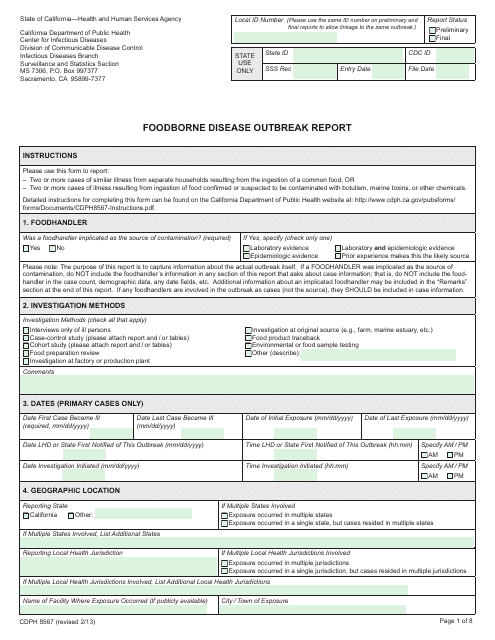
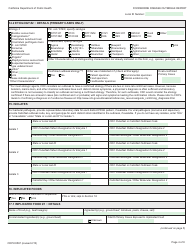
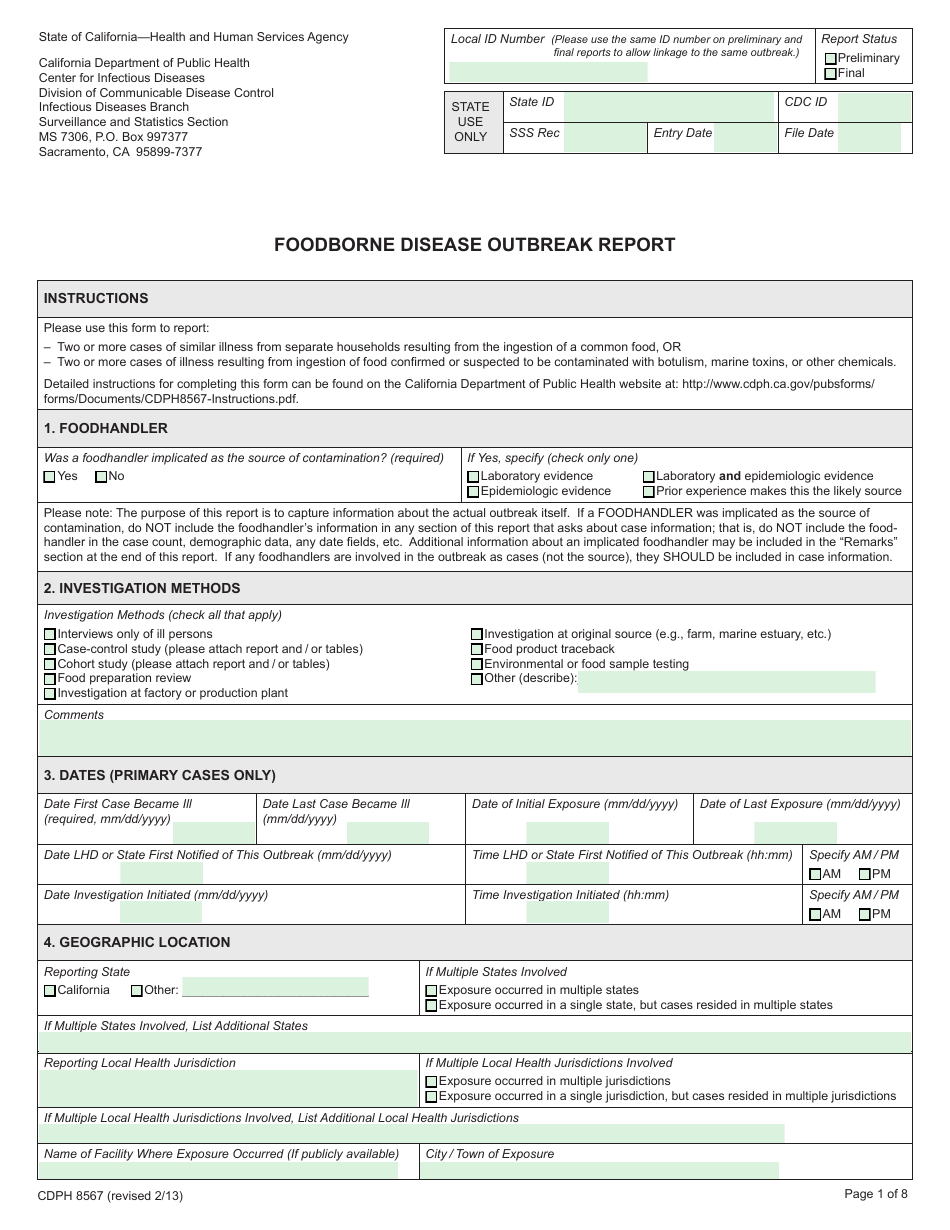
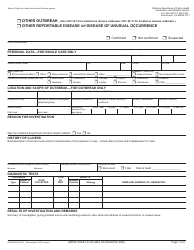
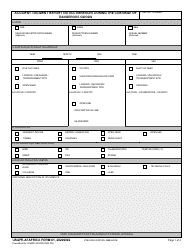
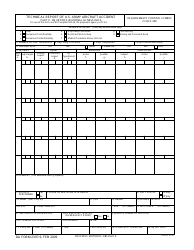
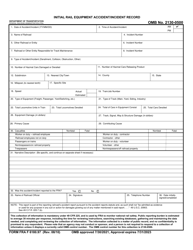
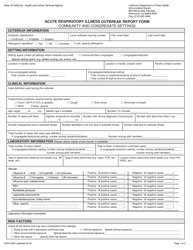
Form CDPH8567 Foodborne Disease Outbreak Report - California
What Is Form CDPH8567?
This is a legal form that was released by the California Department of Public Health - a government authority operating within California. Check the official instructions before completing and submitting the form.
FAQ
Q: What is the CDPH8567 Foodborne Disease Outbreak Report?
A: The CDPH8567 Foodborne Disease Outbreak Report is a form used to report foodborne disease outbreaks in California.
Q: Who uses the CDPH8567 Foodborne Disease Outbreak Report?
A: Public health officials, healthcare providers, and laboratories use the CDPH8567 Foodborne Disease Outbreak Report to report outbreaks.
Q: Why is it important to report foodborne disease outbreaks?
A: Reporting foodborne disease outbreaks helps public health officials investigate and prevent the spread of illnesses associated with contaminated food.
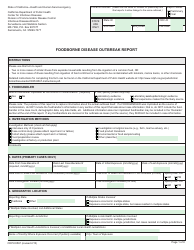
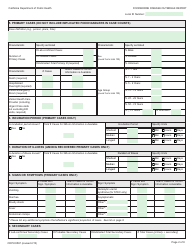
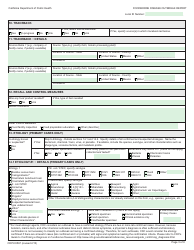
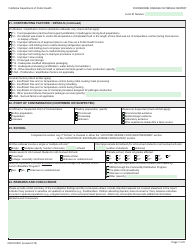
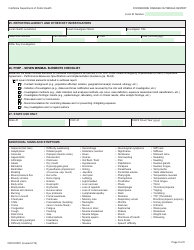
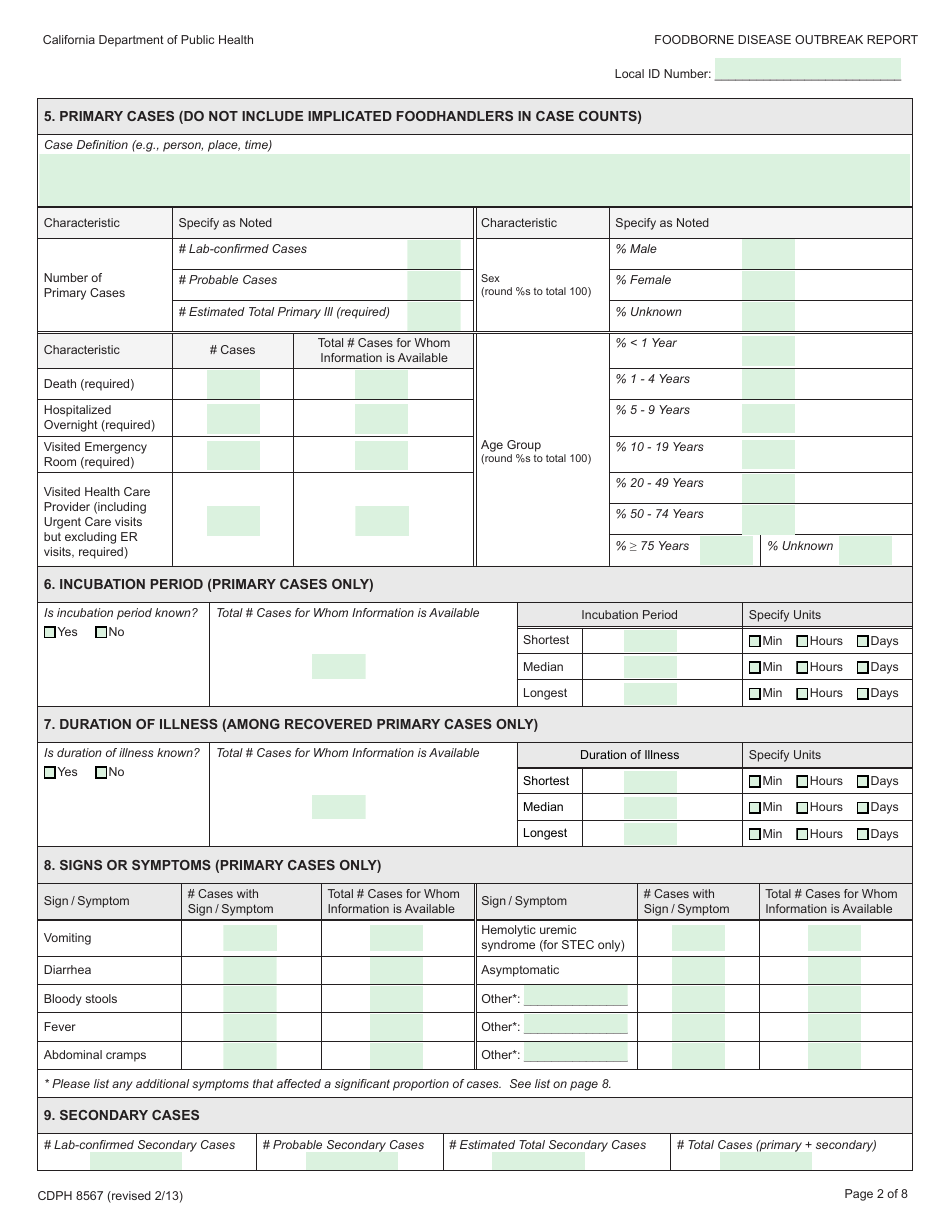
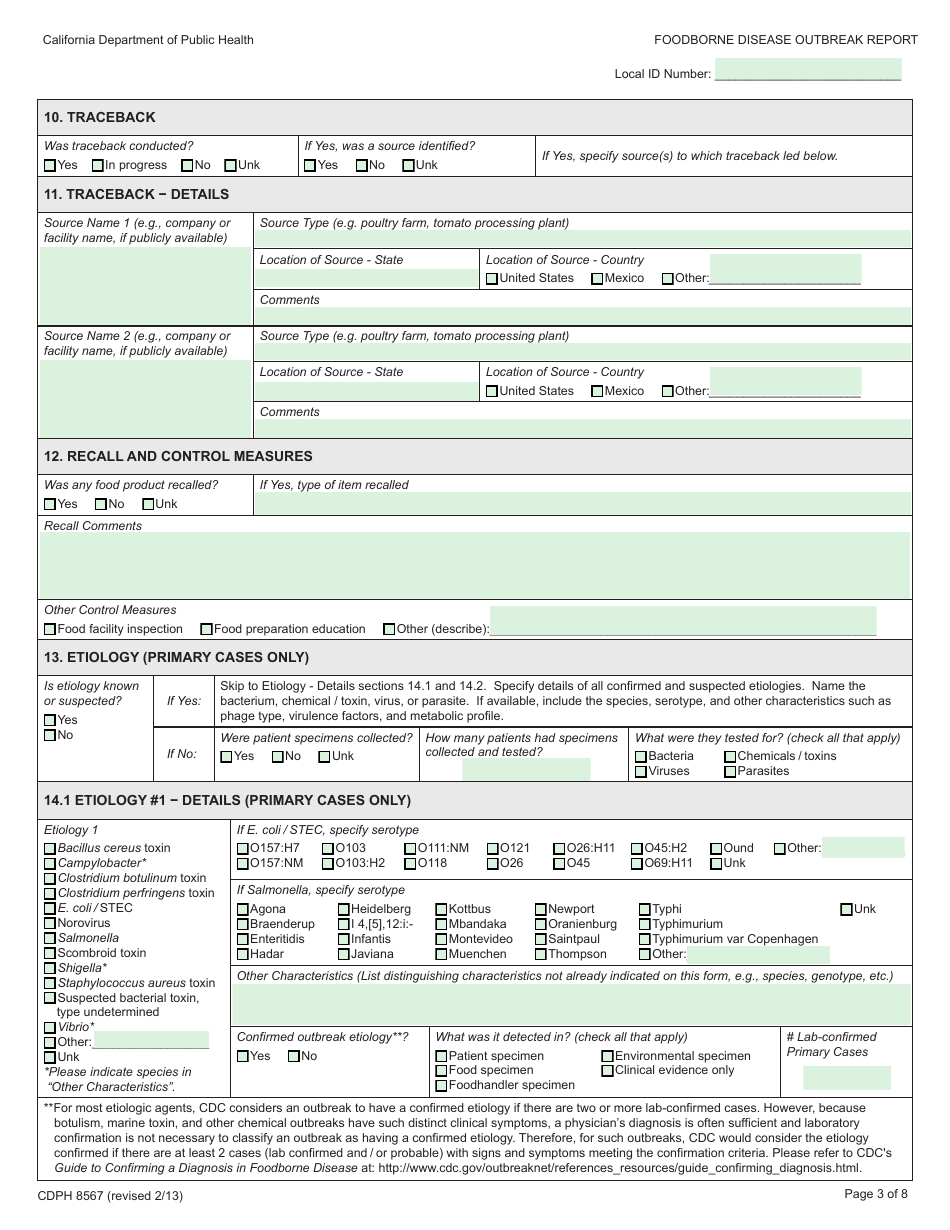
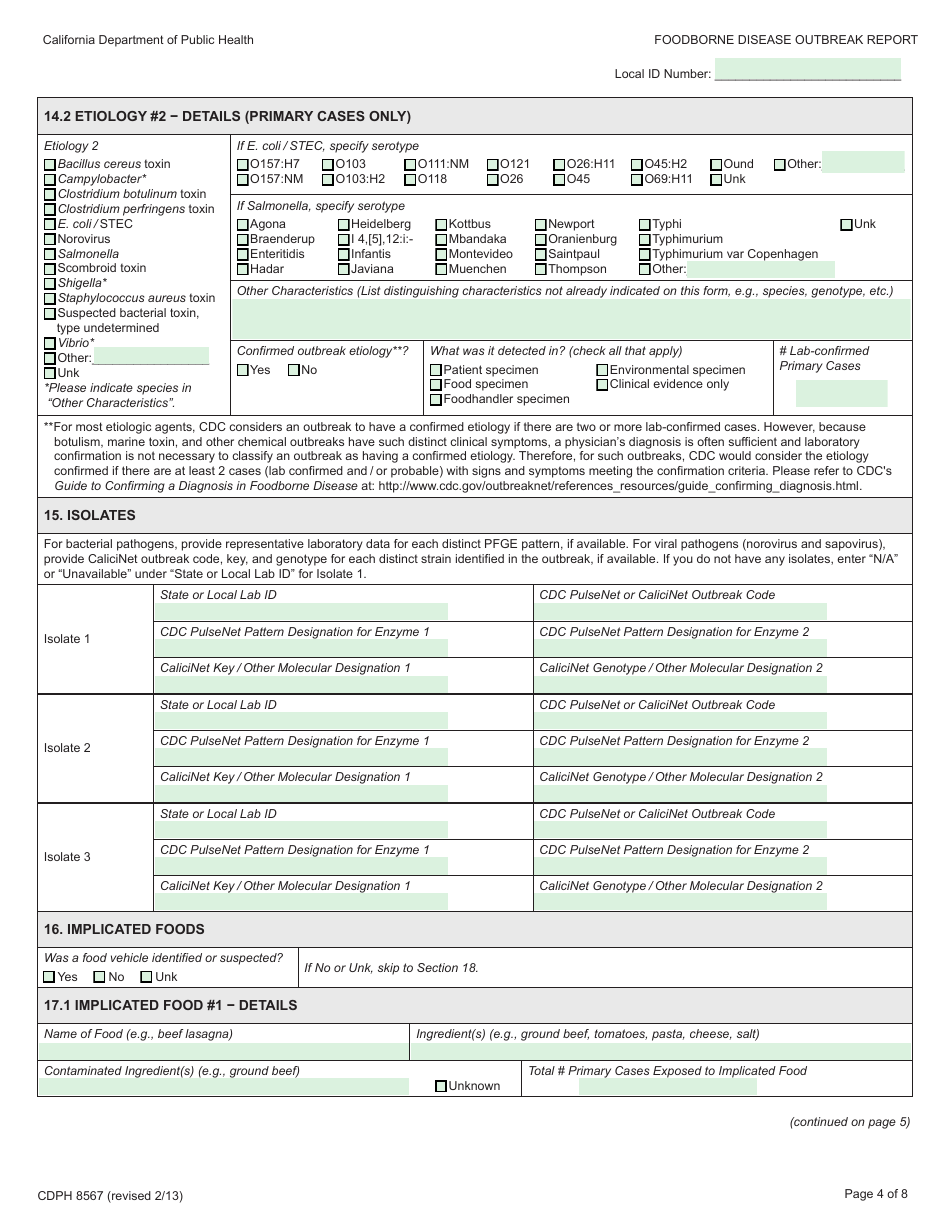
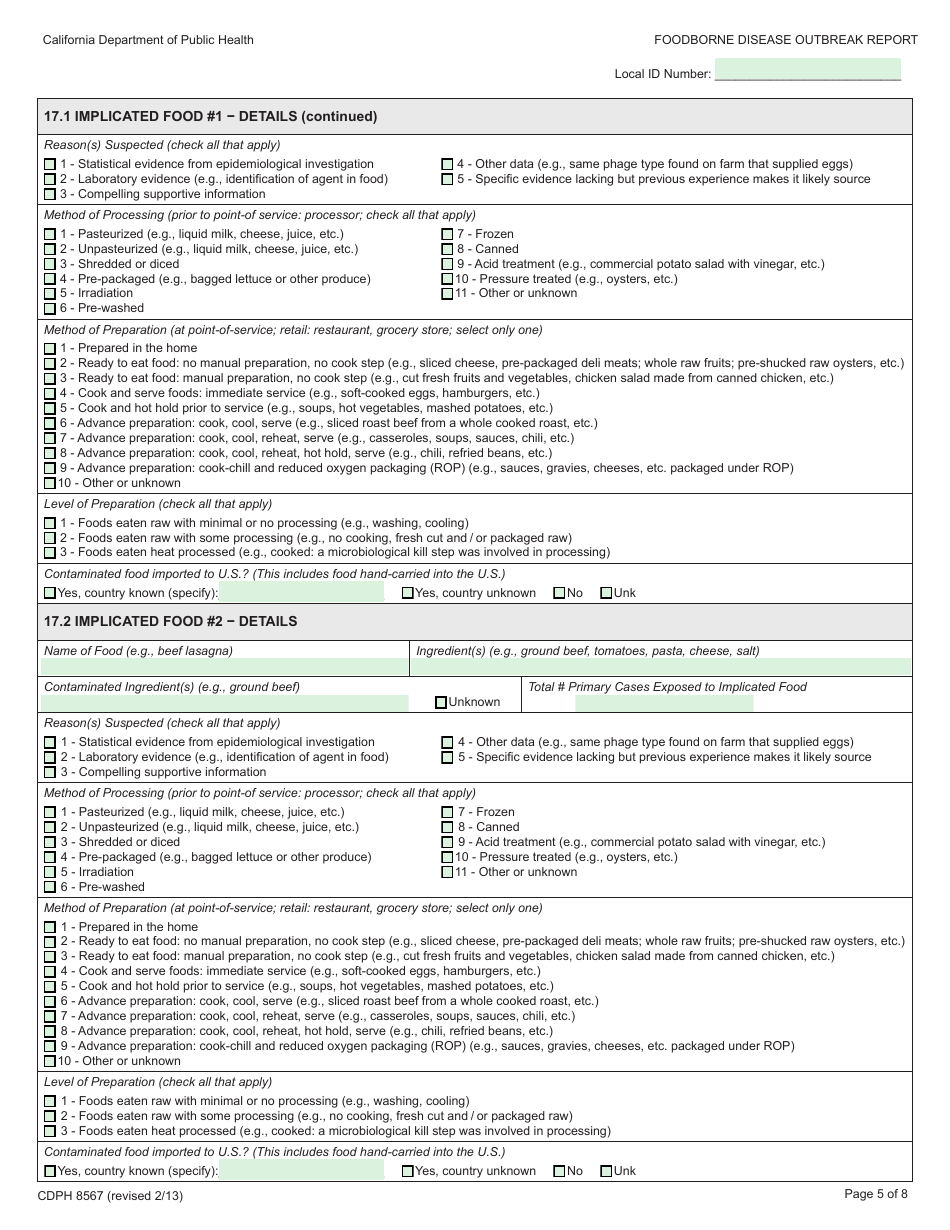
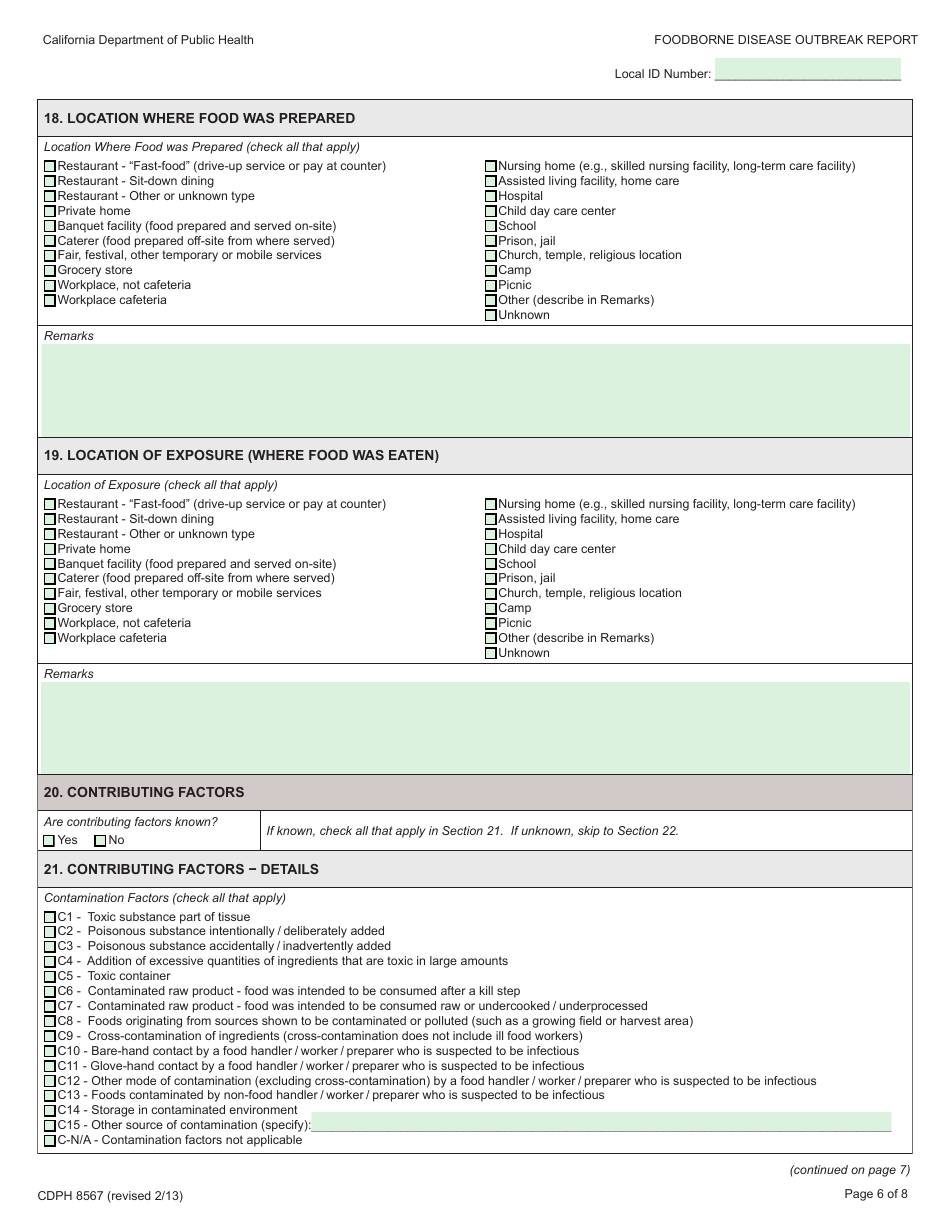
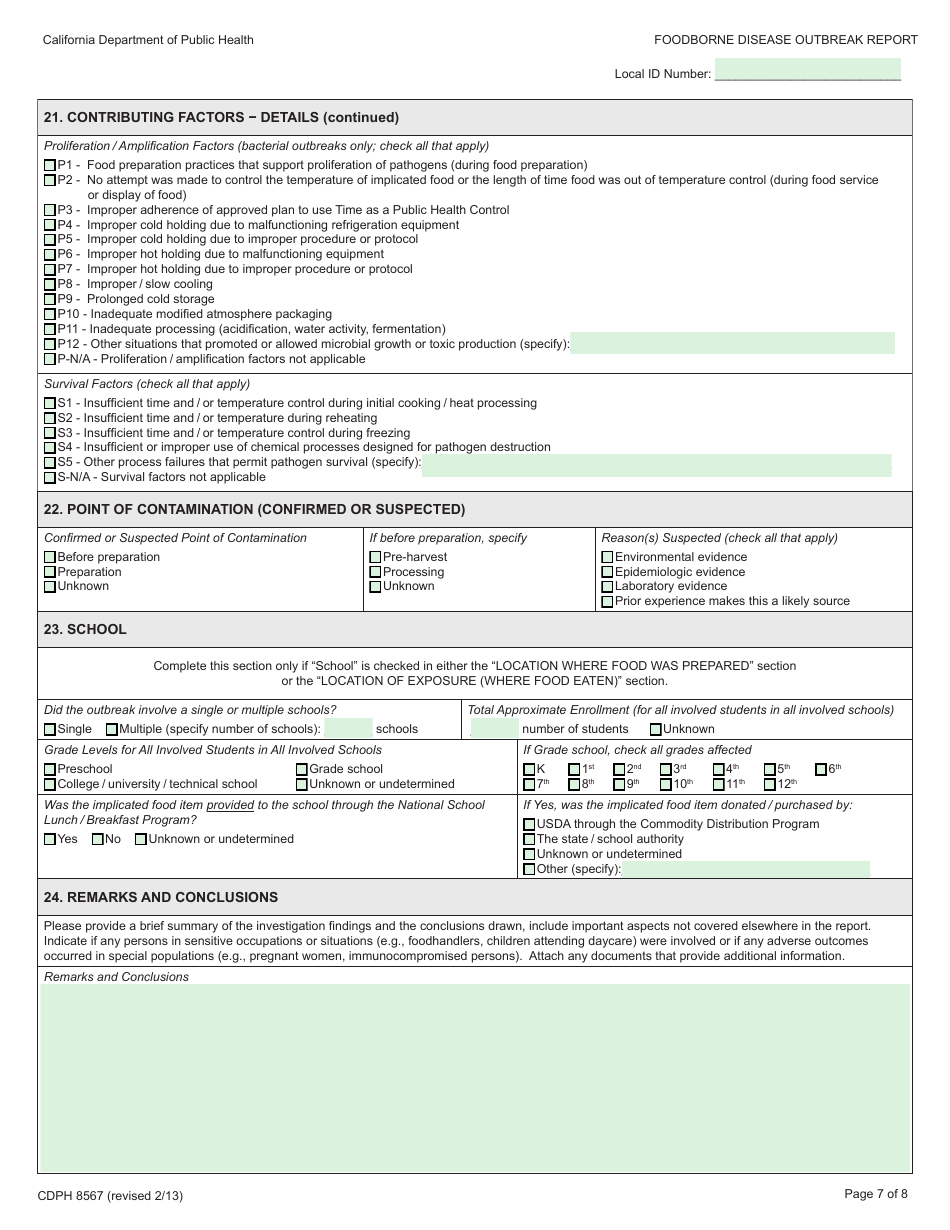
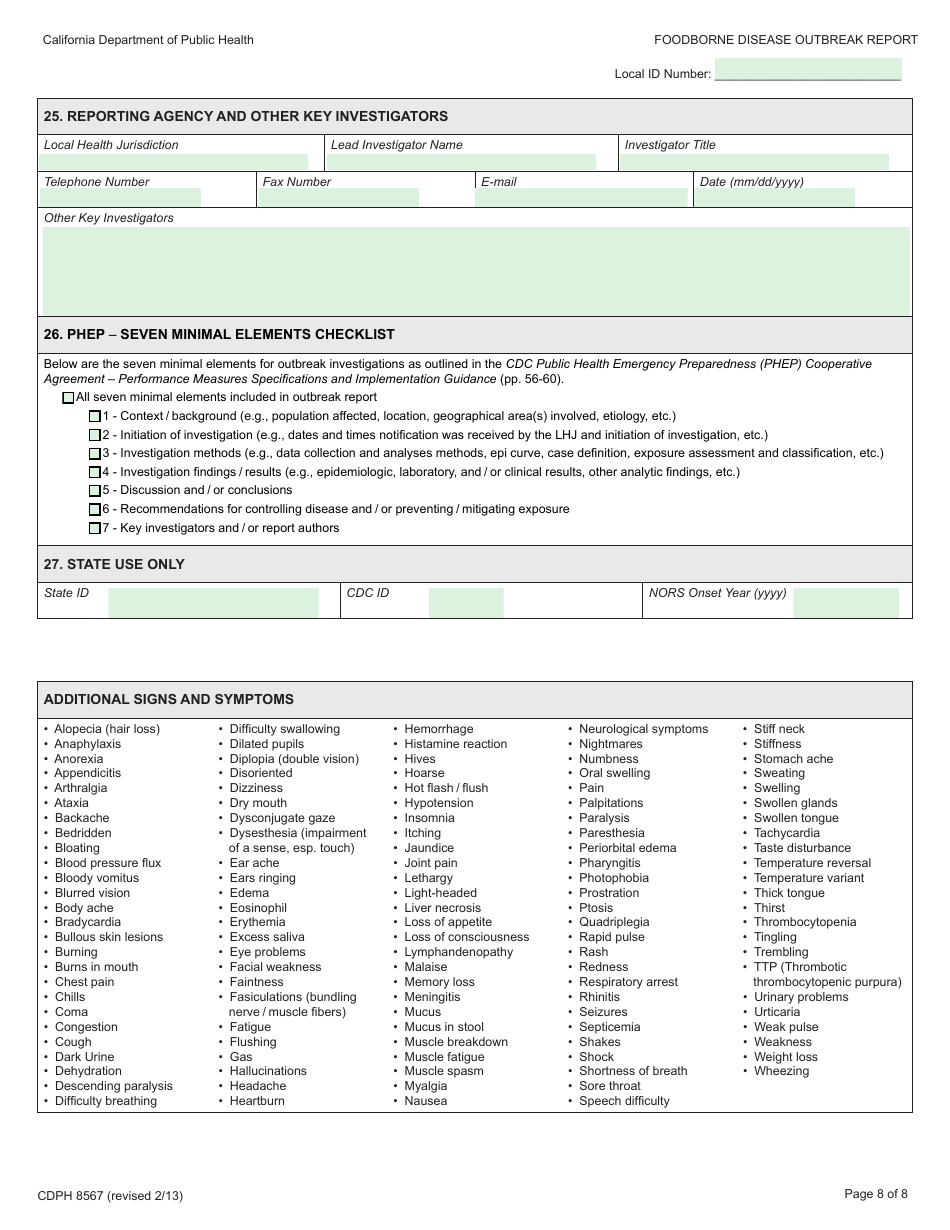
Q: What information is included in the CDPH8567 Foodborne Disease Outbreak Report?
A: The report includes information about the suspected food source, number of cases and hospitalizations, symptoms, and laboratory testing results.
Q: How should I submit a CDPH8567 Foodborne Disease Outbreak Report?
A: The report should be submitted to the local public health department or the California Department of Public Health using the specified reporting channels.
Q: What happens after a CDPH8567 Foodborne Disease Outbreak Report is submitted?
A: Public health officials will review the report, conduct further investigations if needed, and take necessary actions to prevent the spread of the disease.
Q: Can I submit a CDPH8567 Foodborne Disease Outbreak Report anonymously?
A: Yes, you can choose to submit the report anonymously, but providing your contact information may help public health officials gather additional information if needed.
Q: Are there any legal requirements to report foodborne disease outbreaks?
A: Yes, there are legal requirements in California to report foodborne disease outbreaks to local public health departments for investigation and control measures.
Q: How long does it take to receive a response after submitting a CDPH8567 Foodborne Disease Outbreak Report?
A: The response time may vary depending on the severity and complexity of the outbreak, but public health officials strive to provide timely responses.
Q: Can individuals report suspected foodborne illness without using the CDPH8567 Foodborne Disease Outbreak Report?
A: Yes, individuals can directly contact their local public health department to report suspected foodborne illnesses even if they are not part of a larger outbreak.
Form Details:
- Released on February 1, 2013;
- The latest edition provided by the California Department of Public Health;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form CDPH8567 by clicking the link below or browse more documents and templates provided by the California Department of Public Health.