA Forms stored in our online database.